Forms and classifications of gastritis
Gastritis is a disease of the gastrointestinal tract associated with disruption of normal processes in the gastric mucosa. There are acute and chronic forms. The acute form is the first manifestation of the disease. Chronic - regularly recurring cases of violations.
Acute, in turn, is divided into:
- Catarrhal - a simple form caused by lack of a healthy diet or food poisoning.
- Fibrous is a secondary form that accompanies complex infectious diseases.
- Phlegmonous is a complication of stomach cancer or ulcers.
- Corrosive - a form caused by poisoning with alkalis, acids, poisons, and heavy metal compounds.
Chronic gastritis happens:
- Autoimmune - gastritis, inherited or as a result of autoimmune disorders in the body.
- Chemical - gastritis, which develops as a result of the backflow of the contents of the duodenum into the stomach.
- Bacterial - gastritis caused by the bacterium Helicobacter Pylori.
According to morphological characteristics, chronic gastritis is:
- Superficial.
- With damage to the glands without atrophy.
- Atrophic.
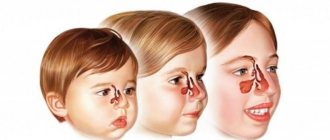
Signs of acute gastritis in a child
Gastritis in a child (symptoms and treatment are closely interrelated) begins with the manifestation of signs of the disease.
The acute form is characterized by:
- general poor health;
- cramps in the stomach;
- feeling of heaviness in the stomach;
- dizziness;
- nausea;
- heartburn;
- vomiting (sometimes with blood);
- diarrhea.
The main signs of gastritis or how to identify the disease
In order to determine the development of the disease in time and begin treatment, parents should know the main symptoms of gastritis. The child may not show absolutely all the symptoms, but even 1-2 signs characteristic of this disease should cause concern among parents. Of course, some symptoms in most cases are observed in other diseases, but they should not be ignored:
- restless behavior, incessant crying for no particular reason, sleep disturbance, lethargy;
- abdominal pain, loss of appetite;
- the appearance of bruises under the eyes, pale skin;
- coating on the tongue;
- diarrhea, nausea and vomiting;
- drying of the mucous membranes of the mouth, increased salivation;
- chills and fever.
General signs of chronic gastritis in children
Chronic gastritis is characterized by regular manifestations. Therefore, based on the child’s equally recurring symptoms, this diagnosis can be assumed. But in any case, treatment is prescribed strictly by a gastroenterologist.
A visit to him is required if the following symptoms occur:
- belching with a sour smell;
- periodic bowel dysfunction;
- decreased appetite;
- increased gas formation;
- vomiting without signs of poisoning;
- white coating on the tongue;
- smell from the mouth.
Correct treatment of gastritis in children
For treatment of the disease to be effective, you must first find out what caused gastritis.
The main condition for treating this disease is to create a favorable atmosphere for the child so that his life can pass without stress and conflicts. The baby’s nutrition also plays an important role. It is advisable that the baby has an organized diet, that is, he should eat at the same time.
Treatment with medications is carried out only in a hospital setting.
Self-treatment at home is not allowed, since the disease can become chronic.
In the hospital, specialists select effective medications on an individual basis, and also carry out physiotherapeutic treatment, which eliminates pain and improves the recovery process of the gastric mucosa.
Specifics of manifestation of the atrophic form of gastritis
Gastritis in a child (symptoms and treatment are described later in the article) can take the most severe form - when atrophy of the gastric glands occurs. This is atrophic gastritis. Its severity lies in the fact that the disease is asymptomatic in the initial stages. And only when the work of the glands stops completely does the child begin to complain of feeling unwell.
Symptoms of the disease are:
- decreased appetite;
- constant belching after eating;
- rumbling and gurgling in the stomach;
- regular bowel dysfunction;
- weakness;
- heaviness in the epigastric region;
- vomit.
Over time, as a result of gland atrophy, the process of absorption of vitamins and nutrients in the mucous membrane of the stomach and intestines stops, which leads to poor vision, hair loss, brittle nails and teeth.
The hydrobalance of the skin is disrupted, and dehydration may occur. Often, with the atrophic form of gastritis, tumors form in the stomach of children, which is why this type is also called precancerous.
The causes of atrophic gastritis are impaired diet. The child’s stomach is not able to cope with fatty or heavy foods, and this provokes gland atrophy. Another cause is the bacterium Helicobacter Pylori.
