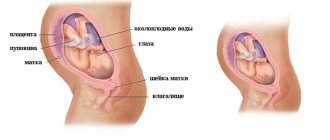
The 23rd week of pregnancy (5 months and 3 weeks) is the second trimester of gestation. A woman’s physical capabilities gradually become less due to weight gain, the growth of the child, and the pressure of the uterine fundus on the internal organs. Habitual daily activity causes rapid fatigue, which forces the pregnant woman to reconsider her daily routine. The baby continues to gain weight, actively moves in the uterine cavity, pushes and reacts to external stimuli. The feeling of a child in the womb forms a woman's maternal instinct.
Fetal development at 23 weeks of gestation
- Now the child’s weight is about 0.5 kg, and his height can reach up to 29 cm.
- The 23rd week of pregnancy is characterized by active growth of the fetal brain. From just 2 to 5 months, the brain increased in size 10 times. At the moment, his weight is about 24 g, and over the next two weeks he will weigh another 5 times. Therefore, it is so important that the baby does not experience oxygen starvation, which can negatively affect brain development. Taking this factor into account, a woman should spend as much time as possible outdoors, taking daily walks. In addition, you need to try to protect yourself from stressful situations as much as possible.
- By week 23, the baby’s digestive tract is fully formed. He has his own stomach, liver, esophagus, pancreas, and intestines. Moreover, this whole complex system is already working. The child constantly swallows amniotic fluid, making about 60 respiratory movements per minute. Sometimes the baby even hiccups, which is quite clearly felt by the expectant mother. The pancreas, which produces insulin, continues to actively develop.
- After the amniotic fluid enters the fetal esophagus, sugar and water are synthesized from it. The baby's first stool, meconium, is formed from sugars, which will also consist of bile.
- The baby's skin is covered with wrinkles, it has not yet smoothed out. The first brown fat began to accumulate under it. Lanugo - the hairs that cover the body of the fetus - darken at this stage.
- Gradually, nails form on the tips of the fingers.
- At 23 weeks, the spleen begins to function for the first time. It produces red blood cells and destroys those that turn out to be “poor quality”.
- Boys have formed a scrotum, and girls have ovaries, which already contain millions of eggs needed to produce their own offspring.
- Most scientists are of the opinion that the baby begins to see his first dreams precisely from the 23rd week of intrauterine life. Although the baby sleeps most of the time, he wakes briefly every hour.
Recommendations
In the 2nd trimester of pregnancy, a woman’s appetite increases, which often leads to gaining extra pounds. To prevent weight gain, it is important to properly plan your diet. Food should be taken in small portions 5-6 times a day to improve metabolic processes in the body. The calorie content of the daily diet should not exceed 2700-3000 kcal.
The diet includes fruits, vegetables, herbs, cereals, dairy products, lean meat, and fish. Red meat contains heme iron, which prevents the development of anemia. Drinking regime is no less important than nutrition. You should drink up to 2 liters of liquid per day if you are not prone to swelling. It is recommended to drink still water before each meal, which reduces the amount of food eaten and reduces appetite.
Regular physical activity is necessary for normal fetal development. Doctors recommend water aerobics, fitness for pregnant women, and walking at a leisurely pace. It is important to choose comfortable clothes that do not restrict movement, and shoes with low heels of 1-3 cm. Special clothing for pregnant women meets all hygiene requirements at this stage of gestation.
To relieve the lumbar spine and reduce the pressure of the uterus on the internal organs, you can wear a prenatal bandage. To prevent the appearance of stretch marks on the body, it is recommended to use special creams and gels. For the comfort of the mammary glands, it is necessary to wear a bodice made of natural fabric. If colostrum leaks, use nipple pads.
The 23rd week of pregnancy is another step that brings a woman closer to childbirth, and prepares the child for life outside the womb. Following a daily routine and diet, a scheduled visit to an obstetrician-gynecologist, and wearing a prenatal bandage will help you get through this period without developing complications.
What happens to the expectant mother?
