Symptoms of the so-called “intestinal flu” - nausea, vomiting, stool upset, abdominal pain, fever, weakness - are observed more often in the spring and autumn, but their appearance is excluded in the summer. A person can get this infection at any age, but the majority of those affected are children, from the first days of life to adolescence. In fact, the viruses that cause this disease are not related to the influenza virus. The strange term “intestinal flu” appeared due to the fact that outbreaks of this infection often coincided with an increase in the number of acute respiratory viral infections (including influenza) in the cold season and a partial reminder of the manifestations of the disease with typical symptoms of a cold infection (weakness, fever, aches and pain in joints, etc.).
Causes of intestinal flu
Symptoms and causes of intestinal flu are often caused by an invading viral infection. Professors have described a large number of virus strains. The causative agents of intestinal flu are known, often the causes are:
- Rotaviruses.
- Astroviruses.
- Noroviruses.
- Caliciviruses.
- Adenoviruses.
Viral strains cause an acute inflammatory process in the digestive tract. There are clinical symptoms of intestinal infection, symptoms of acute respiratory infection, similar in symptoms to influenza.
Similar symptoms of E. coli in children.
Epidemiology
Most often, manifestations of rotavirus disease in a child can be detected in the autumn-winter period. Often large outbreaks of the disease occur during seasonal respiratory infections.
“Intestinal flu” received its unofficial name due to the highest prevalence of infection on the eve of influenza epidemics.
Due to its high contagiousness (infectiousness), the disease often occurs en masse, and group diseases are observed in children's institutions and hospitals. Predisposing factors for the development of the disease include the cold season, overcrowding in hospitals, and frequent contacts of children in groups.
Cases of rotavirus infection in children under 3 months are very rare. Infants have immunity acquired from their mother during pregnancy or breastfeeding.
Routes of infection
Infection occurs when the microorganism penetrates the epithelial cells of the mucous membrane of the gastrointestinal tract. The severity of clinical symptoms depends on the number of pathogens in the body and the state of the child’s immune system. Symptoms and treatment vary depending on the nature of the pathogen.
Routes of infection are determined based on the nature of the disease:
- Infection through nutritional routes. Pathogens enter the child's body with unwashed fruits and vegetables. You can become infected with low-quality, expired dairy and meat products.
- E. coli in a child can be transmitted through unwashed hands.
- Stomach flu in children can be transmitted through water contaminated with the corresponding strain of virus or bacteria.
- Viral stomach flu can be infected by airborne droplets. The pathogen is transmitted from a person by talking or sneezing.
- Signs of intestinal flu are observed through contact and household infection of a child. It is enough for a child to hold in his hands a toy that a sick child was playing with the day before, or to hold on to the door handle in a kindergarten or school.
Virus persistence in the environment
Rotavirus influenza is resistant and viable. This type of infectious pathogen can withstand heating up to 60 degrees and freezing.
Not all cleaning products kill the virus in the environment. Prevention of spread in the environment is carried out with high concentration chlorine-containing antiseptic solutions.
Folk remedies
In parallel with traditional treatment, traditional methods can be used to alleviate the condition of intestinal flu:
- Tea with mint. It has a pronounced antibacterial and anti-inflammatory effect. Helps stop the initial signs of the disease, destroying the causative agents of viral infection. To prepare the drink, add a little peppermint to boiling water and cook over low heat for 20 minutes. Afterwards, the tea is filtered and drunk up to 4 times a day between meals.
- Chia seeds. An effective remedy for restoring water-salt balance in case of stool disturbances and severe vomiting. The seeds have a hydrophilic property. Saturate the body with fiber, vitamins and essential nutrients. Used as a drink. Dissolve 1 tbsp in a glass of water. spoon of seeds, let it brew for 10 minutes and drink in one go. If necessary, you can add a little honey.
- Turmeric. Widely used to treat disorders associated with the gastrointestinal tract. Helps suppress infection, inflammation and bloating. Has antibacterial and antioxidant properties. Used in combination with milk, tea, soups and vegetable dishes.
The main advantage of traditional therapy is safety and simplicity. However, you should not abuse home methods; it is recommended to consult a doctor before use.
Clinical manifestations of the disease
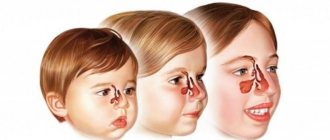
Parents should understand what the symptoms of intestinal flu mean in a child and how to treat intestinal flu. The first clinical manifestations of intestinal flu are signs similar to respiratory infections. The child has a sore throat and cough. There is mucous discharge from the nasal passages.
Clinical signs resolve on their own. Symptoms of intestinal distress appear. The sequence distinguishes intestinal flu from other infections that affect the child’s digestive tract. The latter begin with manifestations of dyspepsia.
