Causes
- Poor nutrition. The child's body is very sensitive to food, since the stomach and other important organs that take part in digestion are not yet fully formed and are not ready for heavy loads.
- Thus, a child’s consumption of very fatty and fried foods can lead to the development of this disease. Parents do not always adhere to special diets and feed their daughters and sons exclusively steamed and boiled food. Most are of the opinion that after a year the baby can eat from the “common” table. This is a big mistake, since the baby’s body is not ready for such stress.
- Problems with the digestive organs. Very often, biliary dyskinesia accompanies diseases such as gastritis, pancreatitis, etc.
- Hepatitis. Today many children are carriers of this virus.
- Worms. As a rule, worms cause great damage to the child’s body, as they take all the necessary nutrients. And besides, due to its destructive actions, problems with the gallbladder may begin.
- Intestinal infection. When some kind of stick enters the baby’s body, it immediately develops, thereby provoking the appearance of symptoms such as nausea, weakness, and vomiting. The main symptom of intestinal infections is intoxication of the body, due to which the baby can suffer greatly. And an intestinal infection can provoke the development of complications, which, as a rule, are much more serious than the initial problem
- Problems with hormones. Often in childhood, hormonal disorders may appear, which are provoked by many factors. And because of such disorders, the likelihood that biliary dyskinesia may occur increases
- Nervous system disorders. The child’s nervous system is very vulnerable, and any emotional stress can provoke the development of problems that can later cause the development of other diseases.
- Physical exercise. Almost all pediatricians say that children should never be overloaded, especially physically, since their body is not designed and not ready for such stress.
- Fast growth. Sometimes the cause of the development of biliary dyskinesia can be the rapid growth of a child. This usually happens after 10 years, when the transition period begins. This happens most often in boys, because in 2-3 years they grow up and become about the same height as their parents. But the body does not always have time to adapt to such a change.
- Allergic reaction. Many people think that allergies are not scary, and they do not cause much harm to the body. But this is a serious misconception, since it can manifest itself in different ways, and it happens that the cause of simple peeling of the skin may not be a lack of water in the body, but an allergy. It is worth knowing that it all starts with the intestines, and often allergens penetrate other organs, provoking the development of serious complications. And, as a rule, parents do not pay attention to mild manifestations, although it is at this moment that unpleasant consequences can be prevented
- Congenital gallbladder defects
Symptoms
- Pain in the liver area. It can be either aching or paroxysmal in nature. It all depends. How serious is the damage? Usually the pain appears an hour after eating. If a child has eaten a lot, and the food was quite fatty, then the pain attack will be much stronger than if he ate something more healthy and less harmful. In addition, severe pain can radiate to nearby organs, thereby causing even greater discomfort to the child.
- Nausea and sometimes vomiting. This happens as a result of a severe pain attack
- Abnormal stool. This can be either loose stools or, on the contrary, constipation. It all depends on individual characteristics and reaction to such a problem.
- Decreased blood pressure
- Rapid pulse, that is, palpitations that occur mainly during an attack of pain
- Sleep problems. Very often, children with this disease find it difficult to put them to sleep because they are constantly in pain. And they don't sleep very well
- Increased sweating, which can occur either during an attack of pain or simply during the day
- Headache
- In addition to the above symptoms, when examined by a doctor, the child will complain of pain in the right precostal area when he touches this place. It should be noted that with such symptoms, there will be no increase in body temperature.
- Hypokinetic form. The manifestations of this form are slightly different from the hyperkinetic one, since the pain usually does not spread to other organs and does not manifest itself as acutely. Usually, the child complains of unpleasant pain in the liver area (points to this place with a pen). Often, when experiencing stress or some other strong emotions, the pain may noticeably intensify and a feeling of pressure will appear in the area of the gallbladder.
- Lack of appetite, and the child may not pay attention even to what he likes so much, for example, not wanting candy or a banana
- Belching
- Bitter taste in mouth
- Nausea, which can be mild or very severe
- Problems with bowel movements, most often constipation
- Flatulence, which may cause the child to complain of abdominal pain
Acute cholecystitis
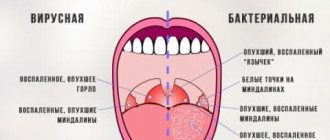
Inflammation of the mucous membrane occurs when infectious agents enter it (hematogenously or lymphogenously), which most often are Escherichia coli or staphylococci.