At 23 weeks of pregnancy, a woman fully feels the movements of the fetus. If earlier they could be confused with the work of the intestines, now all doubts fade into the background - the child is really moving. As a rule, the fetus is most active in the evenings and at night. Now you can try to “calm” him down by talking to the child in a quiet and even voice, or by singing him a lullaby. At the same time, you can lightly stroke your stomach.
The expectant mother is worried about heartburn, because the growing belly begins to put pressure on the stomach. To reduce discomfort, it is recommended to drink a glass of milk, eat a few shares of quality chocolate or chew sunflower seeds. Soda should not be used to relieve heartburn. Its use will lead to the fact that the unpleasant feeling will only intensify and begin to occur more often.
At the 23rd week of pregnancy, a woman experiences certain breathing difficulties, which are understandable. They occur due to the fact that the enlarged uterus puts pressure on the diaphragm, compresses the lungs and expands the sternum. Although there is nothing critical in this, you need to try to master special breathing techniques that will allow you to fully provide your body and your child with oxygen.
More frequent trips to the toilet to empty the bladder. Moreover, as pregnancy progresses, the pressure on this organ will increase. To prevent the desire to urinate from bothering you at night, you need to limit the amount of liquid you drink after six o’clock in the evening.
It is possible that in the morning a woman will experience slight swelling as the body retains excess fluid in order to provide the placenta with it if necessary. When swelling becomes very severe, you need to reduce your salt intake, but you shouldn’t give it up completely.
Hormonal surges that occur in the body every day can cause the skin of the hands to periodically turn red. There is no need to worry about this, as everything will pass soon.
Body skin may become drier and begin to peel. Stretch marks often appear on it. To reduce discomfort, you need to use special moisturizing creams.
It is equally important to keep the breasts clean, because the first colostrum may already begin to be released from it. Teeth need special care, as calcium consumption increases. Insufficient oral hygiene can lead to deterioration of tooth enamel.
Many women note that their hair becomes thicker and healthier during pregnancy. The fact is that the blood supply to all organs increases, so the hair follicles receive more nutrients. However, you should be prepared for the fact that after childbirth your hair may thin out.
Sweating increases, which often causes acne and other skin defects. To avoid this, it is necessary to wipe problem areas with antiseptics. Regular showering will help combat the unpleasant odor.
Changes in the body
The uterus rises and puts pressure on the internal organs.
The uterus grows - it rises 3.5–4 cm above the navel. The height of the uterine fundus (from the pubis to the upper border) is about 23 cm. The woman’s body weight also increases - by this time she adds 5–7 kg. The norm for weight gain is now considered to be 400–800 g per week. The following symptoms may be bothering you right now:
- Swelling. Minor swelling of the extremities is acceptable. You should be wary of intense and frequent swelling, large weight gain associated with fluid retention in the body. To avoid this condition, limit your salt intake and rest with your feet up.
- Varicose veins The increased mass of the uterus, combined with a large volume of blood circulating in the body, creates a load on the vessels, spider veins may appear on the legs, and veins may “pop out.” It is worth visiting a phlebologist, as well as increasing physical activity and wearing compression garments.
- Cramps of the calf muscles. Quite a common occurrence during pregnancy. Usually caused by calcium deficiency and is more common at night. It is recommended to massage the foot, straighten the leg and pull the toes towards you. To eliminate this symptom, the doctor may prescribe or increase the dosage of calcium supplement taken by the mother.
- Dark spots. A dark stripe may appear longitudinally across the abdomen, and the nipples may darken. Pigment spots often appear on the face. Usually this problem goes away on its own after childbirth.
- Stretch marks. Now the belly is already quite large, and subsequently it will grow even faster than before. To prevent stretch marks from appearing due to excessive stretching of the skin, use special creams for expectant mothers, rub the skin with a washcloth while bathing, and control weight gain.
- Heartburn, constipation. Digestive problems are caused by the pressure of the heavier uterus on the intestines and esophagus. To minimize these problems, try to eat small meals, eat healthy foods prepared in a gentle way, and move more during the day.
