Purulent sinusitis in children most often occurs at the age of 6–7 years. The causes of the development of the disease are related to the anatomy of the maxillary sinuses in children. Sinusitis can be cured at home, without surgery. To treat sinusitis in a child, antibacterial therapy, various drops, warming up the sinuses, and inhalations are used. Additionally, they are treated using traditional medicine methods. If treatment does not help, a “cuckoo” is prescribed, and in extreme cases, a puncture of the maxillary sinus.
Causes and risk factors
The maxillary sinuses communicate with the nasal cavity through small openings. If for any reason (usually due to inflammatory swelling of the nasal mucosa) these openings close, then the sinuses stop being cleaned and ventilated. This creates in them a favorable environment for the activity of pathogenic microflora, which causes the development of an inflammatory process in the mucous membrane of the sinuses.
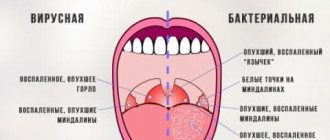
The causative agents of sinusitis in children are most often viruses. Less commonly (5–10% of cases), the disease is caused by pathogenic and opportunistic bacterial agents (Haemophilus influenzae, staphylococci, streptococci, moraxella), and even more rarely by a fungal infection.
Most often, children are diagnosed with sinusitis after 12 years of age.
Risk factors for the development of sinusitis in children are diseases that contribute to the penetration of infection into the maxillary sinus or disrupt its normal ventilation:
- chronic rhinitis of various etiologies;
- acute respiratory viral infection;
- chronic pharyngitis;
- chronic tonsillitis;
- adenoid vegetations;
- congenital anomaly of the structure of the nasal passages;
- diseases of the teeth of the upper jaw;
- dental interventions on the teeth of the upper jaw;
- deviated nasal septum.
Nature of the disease
The maxillary sinuses are cavities that are located on the sides of the nose, in the recess of the facial bone that passes into the upper jaw.
This is a space that is normally free of any fluids and is connected to the nasal passages by several narrow passages. When infectious agents enter the cavity, inflammation of the sinus mucous membranes occurs, and in response, purulent exudate begins to be produced. If the nose is functioning well and the ducts between the nostrils and the maxillary sinus remain open, the infection goes unnoticed: the immune system copes with the infection, the fluid from the cavity is gradually eliminated through the nose, and recovery occurs. In such cases, an episode of infection most often goes unnoticed, which is typical for a healthy body.
But in the presence of certain factors complicating the outflow of secretions, natural sanitation of the space does not occur, the fluid stagnates in the cavity and is a prerequisite for the development of the disease.
Important! Until the age of three, the development of sinusitis is unlikely - at this time the sinuses are just beginning to form and do not participate in air exchange. And imperfection of the cavity between the ages of 3 and 6 years can serve as a provoking factor for the disease.
Forms of the disease
Sinusitis in children can be catarrhal or purulent. In case of purulent inflammation, the discharge from the maxillary sinus is purulent or purulent-mucous, in case of the catarrhal form of the disease it is serous. Catarrhal inflammation can turn into a purulent form.
Depending on the route of infection into the maxillary sinus, the following types of sinusitis in children are distinguished:
- rhinogenic – microbes penetrate from the nasal cavity; this is the most common way;
- hematogenous - an infection through the bloodstream enters the sinus from another source of infection in the body;
- odontogenic – the source of infection is the carious teeth of the upper jaw;
- traumatic.
Inflammation of the maxillary sinus can be unilateral or bilateral.
With purulent sinusitis, pus accumulates in the maxillary sinus
The nature of the inflammatory process is acute and chronic.
Swimming in public pools with chlorinated water is contraindicated for children suffering from chronic sinusitis.
Depending on the morphological changes, chronic sinusitis in children is:
- exudative (catarrhal or purulent) – the predominant process is the formation of exudate (serous or purulent);
- productive (parietal-hyperplastic, atrophic, necrotic, polypous, purulent-polypous). With this form of the disease, pronounced changes in the structure of the mucous membrane of the maxillary sinus occur (hyperplasia, atrophy, polyps).