Concomitant cholelithiasis and structural anomalies contribute to the occurrence of cholecystitis. Young patients with acute inflammation complain of:
- intense pain in the upper abdomen;
- discomfort, heaviness in the right half of the abdomen;
- belching, nausea, vomiting;
- fever up to 37.5 degrees;
- general weakness, malaise.
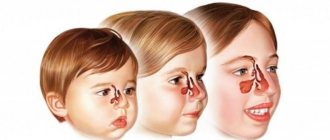
Features of the manifestation of symptoms of the disease in children
- A lot at one time. This happens when there is no systemic nutrition, but only snacks.
- Large amounts of food, overfeeding the baby. This happens to those children whose parents are manic about portion sizes and believe that a child should eat almost the same amount as an adult. And he shouldn’t refuse food
- Fast food. Everyone knows that fast food is the most unhealthy food there can be. Such dishes are prepared in a huge amount of vegetable oil, making the product dangerous to the health of the child.
Diagnostics
- Ultrasound examination of the gallbladder. During this procedure, the doctor completely studies the structure of the bladder, its ducts, records the dimensions, considers whether there are any congenital defects that can cause pain, etc. All results are recorded and sent directly to the attending physician
- Ultrasound examination before and after breakfast. If any abnormalities were noticed on the initial ultrasound, the doctor will have to conduct the following study: the child is given an ultrasound before he has breakfast. Then, the child is given something to eat, fatty food at that, and after half an hour or forty minutes another ultrasound examination is performed. During it, you will see how much the bladder will shrink, and what form of the disease is present in the baby
- Duodenal sounding. To conduct this study, you need to prepare the child well, as it takes quite a long time, and the procedure is very unpleasant. So, a probe is inserted into the duodenum, with the help of which bile is examined. For this, several samples are taken. True, this method is used very rarely today, since it is rare that a child will be able to withstand this procedure
- X-ray. This study is not done for all children, but only for those who, based on the results of an ultrasound examination, were found to have congenital malformations of the gallbladder and its ducts
- Endoscopic retrograde cholangiopancreatography. This study is very serious and is carried out very rarely, only on special instructions from a specialist.
The role of pathology in the development of gallbladder diseases
The structure of the biliary zone, including the gallbladder and ducts, allows for a high degree of variability. Bends and folds are classified as minor pathologies. This condition is not a disease, but the abnormal structure increases the risk of impaired organ motility and the development of congestion. Treatment for bending of the gallbladder has not been developed, but there are methods to prevent possible complications.
The bend of the gallbladder can be congenital or acquired. The hereditary factor plays a major role in the spread of the anomaly. Often this structure is combined with an abnormal structure of the nerve endings and blood vessels of the organ. Congenital bending can be classified based on the location of changes and the shape of the gallbladder:
- hourglass shape;
- S-shape;
- Phrygian cap.
Deformation may be in the area of the bottom, body of the gallbladder. The most dangerous pathology of the structure of the cervix is the narrowest place where the folds of the mucous membrane, the sphincter of the cystic duct, are located. Injuries and obstructions in the patency of this zone lead to inflammation of the bladder, obstructive jaundice, and hepatic colic.
Acquired bending of the gallbladder is associated with chronic inflammation that affects the outer, serous membrane (pericholecystitis). In this case, the bubble has an unusual shape, angular protrusions, torsions, adhesions with neighboring organs, which cannot be classified. The medical history of such patients already includes chronic cholecystitis, and often cholelithiasis (GSD).
Anomalies of the gallbladder are classified as a genetic group of risk factors for cholelithiasis. Doctor of Medical Sciences E.Yu. Eremina in the article “Biliary pathologies: possibilities for prevention” identifies the stages of development of GB pathologies with an inflection:
- abnormal development of the same;
- biliary dysfunction, biliary dyskinesia;
- chronic acalculous cholecystitis;
- biliary sludge;
- cholelithiasis (GSD);
- cholecystectomy.
The final form of GB is determined by 12–14 years. Until this time, variations in structure are possible. In children, a spherical and S-shaped gallbladder is often found, as well as its kinks, connecting septa and constrictions inside the gallbladder cavity. If these changes affect the contractility of the organ, then there is a threat of the appearance of biliary sludge, thick putty-like bile with a solid sediment.