The mother’s emotional background is most likely stable - the body is accustomed to changes in hormonal levels, but unreasonable sadness and outbursts of irritability may periodically occur. Try to tune in to a positive mood, think only about pleasant things, receive positive emotions, because a bad mood and experiences negatively affect the baby in the womb.
Fetal movements at this stage are felt quite clearly. At the same time, the frequency of active movements is individual, depending on the activity of the mother, her sensitivity to touches from the inside. It is known that the fetus sleeps up to 20 hours a day at this stage. You should be wary if you do not feel any movement within 24 hours. However, if the doctor hears the fetal heartbeat at the appointment, there is no reason to worry, everything is fine with the baby. The baby may hiccup in the womb, and frequent “trembling” of the abdomen is felt. Don't worry, hiccups are caused by swallowing amniotic fluid and are not a cause for alarm.
Pain
Pain can occur due to being in one position for a long time.
Already now the uterus can begin to prepare for childbirth. This manifests itself in the form of so-called training contractions. You may feel a mild nagging pain in the abdomen, radiating to the lower back, which goes away on its own. To ease the condition, lie on your left side and rest. Normally, false contractions occur rarely and are short-lived. If you feel this condition more than 5 times in an hour, or the pain is sharp, sharp, you should consult a doctor - perhaps this is a sign of the onset of premature labor.
Due to the load on the spine, the lower back may hurt. At this stage, the pelvic bones begin to move apart in preparation for the upcoming birth, which can also cause discomfort. Choose comfortable shoes without heels to avoid falls due to poor coordination.
Painful sensations can also occur in the abdominal area, usually due to tension in the ligaments. If the uterus is relaxed, and most often the pain is felt with sudden movements, there is no need to worry. To alleviate the condition, it is recommended to wear a prenatal bandage, which will relieve stress from both the abdominal muscles and the back. If pain is caused by the baby’s movements in the womb, and at the appointment the doctor notes a lag in the growth of the uterine fundus, oligohydramnios most likely develops. This condition is dangerous and can lead to premature birth; constant medical monitoring is required.
Discharge
Unusual vaginal discharge accompanied by abdominal pain is a warning sign.
Translucent or whitish mucous vaginal discharge is considered normal. They have almost no smell or have a slightly sour smell. The consistency is homogeneous, without lumps or any inclusions. Their volume may increase slightly compared to the previous period, or remain the same. Excessively thin, transparent discharge may be a sign of water leakage. Purulent discharge (yellow, gray, green) with an unpleasant odor is a symptom of an infection or inflammatory process. Curdled discharge with a pungent sour-milk odor is often a manifestation of thrush. To diagnose the disease, it is necessary to take a vaginal smear, and then undergo appropriate treatment according to the doctor’s recommendations.
Bloody or brown discharge should also alert you. They can be caused by a variety of reasons, including:
- premature birth;
- placental abruption;
- frozen pregnancy;
- cervical erosion and others.
If the bleeding is profuse and accompanied by pain, you should immediately call an ambulance.
Stomach
The shape and size of the abdomen do not depend on the sex of the fetus.
The size and shape of the abdomen of the expectant mother depend on many factors, including:
- placenta attachment site;
- position of the fetus in the womb;
- number of fruits;
- mother's physique;
- the size of the future baby.
It is known that during repeated pregnancy, as well as when carrying twins, the belly grows faster than in other cases. Fat mothers can keep their position a secret longer than thin mothers. Popular beliefs linking the shape of the abdomen with the gender of the child do not find scientific confirmation. The tummy can be pointed in case of cephalic presentation, attachment of the placenta along the anterior wall. A wide belly is observed with a transverse position of the fetus, in obese mothers. If you have polyhydramnios or a large fetus, or if you are carrying twins, your belly may seem too large.
Photo gallery: bellies at 23 weeks
Take photos regularly to monitor your belly growth
Travel is not prohibited if the pregnancy is going smoothly
Try to wear clothes that do not put pressure on your stomach
Causes of pain at 23 weeks
At 23 weeks of pregnancy, a woman may begin to experience pain in the back. The load on the lower back and the spine as a whole increases. Pain is also caused by the expansion of the pelvic bones, which is aimed at facilitating the passage of the child through the birth canal.