Modern diagnostic methods make it possible to quickly and accurately diagnose this disease. The most commonly used method is endoscopic examination. At an early stage, atrophic gastritis can be successfully treated. The basic principle of treatment combines drug therapy with a gentle diet.
Causes of gastritis in children
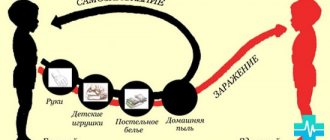
Recently, scientists have proven that gastritis is a contagious disease that can be transmitted through household and airborne transmission. This became clear after the discovery of the main pathogen - the bacterium Helicobacter Pylori.
Of course, there are other causes of the disease:
- unbalanced or unhealthy diet;
- stress or disturbance of the child’s psycho-emotional background;
- physical activity and fatigue;
- infectious cause (after suffering a severe infection);
- disturbance in autoimmune processes;
- genetic predisposition;
- side effects of strong medications.
Causes
Taking into account age-related physiology, it is possible to form a risk group, which includes children who have a high probability of developing gastritis. The most common cause is nutritional disorders:
- irregular feeding, increasing intervals between meals up to 5 hours or more;
- lack of proper control, permission to eat harmful fast food products prepared under dubious conditions by frying or smoking (burgers, French fries, chips), drinking spiced crackers with sweet carbonated drinks that use harmful dyes;
- consumption of poor quality food purchased at kiosks or stores with expired shelf life;
- eating contaminated food in public canteens if the process of culinary processing and storage of food is carried out improperly.
Children don't realize that something tasty can be dangerous.
This proves that as a child grows up, he needs food control, training in the rules of independent choice and hygiene. Psycho-emotional overload with the start of school activities increases children’s sensitivity to environmental aggression. The regulating function of the nervous system for the production of gastric juice and appetite are disrupted.
The consequence may be inflammation in the stomach. Both increased physical activity and insufficient mobility are equally harmful. They disrupt blood circulation and disrupt immune defenses. Helicobacter infection plays a role in the development of chronic gastritis.
The microorganism reproduces quite well in conditions of high acidity. Children with hypersecretion of gastric juice are most sensitive. Acute gastritis can be caused by:
- any food products, nutritional mixtures during the infant period;
- contaminated dishes for older children;
- accidental ingestion of medications, cleaning products, and pesticides by a small child.
Children's bodies have a hard time dealing with toxic substances and infections. He is not able to limit himself to a local response. Causes severe autoimmune inflammation, in which one’s own cells are mistaken for foreign and destroyed. This is how chronic atrophic gastritis develops in children.
Among the causes of chronic gastritis, we must not forget about the possibility of primary damage to the child’s liver, gallbladder, pancreas (hepatitis, cholecystitis, pancreatitis), and intestines. Sluggish gastritis leads to:
- food allergies;
- endocrine disorders;
- chronic infections (tonsillitis);
- long-term use of medications;
- helminth infection.
Diagnosis of gastritis in children
To correctly diagnose the disease, the following factors are considered together:
- clinical picture;
- patient complaints;
- medical history;
- genetics.
The main method of diagnosis is fibrogastroduodenoscopy (FGDS) - endoscopic examination. It consists of placing a special apparatus - a probe with a built-in camera (gastroscope) into the stomach cavity for visual examination of the mucous membrane.
A gastroscope can also perform additional functions: taking a biopsy (a piece of mucous membrane) for analysis and measuring the pH value. A biopsy is an absolutely safe and harmless analysis, but at the same time very informative. The pH-metry method allows you to determine the level of stomach acidity.
However, FGDS is a very labor-intensive process and has many contraindications for the child. Therefore, in a number of uncomplicated cases, it is more appropriate to prescribe treatment without such diagnostics. The younger the child is, the more difficult it is to carry out this procedure.
The presence of the bacterium Helicobacter Pylori in the stomach is determined by analyzing stool and a sample of the mucous membrane. There is also a blood test for antibodies to this bacterium. Ultrasound diagnostics and x-ray studies are not informative in making a diagnosis, but they can reveal accompanying diseases, such as biliary dyskinesia.
If it is impossible to use FGDS, sometimes they resort to x-rays. To do this, a person swallows a contrast agent on an empty stomach. Based on the images, the gastroenterologist evaluates the contours of the abdominal organs and makes a diagnosis.
How and how to treat various forms of gastritis in a child?