In clinical practice, polypous-purulent and polypous forms of chronic sinusitis are most often encountered.
Symptoms of sinusitis in children
Acute sinusitis begins with a sudden increase in body temperature to 38-39 °C, accompanied by chills. In rare cases, body temperature remains within normal limits. Children are bothered by pain localized in the area of the root of the nose, forehead, and zygomatic bone on the affected side. The pain can radiate to the temple and intensifies with palpation. Often the pain takes on a diffuse character, that is, it is perceived as a headache without a clear localization.
On the affected side, nasal breathing is impaired; with a bilateral process, children are forced to breathe through the mouth.
Nasal discharge at the onset of the disease is liquid and serous in nature. Subsequently, they become green, cloudy and viscous, dry out quickly and form rough crusts in the nasal cavity.
Sinusitis in children is accompanied by headaches, runny nose, and impaired nasal breathing.
Swelling of the nasal mucosa often leads to compression of the lacrimal canal. As a result, tear fluid cannot flow into the nasal cavity and lacrimation occurs.
Signs of sinusitis in children are often regarded by parents as manifestations of ARVI. However, the approach to the treatment of these diseases is different, so it is important that the sick child is examined by a pediatrician, and, if necessary, by an otolaryngologist.
The outcome of acute sinusitis in children can be recovery or the disease becoming chronic.
In the remission stage of chronic sinusitis in children, there are no signs of the disease. The children feel healthy and do not have any complaints. When the inflammatory process worsens, symptoms of intoxication occur (muscle pain, weakness, headache, loss of appetite) and body temperature rises to subfebrile levels (up to 38 ° C). The amount of nasal discharge increases.
Children under the age of 3-4 years do not have sinusitis, this is due to age-related anatomical features: by the time the child is born, the maxillary sinuses are in their infancy, their development begins after 5-6 years and continues until 10-12 years.
If, during an exacerbation of chronic sinusitis, the outflow from the maxillary sinus is disrupted, a headache occurs. It has a bursting or pressing character and is localized “behind the eyes.” Increased pain is caused by pressure on the eyes and cheekbones, and by looking up. In the lying position, the outflow from the maxillary sinus improves, and therefore the intensity of the headache weakens.
Another symptom of chronic sinusitis in children is a cough that occurs at night and does not respond to traditional therapy. The appearance of a cough is due to the fact that when lying down, pus from the affected maxillary sinus flows down the back wall of the pharynx and irritates it, i.e. the cough is reflexive in nature.
With chronic sinusitis in children, damage is often detected in the vestibule of the nasal cavity (weeping, maceration, swelling, cracks).
Local medical procedures
Rinsing the nasal cavity is one of the most effective procedures for sinusitis in a child. It is not always possible for a baby to blow his nose on his own to remove secretions from the nasal passages. The correct rinsing process guarantees improvement and restoration of the mucous membrane.
To make the procedure more effective, before rinsing, each nasal passage is irrigated with an isotonic solution. This allows you to remove mucus and dried crusts. The next step will be the instillation of vasoconstrictor drops, which will relieve swelling and open the anastomosis through which the nasal cavity and the maxillary sinuses communicate. Thanks to this, the contents of the maxillary sinus will easily come out.
After preparation, a washing procedure is carried out. The child's head should be turned to the side. The solution should be poured into one nostril and poured out of the other. The process is not pleasant for the child, but very effective. It is good to use chamomile decoction, furatsilin solution, and saline solution as washing solutions.
Diagnostics
Diagnosis of sinusitis in children is carried out on the basis of the characteristic clinical picture of the disease, complaints of the patient (or his parents), the results of a medical examination and laboratory and instrumental studies.
