Tracheitis in children is an inflammatory disease concentrated in the trachea. It may be limited or affect the larynx and bronchi. Tracheitis is not life-threatening for the child, but requires a mandatory examination by a doctor for accurate diagnosis and effective treatment.
In young children, the disease is quite unpleasant, with bouts of severe coughing. But with adequate, timely treatment, tracheitis goes away without leaving a trace, without leading to complications.
Professional consultation is important to identify the cause and type of tracheal damage, which is divided into:
- acute or chronic;
- catarrhal;
- hyperplastic;
- atrophic.
Each type of disease has special symptoms and specific treatment. To understand how to cure tracheitis, it is necessary to have a general understanding of the structure of the respiratory system.
The trachea is a tubular organ that conducts air into the lungs and connects the larynx with the bronchi. Inside, the trachea is covered with epithelium, the sensitive endings of which react to external stimuli. When infections, chemicals or allergic substances enter the trachea, inflammation occurs. In this case, irritation of nerve receptors causes coughing attacks.
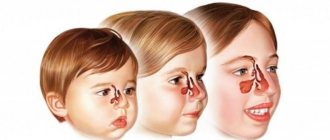
As a rule, tracheitis occurs in school-age children as a complication of viral infections. Before 6-7 years of age, isolated tracheitis is observed infrequently, since the inflammatory process covers the entire respiratory tract of the child.
Causes of childhood tracheitis
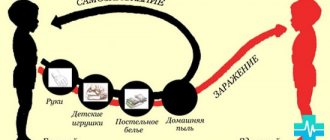
In the vast majority of cases, the disease is caused by a variety of infections: viruses, bacteria, and their associations. During the cold season, the likelihood of developing tracheitis increases. The reason for this is infection with respiratory viruses. It is important to remember that respiratory tract diseases, in the absence of proper treatment, develop according to the following scheme: laryngitis - tracheitis - bronchitis.
Subsequently, a bacterial component (streptococcus, staphylococcus, etc.) may be added to the viral component. The causative agents of childhood diseases, in particular measles, whooping cough, can also cause an inflammatory process.
The best prevention of tracheitis at this time is to follow infection safety measures: avoid close contact with sick people, ventilate rooms, wear a mask in crowded places, in particular during visits to a children's clinic.
Non-infectious causes
Other factors for tracheitis in children cannot be ruled out. These include:
- low or high temperature exposure (breathing icy or hot air with dust particles);
- inhalation of toxic fumes (household chemicals, paints, tobacco smoke, etc.);
- allergic nature.
Pediatricians include hypothermia, weakened immunity, difficulty in nasal breathing caused by enlarged adenoids, and chronic sinusitis as provoking factors. These unfavorable moments do not directly lead to inflammation, but damage the protective barrier that prevents the proliferation of bacteria.
Description of the disease
The trachea is a tubular organ that connects the larynx and bronchi and serves to conduct air into the lungs.
When allergens or infectious agents come into contact with the tracheal mucosa, a diffuse inflammatory process develops that covers the entire organ. Due to irritation of the nerve endings, a protective reflex is formed - cough. With tracheitis, it is dry and unproductive. Tracheitis can be infectious (caused by fungi, bacteria, viruses, protozoa) and non-infectious (allergic). Depending on the course, there is an acute form (severe symptoms for a short time) and a chronic form (long-term moderate or mild symptoms). As a rule, chronic occurs against the background of serious systemic diseases or with inadequate acute therapy.
In pediatric otolaryngology and pediatrics, inflammation of the respiratory tube rarely develops in isolation. More often this occurs against the background of ARVI, when not only the trachea is affected, but also other organs of the respiratory system. In young patients, tracheobronchitis and laryngotracheitis are more often diagnosed.
Long-term inflammation of the tracheal mucosa leads to its morphological changes. Chronic tracheitis occurs with hypertrophic processes (thickening of the mucosa) or atrophic (thinning of the membranes).
Symptoms of tracheitis in children
The presence of inflammation of the trachea may be indicated by:
- Paroxysmal cough.
- Pain behind the sternum when inhaling.
- Hoarse breathing.
- Sore throat.
- Fatigue, poor sleep, lack of appetite.
In some cases, an increase in temperature is observed. It is not a mandatory sign, but rather is associated with a primary infection.