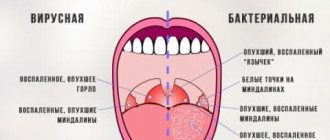
Gastritis in a child (symptoms and treatment require special attention) is not a death sentence. Full recovery depends on timely diagnosis and correct diagnosis. Due to the similarity of symptoms, it is important not to confuse gastritis with diseases of the duodenum or gallbladder.
Specifics of treatment of gastritis with high acidity
Treatment of gastritis with high acidity is aimed at normalizing the pH balance in the stomach. Combines drug therapy with non-drug methods.
Main medications for treatment:
- antibiotics to neutralize the bacteria Helicobacter Pylori;
- drugs to reduce acidity - antacids: Almagel, Phosphalugel.
- enzymes that help digestion: Creon, Festal, Pancreatin.
- drugs that reduce the production of stomach acid - Omeprazole;
- antiulcer drugs - Ranitidine;
- antiemetic drugs - Motilium;
- drugs that coat the gastric mucosa.
A gentle diet involves complete abstinence from the following foods:
- alcoholic drinks;
- fried, smoked and salted dishes;
- semi-finished products;
- hot sauces;
- onion garlic.
Allowed for consumption:
- low-fat broths;
- porridge with water;
- boiled meat;
- 2-3 day bread;
- vegetables.
All dishes must be steamed or boiled in water.
If gastritis with high acidity in a child is not treated, the symptoms can develop into a more serious disease - a stomach ulcer.
All treatment is carried out on an outpatient basis. For the treatment of chronic forms, the patient is recommended to go to hospital at least 2 times a year.
Features of therapy for gastritis with low acidity in a child
Gastritis with low acidity is a rare but dangerous phenomenon. Stomach acid contains enzymes that help food digest. When acidity drops, their number rapidly decreases. As a result, microelements and vitamins are not absorbed in the stomach, and food moves on undigested.
Another danger of this form of gastritis is the possibility of intoxication of the body with various bacteria or viruses. Hydrochloric acid, found in the stomach, is an excellent antiseptic that disinfects questionable foods. With reduced acidity, this useful function stops working.
Treatment of gastritis with low acidity involves taking medications:
- antibiotics;
- complex of vitamins and microelements (B12, iron, iodine, calcium).
A restrictive diet with a predominance of boiled and stewed dishes is indicated. Smoked meats, baked goods and sweets are completely excluded. After going into remission, homemade pickles and salted fish are added to increase acidity.
Prevention of gastritis
Prevention of gastritis in children lies entirely on the shoulders of parents. They are fully responsible for his diet. Accordingly, it is necessary to impose a normal eating schedule from a very early age, to include fiber, porridge, and fruit juices in the diet (they increase acidity and speed up digestion). This is especially important during school years.
And for the youngest children, the main thing is to breastfeed for as long as possible. Mother's milk does not create a burden on the digestive tract, since it is a concentrated mixture of only nutrients, glucose, fat, and protein. This is more than enough food for a child.
Gastritis in children, the symptoms of which and treatment directly depend on their age, quite often occurs with the introduction of complementary foods. Accordingly, it is better to prepare a diet for the child in advance. You can talk about this in more detail with your pediatrician.
And you should not ignore the therapeutic diet. These are the so-called fasting days, when the child should be given only steamed rice porridge and baked fruits and vegetables. This best cleanses the body of waste deposits, and at the same time prevents helminthiasis.
Treatment of chronic gastritis in children with drugs
Drugs indicated for the treatment of chronic gastritis in children can be divided into 2 groups:
1. Reducing the production of gastric secretions:
- antisecretory agents;
- antacids;
- proton pump inhibitors;
- anticholinergic drugs.
2. Antibacterial drugs.
- Antacids include: Rennie, Maalox, Gaviscon, Almagel, Phosphalugel. These are effective drugs that reduce the manifestation of symptoms and the risk of recurrence of the disease.
- Antisecretory drugs - Ranitidine, Famotidine. These are quite strong remedies that are used only for severe signs of gastritis.
- Proton pump inhibitors: Omeprazole, Nolpaza, Controloc, Sanpraz. Some patients may not be sensitive to this group of drugs.
- Anticholinergic agents: Gastracepin. Highly effective drugs with minimal side effects.
- Antibiotics: Amoxicillin, Metronidazole, Clarithromycin. Prescribed only if the presence of the bacterium Helicobacter Pylori is confirmed.