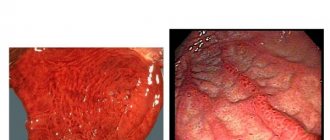
Thickening of tissues of more than 2 mm and their double-layeredness are signs of an inflammatory process. An ultrasound scan reveals biliary sludge. To monitor the functions of the organ, two studies are carried out: on an empty stomach and after breakfast, promoting the outflow of bile, in order to get an idea of the ability of the gallbladder to empty.
Treatment
- The baby needs to eat about 4 or 5 times a day and in small portions so that the load on the gallbladder is as little as possible
- The baby must be fed strictly at certain hours, and the break between feedings should always be the same (about 3 hours)
- It is best to steam it, or simply boil it. In addition, it is better to give preference to pureed food or well-chopped
- You need to exclude foods such as lard, fried foods, legumes, nuts, sweets, buns, sparkling water, etc.
- You need to include easily digestible carbohydrates in your diet, which can be obtained from marshmallows, marshmallows, and jam. As well as other products - sour cream, butter, cheese, not spicy, beets, carrots, all fresh fruits, as well as strawberries and raspberries
- Medicines that help relax smooth muscles. Usually this is No-shpa, Odeston
- Medicines that calm the nervous system. Usually it is valerian or motherwort
- Magnesium
- Only a doctor can prescribe this or that medicine, since they all have side effects and contraindications.
If a child has exacerbations rarely, and he is not bothered by pain, then the doctor may recommend drinking mineral water, such as Slavyanovskaya, Essentuki.
- Treatment of hypomotor form. For children who have this particular form of the disease, there are slightly different recommendations. So, you need to follow a daily routine, clearly alternating periods of wakefulness and sleep in order to calm the nervous system. Also, an active lifestyle is recommended, of course, without heavy loads.
- In this form, the tone is, on the contrary, reduced. And therefore, foods that will help increase it should prevail in the diet. So, it is better to eat milk, sour cream, and fruits.
Biliary dyskinesia is a rather unpleasant disease. But if it is detected in a timely manner, and all doctors’ recommendations are followed, it can be cured. True, you will need to spend a lot of time and effort on this!
Cholecystitis is a very common problem among the youngest population.
This is due to the fact that a variety of reasons lead to the development of the disease, in particular bacterial infections, which the child’s immature immune system cannot fully resist, helminthic diseases, which are also very common among children, as well as poor diet and sedentary lifestyle.
Thus, this pathology can occur both in children in the first years of life and at an older age. Age does not matter.
Cholecystitis in children is considered a very serious disease that negatively affects the quality of life of the baby, so the task of parents is to recognize the disease in the early stages of its development and begin treatment as soon as possible. Otherwise, very unpleasant and dangerous complications may develop.
How to treat biliary dyskinesia in children? Find out about this from our article.
How to remove sand and stones? Treatment methods
This pathology can be treated in the early stages using conservative methods (drug therapy (tablets and capsules) and treatment with folk remedies). In more advanced cases, when there are signs of acute or chronic calculous cholecystitis or there are large stones in the bladder that can block the bile duct, surgical intervention techniques are used.
If flakes are detected in a timely manner in the gallbladder, surgery is usually not required, and therapy is limited to medicinal methods of therapy. However, if the patient begins to be bothered by constant severe pain or a formed stone blocks the lumen of the bile duct, a cholecystectomy (surgery to remove the gallbladder) may be prescribed.
If the symptoms do not bother the patient much or their manifestation is periodic, then doctors recommend a set of measures, including following a special diet (“Treatment Table No. 5”), treatment with choleretic drugs and folk remedies. The pain syndrome is well relieved by various antispasmodic drugs (tablets “No-shpy”, “Mebeverine”, “Duspatolin” and so on).
In addition, you can use folk remedies as additional therapy. The use of traditional medicine recipes is not only an effective method of complementary therapy, but can also serve as an excellent preventative measure for this pathology.
As a rule, folk recipes for the treatment of biliary sludge, which causes the formation of gallstones, are various infusions and decoctions based on medicinal plants or their preparations, which have an anti-inflammatory and choleretic effect on the body. A folk remedy involves a fairly long treatment, consisting of several long (from two to three months) courses of taking medications at certain intervals (most often, two courses per year).