Sometimes leg cramps may occur. This is especially true against the background of a lack of calcium in the body, so its reserves must be replenished daily. The doctor may recommend that the woman take calcium supplements.
Since the center of gravity shifts to the stomach, a woman needs to be especially careful. Even familiar actions need to be performed more carefully, for example, getting out of bed, bending over and squatting.
You should stop wearing high-heeled shoes. This is not only unsafe, but also puts increased stress on your back.
When sleeping, it is best to lie on your side. Sleeping on the stomach is uncomfortable due to its impressive size, and sleeping on the back is not recommended due to the possible deterioration of blood supply to the placenta in this position.
The abdomen may hurt due to muscle tension, which is especially felt during sudden movements, as well as when coughing and sneezing.
Wearing a prenatal bandage helps reduce the load on your back and maintain correct posture. To choose the right product, you should consult your doctor.
What's happening to the stomach?
The appearance of the abdomen changes, with a dark stripe often appearing down the center from the navel to the pubic area. This happens because a pregnant woman's body produces a lot of melanin. Sometimes this also leads to darkening of the nipple areolas and increased pigmentation of the vulva. As a rule, after childbirth everything returns to normal.
The skin of the abdomen may begin to itch due to its tension. Olive oil can be used as a natural moisturizer.
A cause for concern should definitely be severe cramping pain in the abdomen and lower back, which occurs against the background of vaginal discharge with blood, fainting, fever and vomiting. In this case, it is necessary to call an ambulance as quickly as possible.
Possible problems
Mom needs to carefully monitor her well-being, regularly visit a doctor, and undergo routine medical examinations. This is necessary for the prevention, timely detection and correction of possible pregnancy complications. Let's take a closer look at these dangerous conditions.
Preeclampsia
Excessive weight gain while following a diet may indicate internal edema.
This condition is also called late toxicosis. It is characterized by deterioration of the functioning of internal organs and systems caused by pregnancy. Preeclampsia is diagnosed only during pregnancy, and after childbirth the body’s condition usually stabilizes. Preeclampsia occurs in approximately 1/3 of expectant mothers, most often occurring during the first pregnancy, in the third trimester. At week 23, symptoms of the disease may appear for the first time. It is believed that the sooner this happens, the worse the condition will be before childbirth, and the greater the negative impact gestosis will have on the baby in the later stages.
Scientists are unable to reliably identify the causes of the development of gestosis. According to one theory, the disease is provoked by the placenta, which increases blood pressure in the body, which negatively affects the functioning of organs and systems. Preeclampsia often develops against the background of existing chronic diseases. There are several forms of gestosis:
- Early gestosis, or dropsy of pregnancy. It manifests itself as swelling of the extremities, internal fluid retention in the tissues.
- Nephropathy. This is the next stage, developing against the background of edema. The kidneys cannot cope with the increased load, and blood pressure rises.
- Preeclampsia. In addition to edema and high blood pressure, protein is detected in a urine test. Headaches, nausea, blurred vision, and fainting may occur.
- Eclampsia. The most undesirable condition, most often diagnosed in the later stages of pregnancy. Symptoms include seizures and disruption of internal organs, which can lead to a stroke. Eclampsia often leads to placental abruption, premature birth, hypoxia and even fetal death.
It is impossible to completely cure gestosis; the task of doctors is to reduce the intensity of symptoms and stabilize the well-being and functioning of internal organs. A diet is prescribed with limited salt and water intake, herbal sedatives, and mild diuretics. Depending on the form of the disease, treatment is prescribed with appropriate drugs that lower blood pressure, normalize blood flow, and prevent the development of placental insufficiency. A woman is recommended to take vitamins, follow a diet, and constantly monitor edema and blood pressure. In complex forms, gestosis can only be treated in a hospital.
Hypertonicity of the uterus
Doctors use this term to describe painful contractions of the uterus, accompanied by nagging pain in the lower abdomen and back. Women feel “petrification”, heaviness in the stomach. This condition cannot be ignored, since in the absence of proper treatment, hypertonicity can lead to premature birth, impaired blood supply to the placenta, and intrauterine fetal hypoxia.