Prevention
It is important to spend time on preventive measures. Unfortunately, many parents do not attach much importance to this, or do not want to waste their time. However, they must understand that the child’s health is the most valuable, and it must be taken care of from childhood, and every disease causes serious stress to the body.
- Teach your child to wash his hands, wash his face, and brush his teeth. Following these fairly simple rules will help to significantly reduce the risk of developing viral and bacterial pathologies.
- Avoid inhaling contaminated air or other irritants. Make sure that there are no smokers in your child’s company; passive smoking causes great harm to health.
- Always monitor the optimal level of humidity and temperature in the room. To do this, you will need to ventilate the room when there is no child in it and, at least every other day, wash the floors. And if necessary, purchase a special air humidifier.
- A balanced diet and good sleep significantly increase the body's support functions.
- Pay great attention to hardening procedures and daily physical exercise, take care of vitamin therapy. All this will help strengthen the child’s immunity.
Now you know what the treatment of tracheitis in children is, what are the main signs and causes of this disease. My advice to you is that at the first sign of deterioration in your baby’s health, do not hesitate, consult a doctor. Diagnosing and starting treatment for a disease at an early stage is much easier than later dealing with a protracted process or one that has become chronic, not to mention what the child has to go through at this moment. Remember about prevention methods and practice them constantly. Don’t forget, a healthy child is a happy one!
Features of cough
Cough is accompanied by many childhood diseases, in particular, laryngitis, bronchitis, and pneumonia, so pediatricians pay close attention to this symptom. With tracheitis, the cough worsens in the morning, immediately after waking up. This is caused by swelling and phlegm accumulation during sleep.
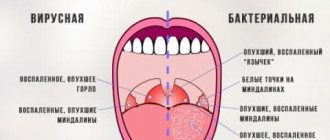
The nature of the cough with inflammation of the trachea is violent, with sharp sound tones. It may be dry or moist with the discharge of viscous sputum. Bacterial tracheitis is characterized by greenish sputum, while viral tracheitis is characterized by sparse, white or gray sputum.
Causes
There are preconditions of infectious and non-infectious nature.
Infectious diseases include the penetration of various pathogens into the body:
- measles;
- influenza sticks;
- pneumococcus;
- enterovirus;
- hemophilus influenzae;
- mycoplasma;
- chlamydia;
- coronaviruses;
- PC virus;
- flu;
- adenovirus;
- whooping cough
Non-infectious causes include:
- influence of allergens;
- inhalation of too cold or hot air;
- penetration into the body of chemical particles and cigarette smoke from passive smoking;
- a solid object entering the trachea.
In addition to the above reasons, it is worth mentioning factors that increase the risk of developing tracheitis in a child:
- hereditary predisposition;
- chronic pathologies of the respiratory system.
How to treat tracheitis in children
Reputable pediatricians warn that if tracheitis is suspected in a child, parents should urgently seek medical help, and if there is a fever, call a doctor at home.
If it is impossible to obtain a consultation with a specialist on the same day, measures must be taken to relieve the cough and the general well-being of the sick person. It must be remembered that medications for adults should not be given to children: this is fraught with severe side effects and negative consequences.
Acute tracheitis can be quickly cured by complex therapy aimed at both eliminating inflammation and relieving a debilitating cough. A competent combination of medications, physiotherapy and folk remedies will help to resolve the disease quickly.
For mild forms of tracheitis in children, antibiotic treatment is not indicated. But if the microbial nature of the inflammation is confirmed, for example, green sputum is present, then antibiotic therapy is recommended without fail. The type and dosage of the antimicrobial drug is selected only by the pediatrician after examination.
Treatment of tracheitis
Doctors approach the treatment of tracheitis in a comprehensive manner.
Specialists carefully study the features of the clinical case and draw up a personalized therapeutic program. It is aimed at eliminating the cause of the disease, reducing the severity of symptoms, speedy recovery of the body and prevention of relapses. With this approach, you can count on quick relief and complete recovery. Treatment of tracheitis involves etiotropic therapy. Antiviral, antibacterial, antiprotozoal or antifungal drugs are prescribed (depending on the pathogen). For allergic forms, antihistamines are selected. Boring cough in the acute phase is treated with antitussives. As sputum forms, expectorants and mucolytic drugs are prescribed. During the recovery period, vitamins and immunomodulators are indicated.