Typical clinical symptoms
Rotavirus infection and stomach flu proceed according to a characteristic pattern:
- The appearance of pain, congestion in the throat and nose. When examined, the throat in young children may be hyperemic.
- Catarrhal symptoms of the upper respiratory tract - cough and runny nose, sneezing, hoarseness.
- Diarrhea develops on days 2-3. In mild stages of the disease, diarrhea occurs up to 10 times a day. The stool is grayish in color and has a pungent odor. In severe forms of the disease, the number of urges to defecate reaches 50 times a day.
- The child complains of pain in the abdomen. From time to time, the baby feels turbulence in the tummy and bloating. The child is in excruciating pain. He screams and knocks his legs.
- The temperature in newborns is subfebrile, reaching febrile levels.
- Nausea and vomiting, frequent diarrhea lead to the development of dehydration in the child.
- Signs of intoxication - the child is lethargic, sleeps poorly or is excessively sleepy. Skin color is pale. Facial features are pointed.
Clinical forms of intestinal influenza
To understand the intestinal flu symptoms, you need to know the different forms of severity of the disease.
Classification of the disease according to characteristics:
- According to the severity of the condition, the disease is mild, moderate, severe.
- Clinical manifestations are divided into typical and atypical forms of the disease. The first form proceeds according to the scheme described above. The second form may not have clinical symptoms and may be mild. The typical form also occurs in a month-old or one-year-old child. The atypical form is typical for adolescents. In adults, the disease may not have clinical symptoms.
Treatment of intestinal flu in children at home is allowed if the disease is mild. Other forms of the disease require hospital treatment.
Possible complications
Rotavirus is an infection that is rarely accompanied by serious complications. This happens if timely treatment is started.
Lack of adequate care for children under one year old leads to the development of unpleasant complications from intestinal flu. It happens if a child has a significant decrease in the body’s immune defense.
A complication is severe dehydration, which can lead to the development of hemodynamic disorders. Intoxication at a severe stage can lead to the development of acute renal failure.
A secondary bacterial infection may occur. These are Escherichia or other types of pathogenic rods. Antibiotics with a wide therapeutic spectrum are prescribed for the treatment of children.
With careful supervision of the child and adequate treatment, you will avoid the development of the listed conditions. The attending physician will examine the child and determine what to do and whether antibacterial drugs can be taken.
When should you call an ambulance immediately?
The biggest problem during illness is indigestion in children, nausea and vomiting. They can lead to dehydration (dehydration) of the child's body, which should be avoided at all costs.
Even if you think that this phenomenon is not considered serious, pay attention to the following signs, and then call a doctor immediately.
- If a child aged 0-12 months has intestinal symptoms that persist for more than 2 days.
- The baby is 2-3 years old and the symptoms do not go away within 3-4 days.
- The child has severe nausea and vomiting. Sometimes this condition requires hospitalization.
- The baby does not drink water and does not urinate during the day.
- After defecation and in the vomit there are blood impurities.
- High fever does not go away after 2 days.
- Dry and cracked lips appeared.
- Excessive sleepiness.
- Moodiness.
- Sunken eyes.
- Colic.
- Dizziness.
- Pale and cold extremities.
Diagnosis of intestinal flu
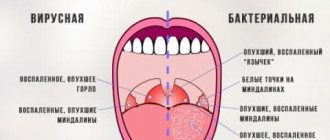
An experienced pediatrician or infectious disease specialist can determine the diagnosis based on the first clinical manifestations. Often, viral and bacterial infections exhibit significant external similarities. Salmonellosis and dysentery can be hidden under the guise of the flu. Possible development of food poisoning. To differentiate between intestinal infections, bacteriological studies are prescribed.
Viral particles are too small to be visible under a microscope. Bacterial infections are detected. The pathogen is distinguished by the characteristic color of the cell nucleus.
Useful and reliable diagnostic information is obtained from studies:
- Polymerase chain reactions.
- Methods of immunofluorescence analysis.
- Enzyme immunosorbent studies.
These tests will detect rotavirus. Research is expensive and rarely used.
For intestinal flu, a standard list of diagnostic procedures is prescribed:
- General blood analysis.
- General urine analysis.
- Stool analysis for coprogram, bacteriological culture.
Tests identify signs of inflammation in the body and check for possible bacterial infection.
What can and cannot be given to a child with intestinal flu?
While the child is experiencing discomfort, pain, fever and other symptoms of illness, several techniques can be used.
They will help alleviate the baby’s condition with intestinal flu.
- Try giving your child water in small portions at regular intervals.
- Do not give milk or dairy products to a sick child.