The causes of hypertension can be:
- hormonal deficiency;
- malformations of the organs of the reproductive system;
- uterine fibroids;
- infections and inflammatory processes of the reproductive system;
- short cervix;
- previous miscarriages, abortions and others.
To correct this condition, the doctor prescribes magnesium, vitamin B6, sedatives, and antispasmodics. It is required to limit physical activity and refuse sex. Bed rest is recommended. In many cases, doctors recommend inpatient treatment for uterine hypertonicity.
Premature birth
In earlier stages, spontaneous termination of pregnancy was called miscarriage, but now it is premature birth. According to international standards, births occurring between 22 and 28 weeks are considered very early preterm birth.
The reasons may be:
- hormonal disorders;
- infectious diseases (primarily the reproductive system);
- malformations of the uterus (one-horned, two-horned, underdeveloped, damaged);
- isthmic-cervical insufficiency (the cervix is not able to withstand the load of the uterus and opens prematurely);
- fetal malformations;
- fetal chromosomal abnormalities;
- placental insufficiency;
- gestosis;
- high or low water levels;
- injuries;
- excessive physical activity, stress;
- premature rupture of water and others.
If the baby was born due to premature birth at the 23rd week, most likely it will not be possible to save him. The organs are formed, but not yet mature and are not able to function outside the mother's womb. There are only a few survivors of this case in the world, but all of them have serious health problems. Babies born at least 2-3 weeks later have a much greater chance of survival.
The main symptoms of premature birth:
- sharp cramping pain in the abdomen, radiating to the back;
- discharge of mucus plug, amniotic fluid;
- bleeding from the vagina.
In many cases, the process of premature birth can be stopped in time if the amniotic sac has not opened and the placenta has not completely separated. The sooner you see a doctor if you feel alarming symptoms, the higher the likelihood of carrying and giving birth to a healthy baby.
What happens to the uterus?
Now the uterus rises above the navel by 4 cm. From time to time it may contract slightly, training for the upcoming birth. Sometimes this process is accompanied by the appearance of mild pain. Such training contractions do not last long, and sometimes they are isolated. They are also called Braxton-Higgs contractions. They may intensify after intimacy. To reduce the intensity of such contractions, you need to change body positions, and it is better to lie on your side.
Training contractions should not increase or cause intense painful sensations. If they become frequent, then you need to call an ambulance.
Is it necessary to do an ultrasound at 23 weeks of pregnancy?
The second planned ultrasound examination can be scheduled precisely at the 23rd week of pregnancy. During an ultrasound, the doctor will evaluate the development of the fetus, its motor activity, heartbeat and other important indicators. At the same time, the uterus and placenta are examined. Sometimes the doctor indicates that the placenta is located lower than it should be. There is no need to worry about this, it can rise, since the uterus will still grow and expand.
An ultrasound performed at the 23rd week of pregnancy will determine the sex of the unborn child if the baby does not turn his butt towards the sensor. However, you can never be 100% sure on this issue, since errors occur even when conducting research using the most modern equipment.
Determining the deadline
You are already an experienced expectant mother; many examinations, ultrasounds, and tests have been carried out. Surely you already know that doctors count the pregnancy period from the first day of menstruation preceding conception. Based on this method of determining the gestation period, doctors evaluate test results, the development of the child using ultrasound, and determine the preliminary date of birth. So, the 23rd obstetric week of pregnancy is:
- five months of pregnancy;
- second trimester;
- approximately 21 embryonic weeks (from the day of conception).
What tests should be taken at 23 weeks?
At 23 weeks, a woman may have a doctor's appointment, so she will need to undergo certain tests. It is possible that she received a referral to them even earlier. Most often, the results of a general blood and urine test are required, as well as a blood test for sugar, coagulation, levels of hCG and other hormones.