Symptoms of gastritis
What external signs of gastritis should puzzle parents? Naturally, the main symptom is the child’s complaint of abdominal pain. Moreover, it can be localized not only in the stomach, but also in the intestines - this is a normal phenomenon, since inflammation affects several neural centers at once and can even spread to the thoracic region.
How to understand that a baby has gastritis? The pathology may also be congenital. The following symptoms indicate this:
- he cries too often;
- does not refuse food, but often vomits, and in large portions;
- general gastrointestinal upset (smell of acetone from urine, colorless diarrhea, release of large amounts of mucus during bowel movements);
- temperature up to 38 degrees (not always);
- The child often tries to tuck his legs under him and keeps his arms on his chest or stomach.
Also, if a newborn refuses to eat and does not even take a pacifier, this should also alert parents. If you suspect gastritis, you should contact your pediatrician as soon as possible or call an ambulance (if weight loss is noticeable, even minimal).
It is worth considering that only a qualified doctor must make an accurate diagnosis of a newborn or infant. The above symptoms may indicate many other diseases, including, for example, kidney inflammation or bladder infection, hepatitis, and so on.
Symptoms of gastritis in older children are always associated with the functioning of the gastrointestinal tract. A high temperature will occur exclusively in the infectious form of gastritis, that is, when the inflammation is provoked by an infectious lesion of the mucous membrane. And this, by the way, can occur against the background of too low stomach acidity.
The diagnosis of gastritis in children itself takes a small amount of time. An experienced doctor can make an accurate diagnosis based on palpation. The main thing is to exclude intestinal adhesions and appendicitis. And you should not be afraid to seek help from a gastroenterologist. Modern methods of examining the intestinal cavity do not pose any danger. And the baby will not always have to swallow a tube for this - now you can get by using capsules with an integrated camera.
Treatment with folk remedies
Most medications have age restrictions and many side effects. If a child has gastritis at an early stage, you can resort to treatment with folk remedies. Many plants and certain foods have proven to be very effective treatments.
For gastritis the following are used:
- green apples;
- olive oil;
- honey;
- cabbage juice;
- herbal infusions (plantain, yarrow, St. John's wort, chamomile, calendula, nettle, valerian);
- birch bark;
- Japanese acacia;
- burdock;
- potato juice.
There are many recipes and diets that include folk remedies. But consultation with a gastroenterologist in this case remains a mandatory procedure.
Psychological atmosphere
One of the main reasons causing gastritis in children is stress and disturbed emotional background. Treatment will be complete only if the therapy is comprehensive: drug therapy, diet and the establishment of a psychological atmosphere.
Stress in a child can arise for hundreds of reasons: from difficult parental relationships to lack of friends in class. It is necessary to clarify these negative attitudes. This may require the help of a child psychologist, because very often parents, without realizing it, behave incorrectly towards their children and cannot independently understand the causes of the disorder.
Another main psychological cause of gastritis in children is eating disorders. This happens when a child is force-fed or forced to eat without appetite.
The desire of every parent to feed their children is natural and normal. But there is no need to lose your sanity. Only the child himself knows how much and when he needs to eat. And mom and dad should only take care that the food offered is healthy and balanced.
Having found out what caused stress in the child, it is necessary to immediately create a favorable environment at home. If the situation is critical, you should think about a psychotherapist who will prescribe sedatives.
Herbal medicine for exacerbation of gastritis in a child
Parents can speed up the child’s healing by adding proven traditional medicine recipes to the therapeutic diet and medications. Calendula, basil and hop cones have a healing effect for gastritis. To prepare a daily portion of the medicinal composition, you need a glass of water and a teaspoon of herbal raw materials. Dried basil is boiled for the shortest time - 5 minutes. Younger schoolchildren can drink warm, strained decoction 5-6 times a day, sip at a time.
Teenagers can distribute a glass of broth throughout the day on their own. The drug relieves nausea and eases pain. Hop cones are taken in the same proportion, but cooking time will take more - two to three hours. The crushed raw materials are poured with a glass of boiling water, but not boiled, but infused.
The dosage of the infusion is for younger schoolchildren, 2 tablespoons before each meal, for teenagers - a quarter glass, also before meals. Calendula is brewed with boiling water and left for 15 minutes. Junior schoolchildren can drink 1/4 glass before each meal, teenagers - 0.5 glass. Calendula perfectly cleanses the stomach from infection and relieves inflammation. Traditional healers advise giving a child suffering from acute gastritis a cup of decoction of white willow leaves in the morning on an empty stomach and immediately after that a cup of fresh milk. You should consult your doctor regarding this recipe, since not all forms of gastritis allow the consumption of dairy products and milk.