- Don't give him drinks that are high in acid.
- You should not give your child foods that are heavy on the stomach. Light vegetable soups and soft porridges (not made with milk) are recommended.
- It is not recommended to give your child medications without the approval of the pediatrician. Sometimes the disease goes away on its own.
- Some liquids, such as soft drinks, sports drinks, apple juice, tea or chicken broth, contain the wrong amount of salt, sugar and water, which can make the condition worse.
- You should avoid feeding your child any fruit juices or foods high in sugar as they tend to make the flu worse.
- The child should remain in bed for twenty-four hours until the diarrhea and vomiting stop. If a child has a fever, the temperature should be checked and noted in a log every four hours.
If symptoms persist after therapy, call your doctor again. After 1-2 days, the first results of therapeutic recovery will be noticeable. If one of the signs of the disease does not go away, you may need to be hospitalized with medication.
Principles of treatment
No specific medicine has been developed to treat the cause of the disease. Therapeutic measures differ in the following areas:
- Detoxification therapy.
- Measures to eliminate signs of dehydration.
- Restoring the functions of the urinary system.
- Restoration of the cardiovascular system.
- Symptomatic therapy.
- Preventive measures aimed at preventing secondary bacterial infection.
You can take medications with the permission of your doctor. You should not put your baby’s life and health in danger by engaging in self-medication. If you find signs of an intestinal disease in a child under one year old, call a pediatrician at home. The doctor will give a referral to the hospital if necessary. In case of a mild form of the disease, children are kept on sick leave on an outpatient basis. The moderate or severe form requires treating patients with intestinal pathology in an infectious diseases hospital.
Before the doctor arrives, give the child first aid.
First aid at home
If you find signs of a respiratory infection in your child combined with symptoms of an intestinal disorder, let’s drink more.
If vomiting does not stop, drinks are given one teaspoon at regular intervals. A large amount of water is not retained in the baby’s stomach and provokes a new attack of vomiting. Pour boiled water and tea. Saline solutions such as Regidron have an effect. Brew medicinal herbs from folk recipes. You should drink a lot, but in small doses.
Monitor your child's position in bed so that he does not choke on vomit. Turn the baby's head to the side and do not leave it unattended. Choose the right pose! Lying on your back is harmful for infants.
Check your child's body temperature. If it rises from 38 degrees, do not tolerate it, take antipyretic drugs based on Paracetamol. Such medications are given to a child who is one month old.
A healing condition is a gentle lactose-free diet. Do not force your child to eat if he has no appetite. Offer to drink regularly. Dishes should be prepared steamed or boiled. Nutrition for patients with intestinal infection is gentle and fractional.
Drug treatment
The full course of drug therapy is carried out over 10 days. Anti-epidemiological drugs help raise the body's immune defense and prevent the spread of the disease. Pathogenetic treatment is selected individually for the child based on his condition.
To eliminate signs of dehydration, saline solutions are used orally, parenterally. If, after treatment with drinking solutions, vomiting does not stop and dehydration increases, switch to intravenous infusions. They are carried out in the infectious diseases department of a hospital for acute life-threatening conditions. Use Enterodes, Regidron internally. You can make your own drinking mixture at home.
To remove pathogenic particles from the body, drugs from the group of sorbents are used. Medicines - Polyphepan, Laktofiltrum or Enterosgel. The purpose helps to quickly cleanse the body of viral particles and bacterial toxins.
To speed up the restoration of non-pathogenic intestinal flora, give your child probiotics. They will help to quickly restore epithelial cells affected by intestinal infection and normalize intestinal activity. Acipol and Linex are effective. The preparations contain lyophilized live cultures of beneficial intestinal bacteria and quickly restore normal microflora in the intestines.
If the child has a fever, fever, or chills, give medications with an antipyretic effect. Paracetamol, Efferalgan, Nurofen - medications for children are available in the form of rectal suppositories, mixtures, and syrups for oral administration.
Enzymes are prescribed to the child to normalize digestive processes. With rotavirus infection, the normal enzymatic function of the intestine decreases - it must be maintained so that the child’s body can sufficiently absorb incoming nutrients. Enzymatic preparations Creon, Mezim, Pancreatin have proven their effectiveness.
Pathogenesis
The pathogen enters the baby’s body and reaches the small intestine. Invading the cells of the surface layer of the intestinal wall, the infectious agent begins to actively multiply. The process of breakdown and absorption of nutrients is disrupted, and diarrhea occurs.
A distinctive feature of rotavirus is the ability of the pathogen to cause lactase deficiency. Normally, the enzyme is synthesized by intestinal cells and is necessary for the absorption of lactose. If there is a deficiency of the substance, dairy intolerance occurs, which lasts for several weeks.