If protein and salts are detected in the urine, it will be necessary to undergo a number of additional studies, since these data may indicate an infection, disturbances in fetal development, etc. The level of human chorionic gonadotropin and progesterone in the blood is of no small importance. Therefore, if any abnormalities are detected, the doctor will prescribe additional tests.
If your blood sugar level is high, you will need to stick to a diet, as the risk of excess weight in the fetus increases. It is possible that a woman in this case may require specific therapy.
Equally important is monitoring the level of hemoglobin in the blood, which allows for timely detection of iron deficiency anemia. It very often develops in pregnant women and causes health problems.
It should be understood that on the basis of any one “bad” analysis, the doctor will not be able to make a diagnosis of this or that problem. As a rule, pathology will be indicated by deviations from the norm in several indicators at once. Therefore, there is no need to worry in advance.
Discharge: norm and pathology
Normally, discharge at the 23rd week of pregnancy should be light milky in color, odorless and foreign inclusions. Any deviations must be reported to the doctor. Signs of ill health are a change in the color of the discharge to yellow, green, earthy, brown, etc. The presence of curdled clots, flakes or foam in the discharge indicates the addition of an infection. It must be treated, since many of the pathogenic microbes are able to overcome the placental barrier and infect the child’s body.
Thrush is a fairly common occurrence during pregnancy. It is indicated by cheesy discharge and severe itching of the skin of the external genitalia. Candidiasis must be treated, otherwise there is a risk of infection of the child during its passage through the birth canal.
A woman should carefully monitor the nature of her discharge to notice possible leakage of amniotic fluid. If such a problem occurs, you should seek medical help as quickly as possible. If you suspect water leakage, you don’t have to worry about guessing; just go to the pharmacy and purchase a special test to detect amniotic fluid.
At 23 weeks of pregnancy, the risk of miscarriage is significantly reduced compared to the first trimester. However, if bleeding occurs, it is necessary to call an ambulance as quickly as possible. The presence of blood may indicate cervical erosion; such discharge may occur after sexual intercourse or a gynecological examination. In any case, consulting a specialist will not hurt.
Visit to the doctor
Tell your doctor about any problems with your health.
Continue to follow your schedule of visits to the gynecologist monitoring your pregnancy. Usually during this period the doctor is visited 2 times a month. The day before, or 1–2 days before the appointment, the woman needs to bring urine samples for analysis to the laboratory. This is necessary for the timely detection of inflammatory processes in the genitourinary system and abnormalities in the functioning of the kidneys. The cause for alarm in this case is the identification of salts and protein in urine.
At the doctor's appointment:
- measures blood pressure;
- weighs the patient;
- determines the height of the uterine fundus (at this stage the norm is 21–24 cm);
- examines limbs for swelling;
- listens to the fetal heartbeat using a stethoscope;
- evaluates test results;
- if necessary, prescribes medications to stabilize the mother’s well-being.
If abnormalities in a biochemical blood test were previously detected, the doctor may issue a referral for a repeat laboratory test. For example, to the level:
- glucose (if gestational diabetes is suspected);
- hemoglobin (for anemia);
- hCG (if there is a threat of premature birth);
- blood clotting (with placental abruption);
- progesterone and others (for hormonal deficiency);
- antibodies to the Rh factor (in case of Rh conflict between the blood of mother and fetus) and others.
If you are pregnant with twins, special medical supervision is required - visit your doctor weekly.
What will an ultrasound show?
In the ultrasound image, the contours of the baby’s body are clearly visible.
An ultrasound examination can be prescribed for the mother at the 23rd week. The procedure is considered safe for mother and baby and is performed 3-4 times during the entire gestation period, or more often if necessary. With the help of ultrasound, doctors are able to confirm or refute various complications of pregnancy and monitor the development of the fetus in accordance with the gestational age. The fetus is already fully formed, but its organs and systems continue to improve and prepare for existence outside the womb. At the 23rd week, the baby can already take the correct position in the uterus - head position (legs up). However, if this has not happened yet, there is still some time for a coup. Breech presentation is considered undesirable - it complicates the birth process and may become an indication for cesarean section. The baby, as a rule, no longer lies transversely - he is quite large, and in this position it is cramped for him. Height and weight indicators are now not as significant as before, because small deviations can be associated with the individual characteristics of the baby and hereditary factors. Not only the baby is examined, but also the uterus, cervix, umbilical cord, and placenta.