There are a great many recipes that remove sand and small stones from the body, and it is simply impractical to list them all. Herbal treatment involves the use of herbs from which infusions and decoctions are prepared. Such collections may include rose hips, strawberry leaves, corn silk, beet juice, black radish juice, dill seeds, wormwood, St. John's wort, milk thistle, immortelle, yarrow and many, many other useful natural ingredients.
When taken on a regular course according to the regimen prescribed by the doctor, these medications can not only significantly reduce the amount of harmful suspended matter, but even help to completely get rid of its presence by being naturally removed from the bladder through the bile ducts.
Its main principle is based on fractional nutrition, which implies frequent (five to seven times a day) intake of small (up to 300 grams) portions of food at regular intervals. Such a therapeutic diet requires giving up fatty, spicy, fried, smoked, pickled and pickled foods, as well as limiting the consumption of sweets, baked goods, sour fruits and berries and other foods that irritate the digestive system.
Alcohol and carbonated drinks should be completely avoided. It is recommended to consume lean meat (veal, chicken, rabbit and turkey), cottage cheese, fermented milk products, virgin vegetable oils, cereal porridges and soups in vegetable broth, as well as sweet fruits and berries, fresh and boiled vegetables and other dietary products.
Concept and characteristics
Cholecystitis is an inflammatory disease affecting the gallbladder area. This organ is important in the digestion process, as it produces bile containing digestive enzymes.
Inflammation in the gallbladder disrupts the functionality of the organ, and therefore the entire digestive process is disrupted, which leads to the development of characteristic symptoms of the disease.
Proper nutrition, digestion of food and absorption of nutrients is a prerequisite for the proper development of the child’s body.
Violation of this process leads to very undesirable consequences, such as developmental delays, intoxication of the body, pain, which significantly reduces the quality of life.
However, a localized form is rare, in which the inflammatory process affects only the gallbladder. Much more often, the source of inflammation spreads to the area of the biliary tract and liver.
Methods for removing stones from the gallbladder
When gallstones have grown to large sizes, such a diagnosis cannot be avoided without surgical intervention. Modern medicine offers options for removing stones from the body that are painless and provide more guarantees that the stones will not form again. Surgical intervention is performed according to certain indications. Today, doctors perform classic abdominal surgeries, laparoscopy, and crushing stones with ultrasound.
Operation
The presence of stones is not considered a reason for surgery. The surgeon prescribes it only when there are specific clinical symptoms: biliary colic, aching, dull pain, heaviness under the ribs on the right, frequent belching, bitter taste in the mouth, heartburn. Standard surgery (cholecystectomy) is often performed for emergency reasons. General anesthesia is performed. The patient's gallbladder is removed, and if necessary, the ducts are drained. The wound is sutured, a drainage is placed to the bladder bed.
Laparoscopy
Recently, stones are often removed by laparoscopy. The stones are removed using trocars, special metal conductors inserted into the peritoneum. The abdominal cavity is filled with carbon dioxide, and a tube from a device is inserted into the incision, which will transmit the image to the monitor. The doctor pulls out the stones and installs staples on the vessels and ducts of the gallbladder. Indications for surgery: calculous cholecystitis.
Ultrasonic stone crushing
Gallstone diseases are sometimes the reason for referral for ultrasonic crushing of stones (lithotripsy). Ultrasound destroys stones, breaking them into small particles (no more than 3 mm). Small pieces exit into the duodenum through the bile ducts. This type of operation is suitable for those patients who have a small number of large cholesterol stones (up to 4-5 pieces).
Causes and risk factors
The main causes of the occurrence and development of cholecystitis in a child are bacterial infections (the causative agent can be different, most often these are staphylococci and streptococci), the presence of chronic foci of infection in the body (for example, advanced caries), as well as helminthic and parasitic diseases (for example, giardiasis ).
However, these reasons are far from the only ones. So, there are a large number of other risk factors, the presence of which can lead to the development of gallbladder pathology:
- Poor nutrition. In particular, violation of the eating pattern (long breaks between meals, leading to stagnant processes in the gallbladder), consumption of large amounts of foods rich in carbohydrates, rare consumption of vegetables and fruits rich in fiber, overeating.
- Sedentary lifestyle.
- Structural anomalies or injuries of the biliary tract that disrupt the process of outflow of produced bile.
- Diseases of the endocrine system (for example, diabetes, obesity).
- Frequent stress, associated, for example, with a sharp change in daily routine, living conditions, and unfavorable family conditions.
- Allergic reactions to food.