Principles of diet for gastritis in children
When treating gastritis with high acidity, adhere to the following nutritional principles: complete avoidance of smoked, fried and spicy foods. When preparing dishes, preference should be given to gentle methods: boiling, stewing.
Salt dishes in very limited quantities, and if possible, stop altogether.
Make portions small but balanced. Products that cause the production of hydrochloric acid in the stomach are prohibited. Alcoholic drinks are the same.
When treating gastritis with low acidity, there are some nutritional principles that boil down to stimulating the formation of enzymes. Most dishes are served in crushed form (puree). The amount of liquid must be increased. Sour foods are already allowed here: fermented milk, citrus fruits. But their consumption must be rationed.
Dishes should be served lukewarm, not hot. Excessively fatty and spicy foods are also prohibited. Bakery products are allowed, but in moderate portions and for 2-3 days.
Nutrition rules for gastritis
For maximum effect in treatment, it is important to adhere to the rules of a healthy diet and feed your child healthy foods:
- Rationality, regularity, fractionation of food intake. With gastritis, you need to eat in small portions, but often, so that the secreted gastric juice has something to digest. Feeding should be done 4-5 times a day or more, at clearly established times.
- Use only fresh food, it is better to prepare dishes immediately before consumption. You need to give up smoked, fatty, fried, spicy foods. Exclude from the menu baked goods made from white flour, black bread, which increases the acidity of the gastrointestinal tract, cakes, sweets, legumes, and raw vegetables.
- Dishes should be served boiled, baked, or steamed. You should not eat rough, hard food. Food should be soft, brought to a mushy state, slightly above room temperature.
- The menu should include mashed potatoes, light vegetable soups, broths, and decoctions made from dietary turkey, rabbit, and chicken meat. It is important to regularly eat porridge: rice, buckwheat, corn, oatmeal. You can include steamed cutlets from dietary meat, cottage cheese casseroles, crackers, and day-old white bread into your diet. For drinks, it is better to take weak teas, drinks made from dried fruits, and medicinal herbs.
It is especially important to strictly adhere to dietary nutrition during the period of exacerbation of the disease, although with chronic gastritis you need to regularly monitor the child’s diet.
Permitted and prohibited products
The full list of acceptable and prohibited products is presented in the table:
| Product categories | Authorized products | Prohibited Products |
| Meat | Lean varieties of beef, horse meat, venison, elk, rabbit | Pork, lamb |
| Bird | Turkey, chicken, quail | Goose, duck |
| Fish | Low-fat fish species: bream, cod, carp, pike perch, pollock, navaga, hake, blue whiting, mullet, pike, flounder, pollock, carp, chum salmon | Salmon, tuna, mackerel, trout, salmon, sturgeon, halibut, Atlantic herring, nanothenia, whitefish, Caspian sprat, eel, sabrefish, catfish, burbot, ivasi, beluga, saury, stellate sturgeon, nelma, chinook salmon, omul, silver carp |
| Bakery products | Yesterday's wheat bread, bran cakes, lean crackers, classic drying | Fresh bread, buns, donuts, cakes, sweet bagels, shortbread |
| Cereals | Oats, buckwheat, rice, semolina | Millet, corn, barley, pearl barley |
| Vegetables | Cauliflower, zucchini, potatoes, carrots, pumpkin, peeled cucumbers, dill (in small quantities) | Fresh or sauerkraut, onions, garlic, sorrel, spinach. |
| Fruits and berries | Bananas, melons, cherries, raspberries, pears, apples, watermelons | Citrus fruits, grapes, gooseberries, blueberries |
| Dairy | Low-fat cottage cheese in the form of casseroles, low-fat yoghurts | Whole cow's or goat's milk, kefir (for high acidity) |
| Beverages | Herbal infusions, teas, unsweetened compotes, fruit drinks, jelly | Alcoholic drinks, kvass, highly carbonated drinks, concentrated juices, Coca-Cola |
Menu for a week for gastritis in a child with recipes
Gastritis in a child (symptoms and treatment must be strictly monitored by a gastroenterologist) obliges him to adhere to a certain diet. Below is a sample menu for 7 days for a child.
Monday
Breakfast:
- oatmeal on water with raisins and pear;
- Herb tea.