The following parameters require special attention:
- brain activity (if the ventricles of the brain expand, the doctor will suspect hydrocephalus - dropsy);
- heart rate (normally about 160 beats per minute);
- position of the fetus in the womb (pelvic, transverse, cephalic);
- weight (about 500 g) and height (about 25–28 cm);
- biparietal size - diameter of the head from temple to temple (52–64 mm);
- head circumference (19–22 mm);
- fronto-occipital size (67–81 mm);
- abdominal circumference (approximately 17–20 mm);
- femur length (38–42 mm);
- humerus length (34–42 mm).
The condition of the placenta is assessed separately - its thickness, structure, location. Maturity at this stage must correspond to 0, otherwise this organ ages prematurely. The woman's pelvic organs are examined - the cervix, internal os (should now be closed). The transparency and amount of amniotic fluid is assessed. Too turbid water can be a sign of infection; if there is a small amount of it, oligohydramnios is determined, and if it is too much, it is polyhydramnios.
At the 23rd week, Doppler ultrasound is performed during an ultrasound - a procedure that allows you to assess the quality of blood flow between the mother and the baby. The following indicators are considered normal:
- resistive index of the umbilical artery (IR) – 0.6–0.8;
- IR of the uterine arteries - 0.36–0.68;
- systolic-diastolic ratio inside the umbilical artery (SOR) – 3.4–3.61;
- SDO of the internal carotid artery - 0.94;
- SDO of the uterine artery - 1.95;
- IR VSA – 0.93 – 0.95;
- blood flow speed inside the fetal aorta is 25.62 – 27.7 cm/s.
At this stage, it is possible to determine the sex of the fetus with 100% accuracy if the visualization is good and the genitals are not hidden behind other parts of the baby’s body. The contours of the baby are visible even to the naked eye, and during the procedure the baby can sleep, suck a finger, yawn or move in the uterus.
Is it possible to have sex?
If the doctor does not indicate the presence of any contraindications to intimate life, then sex at 23 weeks of pregnancy is permitted. Moreover, it can give a woman special pleasure, since the sensitivity of the erogenous zones at this time increases and libido increases.
Doctors strongly recommend that women do not change sexual partners during pregnancy in order to reduce the risk of developing dangerous infections that can harm not only the woman, but also the child. Moreover, the vaginal microflora at this time becomes especially sensitive to foreign bacteria.
Whatever types of sex spouses practice, the main thing is to be careful. During intimacy, a woman should not experience pain or discomfort. Poses should be chosen that do not involve pressure on the stomach.
If a woman has previously suffered a miscarriage, or in the case when she is carrying twins, doctors strongly recommend refusing intimacy. Other contraindications include placenta previa and the threat of premature birth.
Principles of proper nutrition
- Protein predominates in a pregnant woman's menu. However, this does not mean that you need to give up fats and carbohydrates. First of all, the diet should be balanced.
- The menu should include fresh fruits and vegetables every day.
- Calcium-rich foods must be present on the table - fermented milk drinks, cottage cheese, oatmeal.
- You need to remove spicy, pickled, salted, fried and smoked foods from your diet.
- Fresh water should remain your main drink throughout the day. You can also drink fruit drinks, compotes, juices, but you need to be careful with herbal infusions.
- When you want sweets, it is best to replace chocolate and sweets with nuts and dried fruits. You should not get carried away with them, as they are high in calories and can contribute to weight gain.
Video about proper nutrition in the second half of pregnancy. How to prevent anemia? Mother's nutrition in the second trimester is just as important for the child as at the beginning of the term. You supply your baby with the necessary elements for his rapid growth and further development:
Reviews from mothers about the 23rd week
And we're at 23 weeks. Pregnancy 1, 37 years. They did 2 ultrasounds, the fetus is developing well, blood flow is normal, but the placenta has a heterogeneous structure, after a week in the uterus, they will most likely be sent to a day hospital for injections, tablets and droppers. There was no toxicosis or heartburn, sometimes there is a tone, but it goes away quickly. Our boy is kicking as hard as he can.