- Intoxication of the body, including food poisoning.
- Diseases of the autonomic nervous system.
- Persistent disruption of the immune system.
What is an anechoic formation?
This is the name of a formation in the gallbladder that does not allow sound to pass through and is not an independent diagnosis. The gallbladder has a homogeneous structure, and areas of increased echogenicity look like a dark spot on ultrasound results. An anechoic formation is indicated in the doctor’s report if he is unable to make out what he sees on the monitor screen. The therapist or attending physician who sent you for this study will figure out what exactly is inside. Often, next to the concept of anechoic in parentheses, the ultrasound specialist indicates options for possible contents, but does not make diagnoses.
Sound-proof inclusion can be:
- Large blood vessels.
- Capsules containing liquid are avascular neoplasms.
- Neoplasms - benign and malignant tumors.
There is no need to be scared when you see the words anechoic contents of the gallbladder in the ultrasound results; you need to figure out what it is. This means that a liquid inclusion or solid inclusions of echogenic rock are visible in the lumen of the gallbladder.
The dysfunctions contained in the organ are divided into focal neoplasms and diffuse changes. Focal ones include stones, sand, tumors, cholesterosis, fibroids of various sizes, fibromas or adenomas.
Diffuse usually includes the presence of purulent spots, sediments of various etiologies and blood. Often diffuse changes appear after an accident, fall or other abdominal injury. Purulent bile is a fairly rare phenomenon, but no less dangerous than perforation. Blood usually appears after a severe injury; at first, massive bleeding looks like a homogeneous mass on the picture. But after a while, the blood coagulates inside, and on ultrasound it looks like clots, increasing the number of adhesions and dark spots that do not allow sound to pass through.
Symptoms and signs of pathology
Characteristic signs of the development of cholecystitis are the following symptoms :
- Bitter taste in the mouth, which is most pronounced after sleep or prolonged fasting.
- Loss of appetite.
- The appearance of vomiting.
- Stool disorders (diarrhea, constipation, or their alternation).
- Acute attacks of pain localized in the area of the right rib.
The clinical picture of the disease can be supplemented by such signs as:
- An increase in the size of the liver and pain in this organ when pressing on it.
- Pain in the gallbladder area.
- Consolidation of the anterior abdominal wall, its tension during exposure.
- Persistent hyperthermia (antipyretics have a short-term effect).
- Leukocytosis, increased ESR in the blood, indicating the presence of an inflammatory reaction.
- Symptoms of jaundice (extremely rare).
- Disturbances in the functioning of other organs and systems (cardiovascular, endocrine, respiratory).
Diagnostics
To identify the disease, the doctor examines and interviews the patient. However, since the disease can have a hidden course, this data is not always enough to determine a detailed picture.
Therefore, additional laboratory and instrumental diagnostic , including:
- blood test for the level of leukocytes and ESR (with cholecystitis, these indicators are increased);
- blood test for enzymes (sialic acid, transaminase, alkaline phosphatase);
- echography of the gallbladder to determine its size and condition of the walls;
- laboratory examination of bile.
Diagnostic methods
Making a diagnosis begins with an initial examination and collection of anamnesis, on the basis of which the doctor decides to prescribe certain diagnostic tests. Since many gallbladder diseases have similar symptoms, such studies cannot be avoided.
Ultrasound of the abdominal organs
Based on primary data, the doctor can prescribe the following instrumental and laboratory examinations (in combination and separately):
| № | Helpful information |
| 1 | biochemical and general blood tests |
| 2 | Ultrasound of the abdominal organs |
| 3 | urine and stool tests |
| 4 | duodenal intubation |
| 5 | computed tomography (CT) |
| 6 | magnetic resonance cholecystography (MRI) |
Treatment options
Only complex therapy , including drug treatment, the use of herbal preparations, traditional medicine, and adherence to a proper diet, will help eliminate the causes and manifestations of cholecystitis.
Medications
Therapy of the pathology is impossible without taking of medications :
- Antibiotics (if the cause of the disease is a bacterial infection).
- Antihelminthic drugs (for helminthic infestations).
- Painkillers for severe pain.
- Antispasmodics that normalize the functioning of the affected organ.
- Drugs that promote proper flow of bile.
- Symptomatic drugs prescribed for damage to other organs.
Phytotherapy
A positive therapeutic effect is provided by the use of various herbal decoctions, which help normalize the production and outflow of bile and eliminate the inflammatory process.