Dinner:
- noodle soup with chicken meatballs;
- boiled rice with baked veal;
- wheat bread;
- dried fruits compote.
Afternoon snack: raspberry and apple jelly.
Dinner:
- steamed hake with vegetable casserole;
- bread;
- tea.
Tuesday
Breakfast:
- omelette with milk and cheese;
- Herb tea.
Dinner:
- oatmeal soup with low-fat beef broth;
- boiled buckwheat with turkey goulash;
- bread;
- frozen berry compote.
Afternoon snack: cottage cheese casserole with sour cream and raspberries.
Dinner:
- turkey heart risotto;
- bread;
- tea.
Wednesday
Breakfast:
- milk rice porridge;
- homemade rice flour cookies;
- berry tea.
Dinner:
- pike perch fish soup with wheat croutons;
- potato casserole with veal chop;
- pear;
- berry jelly.
Afternoon snack: raspberry pudding.
Dinner:
- pilaf with veal;
- bread;
- cucumber and herb salad with olive oil;
- tea.
Thursday
Breakfast:
- poached egg;
- cheese with bread;
- berry tea.
Dinner:
- buckwheat soup with quail broth;
- vegetable stew of zucchini with veal meatballs;
- bread;
- dried apple compote.
Afternoon snack: baked pear with nuts and honey.
Dinner:
- pumpkin porridge with turkey cutlet;
- apple;
- bread;
- Herb tea.
Friday
Breakfast:
- semolina;
- Herb tea.
Dinner:
- potato soup with rabbit meat;
- boiled vermicelli with baked pollock;
- tomato and herb salad with flaxseed oil;
- berry compote.
Afternoon snack:
- banana;
- kefir.
Dinner:
- zucchini soup with chicken;
- bread;
- herbal decoction
Saturday
Breakfast:
- buckwheat casserole with cottage cheese;
- tea.
Dinner:
- cauliflower cabbage soup with turkey;
- country-style potatoes with beef goulash;
- bread;
- berry juice.
Afternoon snack: a cocktail of kefir and cottage cheese with the addition of cherries.
Dinner:
- carrot and zucchini casserole with chicken cutlet;
- bread;
- tea.
Sunday
Breakfast:
- oatmeal in water with nuts and melon;
- tea.
Dinner:
- rice soup with chicken broth;
- hake baked with zucchini and cauliflower;
- bread;
- cherry compote.
Afternoon snack: cottage cheese casserole.
Dinner:
- pike meatballs with buckwheat porridge on water;
- bread;
- low-fat natural yogurt;
- tea.
Gastritis does not at all oblige you to eat sparingly and limitedly; many permitted dishes are tasty and nutritious.
The most interesting recipes for breakfast, lunch, afternoon snack and dinner are given below:
Cheese omelet recipe (breakfast)
Required ingredients:
- 3 eggs;
- Russian cheese - 40 g;
- a pinch of salt (can be omitted);
- milk - 150 ml;
- vegetable oil.
Cooking method:
- Crack the eggs into a bowl and beat with a blender on low speed or with a fork.
- Pour milk into the eggs, continuing to stir until a homogeneous consistency is obtained.
- Grease a deep frying pan with vegetable oil and heat.
- Pour the mixture of eggs and milk into a hot frying pan, cover with a lid and cook for 5-10 minutes.
- Before serving, add salt to taste and sprinkle with grated cheese.
Fish soup from pike perch with wheat croutons (lunch)
Required ingredients:
- boneless pike perch fillet - 400 g;
- potatoes - 2 medium pieces;
- carrots - 1 medium piece;
- salt to taste;
- dill to taste;
- wheat bread.
Cooking method:
- Boil 3 liters of water in a saucepan.
- Place the washed fish fillet into the boiling broth. Add salt to taste.
- After 25 minutes, remove the fish fillet.
- Add grated carrots and diced potatoes into the broth.
- Cut the wheat bread into cubes and dry in the oven in a dry frying pan for 10 minutes at a temperature of 1500C.
- Pour the soup into bowls, add fish fillet and sprinkle with crackers.
Recipe for baked pear with nuts and honey (afternoon snack)
Required ingredients:
- large pears;
- butter - 20 g for each fruit;
- a handful of walnuts;
- honey to taste.
Cooking method:
- Wash the pears, cut them in half and remove the core.
- Place a piece of butter in the middle.
- Bake in the oven for 7 minutes at 1600C.