With chronic tracheitis, it is extremely difficult to achieve recovery. Measures to prevent colds and viral infections are advisable. It is important to promote the child’s health in a comprehensive manner: ensure a rational regimen, nutritious nutrition, and sufficient intake of vitamins and minerals.
In the acute period of tracheitis, inhalation with a nebulizer has a good effect. After the inflammatory process subsides, physiotherapy (massage, electrophoresis, UHF) is prescribed. They improve microcirculation in the organs of the respiratory system, have a stimulating effect on local immunity and promote tissue restoration.
For a complete recovery, it is important to ensure optimal conditions at home: maintain air humidity, ventilate the room, carry out wet cleaning, eliminate odorous substances, sources of dust, and prevent inhalation of tobacco smoke. It is advisable to avoid temperature changes for a while.
Treating cough
If you have a dry cough, the main measures are aimed at turning it into a wet one. Then the pain and frequency of attacks will decrease. To solve this problem, the doctor can prescribe syrups or drops to thin the sputum: Lazolvan, Ambrobene, etc. After a wet cough appears, the doctor can adjust the treatment regimen, replacing mucolytics with stimulation of airway clearance.
For children in their first year of life, doctors usually recommend herbal syrups that do not contain alcohol, such as Gedelix. After a year, you can give Linkas, Doctor Theis, Tussamag, Travisil syrups. From the age of 3, tracheitis can be treated with almost all herbal cough syrups based on licorice, ivy, plantain, thyme and other medicinal plants.
Diagnostics
- Initially, the child is examined by a pediatrician, listens to the chest, and looks at the condition of the throat mucosa. Next, a list of complaints about well-being is collected, and a preliminary conclusion is made.
- General analysis of urine and blood.
- Biochemical blood test.
- Bacterial culture from the nose and throat.
- Laryngotracheoscopy.
- Endoscopic examination.
- X-ray.
It is not necessary that your baby will need to undergo all of the above examinations. In most cases, basic methods are sufficient, and only if something more serious is suspected, additional studies may be prescribed.
In addition, you need to know that there are a number of diseases whose primary symptoms are similar to tracheitis. These include:
- laryngitis;
- whooping cough;
- bronchitis;
- pharyngitis;
- pneumonia;
- tuberculosis;
- the presence of a foreign body in the child’s throat.
Therefore, it is so important to come to an appointment with a doctor who can carry out differential diagnostics when examining the baby, or prescribe additional examinations to establish a diagnosis.
Nebulizer or grandma's potatoes?
At home, inhalations using a special device - a nebulizer - help well. The advantage of a compressor inhaler is that it sprays any liquid substance into fine dust, be it a regular saline solution, mineral water or a pharmaceutical inhalation product. In this case, the steam temperature does not exceed room temperature.
For tracheitis, inhalation treatment using a nebulizer has an undoubted advantage. The sprayed fine vapor penetrates directly into the affected area, its deposition in other areas is minimal. In this case, such a high absorption of the drug is achieved that the effect occurs after 2-3 procedures.
The old-fashioned way of breathing over potatoes or boiling water is unsafe for small children. Firstly, hot steam can cause burns to the skin and inflamed mucous membranes. Secondly, always restless children can simply spill the hot contents of the inhaler on themselves.
The latest generation of children's nebulizers resembles more a toy than a medical device and is equipped with a special nozzle for a small child. The cost of the inhaler is justified by the fact that they can be used to effectively treat many respiratory and allergic manifestations in both children and adult family members. By purchasing this useful device, you can relieve your cough at home in a few days.
Possible complications
If the disease is not diagnosed in time, serious consequences can begin to develop. The same applies to attempts to independently treat a child, resorting to traditional methods and without consulting a doctor.
Parents should understand that the development of consequences can also be a consequence of weakened immunity or the presence of chronic pathologies in the baby’s body.
So against the background of tracheitis the following can develop:
- bronchitis;
- pneumonia;
- bronchopneumonia;
- bronchial asthma;
- tracheobronchitis;
- attack of suffocation.
In extremely rare cases, the formation of neoplasms, both benign and malignant, is possible.
Also, if left untreated, the acute form of the disease can become chronic.
Folk remedies
Traditional medicine offers many effective methods for treating tracheitis in children, but it would be more correct to combine such methods with traditional therapy. In this case, recovery will go much faster.
Such events include:
- gargling with herbal tinctures;
- warming compresses;
- rubbing with goose fat, herbal balms;
- dry heat (mustard).