Guest
https://mamapedia.com.ua/forum/v-ozidanii-chuda/calendar-beremennosti/23-week-beremennosti.html
23 weeks, I feel absolutely pregnant! ))) I’m finally “bloated”, such a watermelon has grown over the last couple of weeks, and before that there was no belly at all, although on an ultrasound the weight is developing normally... the baby pushes, but only when I’m in a relaxed state... during there is no such day, I’m always worried, waiting for the evening, I already know that as soon as I sit on the sofa, I’ll give my legs a rest, turn on a movie and she comes to life - playing, kicking... There was no toxicosis, no heartburn, except for a couple of times in the evening after a hearty meal dinner))
Guest
https://mamapedia.com.ua/forum/v-ozidanii-chuda/calendar-beremennosti/23-week-beremennosti.html#p=7
I'm now 23 weeks. And only now I finally felt that I was pregnant. It became a little difficult to walk and lie on my stomach. Laziness, drowsiness, and passivity appeared. My baby is kicking. He began to respond to my touches. Dad and I love him very much and are waiting for him! We are very happy when he “gurgles” inside.
Guest_MILEN
https://www.kid.ru/forum/index.php?showtopic=42
I’m also 23, and I’ve gained 6 kg, so I can’t even see my tummy!!! My husband says I'm faking it! More precisely, he said it until he felt how the baby was rowdy! And when will the belly be visible? I’m still running slim and I don’t experience any discomfort... Although I’ve been moving since 15 weeks? And everything seems to be developing well!
Katya
https://www.kid.ru/forum/index.php?s=8049419baf31bbdcefae5c8fa3ace0d0&showtopic=42&st=15
In the morning I wake up, the baby also wakes up, kicks, pushes. While we are driving to work, it can also push several times. less during the working day, but from time to time I still feel it. The next active period is after lunch, fussing and fussing, then quiet. In the evening we come home from work, go to bed for 10 minutes, it starts to rustle again))) Well, the most active time is before bed, somewhere from 22 to 12 at night
Patient
https://deti.mail.ru/forum/v_ozhidanii_chuda/beremennost/shevelenija_na_23_nedeli/
And we just started our 23rd week, although at the ultrasound at 21.4 weeks we already weighed 493 grams)) And they put us 1.1 weeks longer. We are big))
Daria
https://baby63.ru/forum/14–26–1
Answers to popular questions
- I am 23 weeks pregnant, and recently I began to notice that sticky spots appear on my bra, and my nipples always seem to be covered with a greasy coating. What it is?
Colostrum may be released from the breast at 23 weeks of pregnancy, since its production began at 16 weeks. Most often, women notice the first marks on clothes at 32 weeks of pregnancy and later. However, if colostrum appeared earlier, there is nothing to worry about. You just need to wash your breasts more often with warm water, and then gently pat them dry with a towel. You should not specifically put pressure on your breasts or try to express colostrum, as this can trigger the onset of premature labor. A woman must remember that colostrum is a fertile environment for the proliferation of bacterial microorganisms, so hygiene must be especially careful.
- How does toxicosis manifest itself at 23 weeks of pregnancy? Is it true that it manifests itself in dizziness?
Toxicosis in late pregnancy is expressed in increased swelling, the appearance of traces of protein in the urine, fluctuations in blood pressure, headaches and visual impairment. Therefore, when you feel dizzy and have at least one of the listed signs, you need to urgently contact a medical facility. Late toxicosis, or gestosis, can lead to serious problems - preeclampsia and eclampsia.
Author of the article: Lapikova Valentina Vladimirovna | Gynecologist, reproductive specialist
Education: Diploma in Obstetrics and Gynecology received from the Russian State Medical University of the Federal Agency for Health and Social Development (2010). In 2013, she completed her postgraduate studies at NIMU named after. N.I. Pirogova.
Our authors