- Before serving, sprinkle with nuts and honey to taste.
Recipe for zucchini soup with chicken (dinner)
Required ingredients:
- zucchini - 2 pcs.;
- carrots - 2 pcs.;
- low-fat cream - 200 ml;
- potatoes - 1 pc.;
- salt to taste;
- chicken fillet - 300 g.
Cooking method:
- Wash and boil vegetables.
- Leaving a little water in the pan, blend the vegetables with a blender until smooth.
- Pour in the heated cream and salt, mix everything.
- Wash and boil chicken fillet.
- Serve the soup with chopped chicken.
Gastritis in children is a common disease in the modern world. If you notice the first symptoms, you must immediately contact a gastroenterologist for a diagnosis and treatment. A timely cured disease and a subsequent healthy lifestyle will prevent this problem from returning.
Article design: Mila Friedan
Diet for a child with chronic gastritis
The diet for chronic gastritis in children is based on the principles of mechanical, chemical and thermal sparing of the stomach.
Rough, spicy and fatty foods, smoked meats, baked goods, chocolate, chips, soda and other “unhealthy” foods should be excluded from the child’s diet.
The amount of fresh vegetables is sharply limited .
They are replaced with boiled or stewed ones. All food should be steamed, boiled or stewed. Do not serve food that is too hot or too cold. Boiled meat and fish, dairy dishes, omelettes, soft-boiled eggs, well-cooked cereals, dried white bread, weak tea or rosehip infusion are recommended
In children, chronic gastritis usually occurs against a background of normal acidity or with its increase. Therefore, most often young patients are prescribed dietary table No. 1, a weekly menu plan for which may look something like this.
On our website: Symptoms of chronic atrophic gastritis and its treatment
Monday
08:30. Milk rice porridge, soft-boiled egg, tea with milk. 11:00. Applesauce with sugar. 13:30. Vegetable puree soup, potato and zucchini puree, boiled meat, fruit jelly. 16:00. Rosehip decoction, dry cookies. 18:30. Baked fish with milk sauce, carrot puree, tea with milk and honey. 21:00. Non-acidic kefir.
Tuesday
08:30. Milk oatmeal, cottage cheese casserole with sour cream, tea with milk. 11:00. Stewed apple or pear. 13:30. Puree vegetable soup, steamed meatballs, mashed potatoes with butter, dried fruit compote. 16:00. Rosehip decoction, cracker. 18:30. Fish balls, boiled buckwheat porridge, jelly. 21:00. Warm milk.
Wednesday
08:30. Semolina porridge with milk, steam omelette, coffee drink with milk. 11:00. Fruit jelly. 13:30. Milk soup, steamed meat cutlets, carrot puree, fruit jelly. 16:00. Rosehip decoction, dry cookies. 18:30. Boiled fish, pureed buckwheat with butter, dried fruit compote. 21:00. Non-acidic kefir.
Thursday
08:30. Milk rice porridge, non-sour cottage cheese, tea with milk. 11:00. Baked apple. 13:30. Milk soup, boiled white chicken, mashed potatoes and zucchini, fruit jelly. 16:00. Rosehip decoction, cracker. 18:30. Poached fish, pumpkin puree, tea with milk and honey. 21:00. Warm milk.
Friday
08:30. Milk buckwheat porridge, soft-boiled egg, tea with milk. 11:00. Fruit mousse. 13:30. Vegetable soup, steamed chicken cutlets, carrot puree, apple mousse. 16:00. Rosehip decoction, dry cookies. 18:30. Boiled rice, steamed meat, fruit jelly. 21:00. Non-acidic kefir.
Saturday
08:30. Oatmeal with milk, cottage cheese casserole with sour cream, coffee drink with milk. 11:00. Baked apple. 13:30. Pumpkin puree soup, boiled meat, mashed potatoes with butter, dried fruit compote. 16:00. Rosehip decoction, cracker. 18:30. Fish fillet balls, boiled buckwheat, jelly. 21:00. Warm milk.
Sunday
08:30. Semolina porridge with milk, steam omelette, tea with milk. 11:00. Baked pie with jam, jelly. 13:30. Fish soup with vegetables, steamed cutlets, rice pudding, apple mousse. 16:00. Rosehip decoction, dry cookies. 18:30. Chicken souffle, mashed potatoes and zucchini, tea with milk. 21:00. Non-acidic kefir.
On our website: Exercising with gastritis - is it possible?