Special mention should be made about the use of mustard in the treatment of children. A small child has delicate skin, so mustard plasters need to be placed through gauze or thin cloth and held for no more than 10-15 minutes. Mustard irritates nerve receptors, providing a distracting and analgesic effect.
For children over 5 years old, it is good to steam their feet at home with hot water and mustard, especially if tracheitis is accompanied by a runny nose. You can sprinkle dry mustard powder into your socks at night, putting another warm pair on top.
Healing drink
Warm milk with honey will help alleviate the condition of laryngitis and tracheitis. Boil 200 ml of milk, after it has cooled to 40 ° C, add a tablespoon of cow butter and honey, as well as a pinch of soda. The product has a diaphoretic and relaxing effect, so it should be given once a day, just before bedtime.
Treatment
The treatment process is simple, but can be complicated by relapses - exacerbation of the disease upon contact with an allergen.
It is recommended that the child undergo a course of treatment exclusively under the supervision of a doctor, and always taking into account the results of an examination by an allergist and an ENT specialist. We can talk about a positive outcome of therapy only after the allergenic factor is detected and excluded.
Medication
Antihistamines (antiallergic) drugs are used, such as Suprastin, Loratadine and others . If bacterial flora is detected, antibiotics are prescribed. To remove sputum, expectorants are used - ACC, Fluimucil, Ascoril and others. If tracheitis of viral origin, such as influenza A and B, is diagnosed, Rematadine is prescribed.
Attention! All medications are prescribed individually by the attending physician! The article provides only examples!
Folk remedies
It is impossible to cure a child using traditional medicine methods, but it is quite possible to improve his condition a little, soften the cough and stimulate the immune system to work.
To reduce hyperemia, various mouthwashes are used: beetroot decoction, tincture of blackberry leaves and fruits. To soften the cough - warm drinks - these can be citrus juices (contraindicated if you are allergic to these fruits), rosehip or hawthorn decoctions, berry fruit drinks, with priority being lingonberries and cranberries. Drinking is taken in small sips.
Effective remedies include mustard plasters - interscapular and chest plasters, oil wraps, hot baths, honey compresses. Potato compresses have proven their effectiveness. Here are two examples:
First:
- Boil 2 medium-sized potatoes in their skins;
- While they are still hot, grind them to a puree and pour in a tablespoon of vegetable oil;
- Wrap the resulting pulp in gauze or a clean rag and place it on your chest;
- Keep until completely cool.
Second:
- Boil 500 ml of milk, remove from heat;
- Add pine buds;
- Leave the decoction for an hour;
- Drink in parts in one day (the same amount of milk 3–6 times a day). Repeat the procedure if necessary.
The use of steam inhalations is also recommended - the old grandmother’s method of “breathing over hot potatoes”. Inhalation will stimulate the body to remove mucus.
Tracheitis during pregnancy
In pregnant women, tracheitis is recorded quite often, mainly of a viral nature. It happens when a woman has an acute respiratory viral infection, when the tonsils become inflamed or there is inflammation in the throat. Tracheitis is dangerous for pregnant women, including for an unborn baby, because the pathogen can penetrate the fetus through the placenta.
If the disease is bacterial in nature, then treatment can be dangerous for the pregnant woman. It is widely known that antibiotics are prescribed to pregnant women only in extreme cases. A pregnant woman with tracheitis is likely to have complications, mainly bronchitis, in severe cases there may be bronchopneumonia. They affect the development of the unborn child.
Therefore, during pregnancy, prevention of tracheitis is important. A woman needs to avoid crowds of people, especially during the cold season and during epidemics of any diseases. Contact with patients should also be limited in clinics where pregnant women are registered.
Tracheitis - etiology
Infectious tracheitis is caused by the same pathogens that lead to the development of pharyngitis, laryngitis and rhinitis: streptococci, staphylococci. If these diseases are not treated (or treated incorrectly), the inflammatory process can spread to the trachea. Tracheitis can be acute or chronic.
There is also a non-infectious form of tracheitis, which develops as a result of hypothermia of the upper respiratory tract or the harmful effects of chemical suspensions, dust, and steam.
The development of tracheitis may be influenced by the following factors:
- inflammatory processes in the nasal passages and nasopharynx;
- smoking tobacco;
- regular inhalation of toxic substances;
- frequent hypothermia;
- chronic respiratory diseases;
- Constantly breathing in air that is too hot or too cold.