Decoctions are prepared from plants such as strawberries, anise, rose hips, birch buds, yarrow flowers, mullein, elecampane root, burnet, chicory, and hop cones.
The course of treatment varies in duration depending on the form of the disease. Thus, in the chronic form, long-term use of herbal medicines is recommended (up to 10-12 months), but recommendations in each specific case are determined by the doctor.
Traditional medicine
In the fight against the manifestations of the disease, time-tested folk recipes also provide effective assistance, such as:
- Rowan juice. To prepare it, juice is squeezed out of ripe rowan fruits, which must be taken in 50-100 ml doses. 3 times a day half an hour before meals.
- Salt and lemon . The juice obtained from 1 lemon is mixed with 1 liter. boiled water, add 1 tbsp. salt. The resulting solution is taken once a day on an empty stomach in the amount of 1 glass. The duration of treatment is 7-10 days.
- Juice mixture. You need to take 3 parts lemon juice and 1 part each cucumber, beetroot, and carrot juice. The resulting product is taken 2 times a day, 0.5 cups.
Diet therapy
Diet is an important step in the treatment of cholecystitis.
So, from the child’s diet it is necessary to exclude fatty, fried, spicy, pickled foods, foods that are difficult to digest.
It is recommended to consume dairy products (low-fat), boiled or steamed fruits and vegetables, lean meat and fish.
It is important to remember that dishes should be crushed as much as possible, preferably in the form of purees. It is better to avoid eating solid foods.
What can children take?
If you have been prescribed a choleretic drug for children, you should understand what exactly this medicine is and how it works.
A choleretic drug is a drug that helps the formation of bile and its further excretion into the intestines. They can be plant-based, animal protein-based, or synthesized.
Special requirements are imposed on “children’s” choleretic drugs. It is desirable that the drug be in the form of a suspension or syrup. This will make it easier for the child to accept it. But the main thing is that the drug is plant-based. Then it will have much fewer side effects than synthetic choleretic drugs.
Medications
Let's consider the most popular gallstones suitable for children:
Holaflux is a choleretic drug, usually prescribed for chronic cholecystitis and dyskinesia of the bladder and biliary tract. A herbal preparation containing dandelion, thistle, celandine, etc. The medicine facilitates the outflow of bile. The instructions for use say that no side effects were found, so this drug is often prescribed to children. Available in the form of a dry herbal mixture for making choleretic tea.
Folk remedies
In addition to pharmaceutical drugs, diseases of the gallbladder and its ducts can also be treated using traditional methods. The best fighters against bile stagnation are considered to be birch buds, corn silk, rowan fruits, burdock roots, and rose hips. There are several ways to prepare drugs with a choleretic effect:
- Choleretic juices,
- Choleretic decoctions, teas.
Infusions with a choleretic effect should be given to children with great caution - manifestations of allergies to herbs are possible. The most popular infusion for gall bladder problems is Mint.
Take celandine, mint leaves and cinquefoil. Everything should be in equal proportions. The total weight should be no more than 2 grams. Pour a glass of boiling water over the herbal mixture and let cool slightly. This infusion perfectly “disperses” bile and helps normalize liver function. Mint infusion is taken hot, like tea, twice a day. The general course of treatment is at least two weeks. This tea should not be given to children under 6 years of age.
The video below presents some effective recipes for choleretic decoctions and infusions. But before preparing the decoction, check whether a child at this age can drink such an infusion.
Mineral waters or Tyubazh
Rinsing the gallbladder is carried out strictly in the morning. A few days before it, you don’t need to eat salty or fatty foods.
You will need half a liter of still mineral water (Essentuki or Borjomi). The water must be heated to 40 degrees Celsius.
Add a tablespoon of Magnesia (powder) to a glass of hot liquid. Instead of magnesium sulfate, you can use your choice of “Sorbitol” or “Holosas”. The resulting solution must be taken orally. Lying on your right side, apply a warm heating pad to the hypochondrium area. This therapeutic “lying down” should last at least 2 hours. After this, it is advisable to empty your intestines. The most difficult thing here is to force the child to lie in one position for so long. But try to combine YouTube and watching cartoons. Tubage is carried out on the recommendation of a doctor and no more often than once every 6 months.