Diet food
The diet for stomach flu is considered gentle. The child is fed slimy, boiled soups, semi-liquid porridges with water. Serve meat dishes pureed, boiled, and steamed.
Strong meat broths are strictly contraindicated in the acute period of the disease. Cook the soup in vegetable broth. It is recommended to give your child boiled fish and fish dishes. Prepare fish soufflé and steamed cutlets from low-fat fish.
It is better to give yesterday's bread, slightly stale. Cookies or crackers are low-fat and not rich. Give your baby biscuits for tea or compote. During the illness, it is strictly forbidden to give the child whole fresh milk and dairy products. Fresh vegetables, fruits, pickles, and marinades are excluded from the diet. Smoked and fatty foods are prohibited. Serve vegetables and fruits baked or boiled. Prepare the puree with a pinch of salt and sugar.
You need to return to your usual diet gradually. The whole process takes a month.
About the reasons
The source of rotavirus infection is always a sick person. Moreover, you can become infected not only from a sick person with obvious clinical manifestations, but also from an asymptomatic carrier of the infection.
The greatest danger is posed by a patient in the acute period of the disease, the average duration of which is 5 days. But virus shedding can persist for up to 20 days from the onset of the disease. Sometimes, with reduced immunity, the patient remains infectious for up to a month or develops virus carriage.
Viruses enter the environment through feces and saliva, and infection occurs mainly when the pathogen is swallowed by a child.
Just 1 gram of feces of a sick person can contain more than 10 trillion viral particles, and 100 units are enough to infect a child. Therefore, the risk of contracting intestinal flu if basic hygiene rules are not followed is enormous.
Most often, the virus enters the baby’s body through infected things - toys, underwear, household items. But it is possible that an infectious agent can penetrate through the consumption of unboiled water or contaminated food.
The virus can also spread through airborne droplets, sneezing, coughing, or kissing. But such cases of infection are less common.
Disease prevention
Intestinal flu caused by rotavirus infection is characterized by specific prevention through vaccination. No specific prophylaxis has been identified for other viruses. It remains to follow the general rules to prevent infectious diseases of the digestive tract.
To avoid contracting intestinal flu, follow general hygiene rules:
- Avoid contact with people with intestinal infections. During the epidemiological peak, it is better to limit contacts. You can get infected both from a sick child and from a healthy carrier.
- If there is a patient with an intestinal infection in the house, he uses separate dishes and household items. The premises and household utensils are disinfected.
- Wash your hands when coming from the street or from public places, as well as after contact with a sick person or carrier of viral intestinal flu. In addition, carry out this procedure after visiting the toilet and before eating.
It is not recommended to drink raw water from untested sources or eat unwashed vegetables and fruits. Meat and fish undergo heat treatment, milk is boiled before consumption.
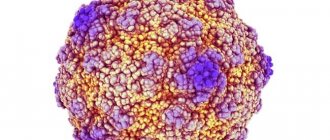
What is rotavirus infection
Intestinal flu is an infectious disease that develops due to rotavirus entering the body. Humanity learned about this pathogen not too long ago. Rotavirus was first discovered in 1974. It is very resistant to adverse environmental influences. Intestinal flu occurs in all children who have not previously encountered this disease.
Rotavirus infection in children is classified as a “disease of dirty hands.” Most often, the disease is diagnosed at the age of 6 months to 2 years, when the child is just beginning to get acquainted with the world or attends nurseries, kindergartens and does not properly observe the rules of personal hygiene. Intestinal flu can also be detected in older children. By the age of 5, almost all children suffer from this disease.
Compliance with hygiene rules, boiling water, and careful processing of food before cooking cannot protect children from infection with rotavirus infection 100%, since intestinal flu is very resistant to various influences and can enter the body in different ways. For example, the enteral route of infection (through the mouth) is not the only one. Pathogens can be transmitted by airborne droplets from a sick person or a carrier of infection.
Rotavirus infection very easily penetrates the child’s intestines. The protein shell of microorganisms is not destroyed by gastric juice, bile and other enzymes. The following processes occur in a child’s body after infection with intestinal flu:
- Rotaviruses penetrate the cells of the tissue lining the intestines.
- Microorganisms multiply.
- The inflammatory process begins in the intestines.
- There is a disruption in the processes of digestion and absorption of nutrients into the blood.
The causative agents of intestinal flu in a child are excreted from the body in feces. 1 g of feces contains a huge amount of them, about 10 trillion. To infect a healthy child with rotavirus, 10–100 microorganisms are sufficient.
The acute period of the disease can last from 3 to 7 days. In severe cases, the symptoms of rotavirus in a child may be observed for a longer period. After this, a recovery period will begin (4–5 days).