When performing rhinoscopy, inflammation of the mucous membrane of the nasal cavity, its swelling, and the release of inflammatory exudate from the sinus are detected.
X-rays are performed to confirm the diagnosis. With sinusitis, the x-ray shows a noticeable darkening of the maxillary sinus on the side of the lesion, but it should be borne in mind that an x-ray of an acute inflammatory process, especially at the onset of the disease, may be uninformative.
To diagnose sinusitis in children, rhinoscopy and radiography are performed.
If necessary, a bacteriological examination of nasal discharge is carried out to determine the pathogen and its sensitivity to antibacterial agents.
The causative agents of sinusitis in children are most often viruses. Less commonly (5–10% of cases), the disease is caused by pathogenic and opportunistic bacterial agents, and even more rarely by a fungal infection.
Treatment of sinusitis in children
For uncomplicated acute sinusitis in children, treatment is usually conservative and carried out on an outpatient basis. The treatment regimen includes:
- antibacterial drugs (eliminate the pathogen);
- non-steroidal anti-inflammatory drugs (have antipyretic, analgesic and anti-inflammatory effects);
- vasoconstrictor drops in the nose (improves outflow from the affected sinus).
If there is no effect from the conservative treatment of sinusitis, children are hospitalized in a specialized department for punctures or probing of the maxillary sinuses.
When treating sinusitis, children are prescribed antibiotic tablets.
In case of exacerbation of chronic sinusitis in children, treatment should be comprehensive, combining methods of local and general therapy.
To suppress microbial flora, antibiotics are prescribed, selected taking into account the sensitivity of the pathogen. If the causative agent of the disease is staphylococcus, then staphylococcal γ-globulin and antistaphylococcal plasma are used. Treatment of sinusitis in children of fungal etiology is carried out with antifungal drugs.
If necessary, drain the affected sinus. Subsequently, through the drainage tube, the sinuses are washed with antiseptic solutions, antibiotics are administered, taking into account the sensitivity of the microflora to them, or antifungal drugs. Enzyme preparations can be used to liquefy the pus and improve its drainage.
In the remission stage of chronic sinusitis, children are recommended to undergo physiotherapeutic treatment methods (mud therapy, microwave currents). For cystic, polypous and hyperplastic forms of the disease, physiotherapy is contraindicated.
Pumping out pus from the maxillary sinuses
If conservative treatment of exudative forms is ineffective, as well as mixed or polypous forms of the disease, surgical treatment is performed. Most often, radical operations are performed, the purpose of which is to form an artificial anastomosis between the maxillary and nasal cavities (methods according to Dliker - Ivanov, Caldwell - Luke).
Possible consequences and complications
Sinusitis in children, especially in the absence of timely and adequate treatment, can lead to the development of a number of serious complications:
- keratitis, conjunctivitis;
- orbital cellulitis;
- optic neuritis;
- periostitis of the orbit;
- edema, abscess of retrobulbar tissue;
- panophthalmos (inflammation of all membranes and tissues of the eyeball);
- arachnoiditis;
- meningitis;
- brain abscess;
- thrombophlebitis of the superior longitudinal or cavernous sinus;
- septic cavernous thrombosis.
Chronic sinusitis in children often causes blockage of the mucous glands, resulting in the formation of small pseudocysts and true cysts of the maxillary sinus.
Prevention methods
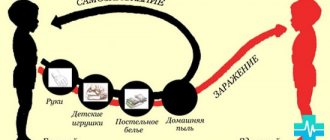
Sinusitis occurs in children with weakened immune systems. To prevent the disease, it is necessary to take care of the child’s health and strengthen it:
- promptly treat any infectious diseases;
- provide a balanced diet;
- spend more time outdoors;
- if possible, relax on the seaside in the summer;
- in the off-season and winter, give vitamin complexes and antiviral drugs.
The consequences of sinusitis can affect the most important organs of the child. Correct and timely treatment, selected by an otolaryngologist, significantly reduces the risk of complications.