Choleretic oil
Flaxseed oil is considered a strong choleretic folk remedy. But the store-bought version of this product will not work. Make your own butter. 100 grams of flaxseeds should be ground in a coffee grinder or blender, placed in a liter jar, and topped with refined (odorless) sunflower or olive oil. Your flaxseed oil should be stored in the refrigerator for a week, and then you can give it a teaspoon to your child before meals.
Clinical guidelines
Since cholecystitis is a very common problem in children, the rules for diagnosing and treating a sick child are provided for at the legislative level .
This document contains all the recommendations regarding the rules of diagnosis (which can pose a serious problem in the absence of clinical manifestations) and treatment (therapy regimen and list of drugs recommended for use by young children).
Clinical protocol for the diagnosis and treatment of cholecystitis in children.
Prevention
In order to prevent the development of cholecystitis in a child, it is necessary:
- Protect the baby from contact with bacteria, identify and treat bacterial and helminthic diseases in a timely manner.
- Prevent the development of chronic foci of infection in the body.
- Monitor your baby's diet and lifestyle.
- Strengthen immunity.
Cholecystitis is a common but very insidious disease that cannot always be detected in the early stages of its development.
However, this is very important, because over time the disease becomes chronic, which makes treatment even more difficult.
A variety of causes and diseases can lead to the development of pathology, and, in turn, cholecystitis itself can serve as a prerequisite for the development of serious complications .
Dr. Komarovsky about problems with the gallbladder in children in this video:
We kindly ask you not to self-medicate. Make an appointment with a doctor!
What is suspension in the gallbladder?
In the modern world, one third of the population suffers from gallstone disease. Thanks to scientific advances, surgery and pharmacology, the percentage of life-threatening complications is steadily decreasing.
At the same time, the possibilities of non-invasive diagnostics are expanding. Timely examination of the organs of the biliary system allows you to avoid early operations.
The decisive diagnostic technique is ultrasound examination of the abdominal organs (ultrasound). The high resolution of this method makes it possible to detect deviations from the norm at the earliest stages. The first pathological signs that can be detected on ultrasound are suspensions in the gallbladder. Normally, there should be no suspensions.
Echogenic suspension in the gallbladder
In the first stages of stagnation in the biliary system, ultrasound scanning reveals an echogenic suspension in the gallbladder. Losing its natural homogeneity, it becomes “flaky”, heterogeneous, and as a result of this, its acoustic resistance changes and flakes appear in the gallbladder.
If normally homogeneous contents absorb the ultrasonic signal, then when “sediment” or “flakes” appear, the ultrasonic wave is reflected, or so-called “echogenicity” appears.
Hyperechoic suspension in the gallbladder
Subsequently, when the components of the sediment stick together in the gallbladder, biliary sludge clots appear. The contents become denser and less homogeneous, and on ultrasound it is visualized as a hyperechoic suspension in the gallbladder.
Biliary sludge in the gallbladder
In a healthy person, the organ is filled with viscous, concentrated bile, homogeneous in its physical properties. At the initial stages of gallstone disease, stagnation of bile occurs, resulting in the formation of a sediment or suspension consisting of bile components - crystals of bile pigments, cholesterol and calcium salts. This condition is called biliary sludge, from biliaris (Latin) - “gall bladder” and sludge (English) - “mud”, which, in fact, is the initial manifestation of gallstone disease.
The sediment in the gallbladder is called biliary sludge
Losing its homogeneous physical structure, pathologically altered bile acquires new properties. The denser its components become, the more intense the return signal from the ultrasound scanner will be. Based on the nature of changes in biliary sludge during ultrasound examination, three groups are distinguished.
Fine suspension
When the adhesion of particles of bile sediment (biliary sludge) becomes intense, a fine suspension in the gallbladder is formed in the lumen. What is this? This is a sediment that consists of microlites - small - up to 4-5 mm hyperechoic inclusions without an acoustic shadow, which can be clearly visualized when the patient’s body position changes during the study.
Sludge
During sludge, the contents of the organ that deposits bile can be densely filled with clots of putty-like, “silty” consistency, the so-called. sludged bile. Scanning of these changes also reveals a hyperechoic suspension, with a horizontal level without acoustic shadow, slowly changing in accordance with changes in the patient's body position.
Sludge bile
When the components of sludged bile crystallize, it is possible to observe a combination of fine suspension - microlites with thick sludged bile. Gallbladder sludge syndrome is the onset of gallstone disease.