Related and recommended questions
The skin of the outer corner of the eye is red. A 5-year-old child has red skin (outer...
Everything around the eyes is swollen and itchy. Everything around the eyes is swollen and red, at first everything...
Scaly redness under the eye Two weeks ago I noticed a roughness under the eye,…
Redness and suppuration of the eye. My daughter is 3 years old, yesterday before going to bed something got in her...
A child's eye is swollen Child 2.7. Today we walked a little in the wind (in the morning) to…
Problem with eyes (redness) I have such a problem, one day I got itchy...
A child's eye is swollen. A 1-year-old child has an inflamed eye, the membrane is red and cloudy and...
Redness of the inner corner of the eye Two months ago I had, I don’t know, the flu...
Diseases of the eyelids Problems with my eyelids began in December 2021. A month before this I...
A child’s eyes are swollen in Thailand. On vacation in Thailand, the child’s eyes first turned red...
The eye and the corners of the eye turned red Two days ago, the inner corner of the left eye turned red...
Redness and swelling of the eyes I have been doing eyelash extensions with rare breaks continuously for…
Redness in the corner of the eye Redness began from the corner of the eye, then tugging, burning,...
Swelling in the inner corner of the eye Two days ago, the upper eyelid began to hurt…
Severely swollen eye with redness The baby's eye suddenly swollen after a night's sleep in the morning...
Redness of the outer corner of the eye in an elderly person. Please tell me. To grandma...
Red skin on the outer corner of the eyelid My son (4 years old) has redness on the outer corner...
Redness in the corners of the eyes. Child 5 years old. Some redness appeared in the corners of the eyes...
Hit in the eye, redness of the white of the eye. Please help. I was hit hard in...
The eye is red and festering. The child is allergic; he went to kindergarten for 5 days; on Thursday he got up...
Symptoms
In a child, red eyes are accompanied by various symptoms: burning, stinging, dryness, lacrimation. Often, along with redness, bruises appear under the child’s eyes (especially with allergies or poor sleep).
First of all, it is important to find out the reason why the whites of the eyes turn red.
Forms of redness:
- superficial inflammation - the protein turns red on the outside of the iris; The conjunctiva is often affected, the eye hurts;
- deep inflammation - inflammation that occurs inside the eyeball; the vessels are more affected around the iris, the redness is less pronounced towards the periphery.
Related and recommended questions
The corner of the eye is irritated. Let’s decide on a diagnosis.. It’s been a constant for a couple of months now...
Redness in the corner of the eye Redness began from the corner of the eye, then tugging, burning,...
Redness of the outer corner of the eye in an elderly person. Please tell me. To grandma...
Red skin on the outer corner of the eyelid My son (4 years old) has redness on the outer corner...
Redness of the skin around the eyes My daughter is five and a half years old. I started rubbing my eyes...
The inner corner of the eye is itchy and swollen. Please tell me what to do. I have…
Red formation in the corner of the eye For about 1.5 years I have been noticing on my inner...
Redness and peeling of the skin around the eyes I have something going on with the skin around my eyes...
The skin around the eyes is peeling, red, swollen and burning. Please help me go...
Peeling at the corners of my eyes The corners of my eyes are peeling, I went to the doctor and he said to apply it...
Redness in the corners of the eyes. Child 5 years old. Some redness appeared in the corners of the eyes...
Itching in the corner of the eye I began to experience itching in the inner location of the eye, t...
The corner of the eye itches. The inner corners of the eyes itch. Almost at the eyelashes.
Problem with eyes (redness) I have such a problem, one day I got itchy...
Inflammation in the corner of the eye My son (15 years old) has persistent scaly redness in the corner of the eye...
Crack in the corner of the eye Dear specialists! Recently, in the inner corner of the eye...
My 5 month old baby has a red eye My 5 month old baby has a red eye...
Staphylococcus epidermis in the eye of a child This summer, my 9-year-old son turned red...
Pain in the outer corner of the eye I have pain in the outer corner of the eye, mainly when blinking….
The child’s eyes turned red, transparent pimples Two days ago the child’s eyes turned red...
Why does this happen: reasons for the appearance of red spots, dots, blood vessels
If the child's eye turns red and a capillary mesh appears, try to find the reason for this. If the provoking factor can be eliminated, the redness itself will go away.
If the cause is an internal disease, visiting a doctor and treatment cannot be avoided.
Causes causing redness:
- fatigue, overstrain;
- entry of a foreign body;
- eye injury;
- allergy;
- blockage of the tear duct in infants.
If you are unable to determine the cause of the redness on your own, consult a doctor immediately.
If a red spot appears on a child’s eye, most likely the reason for this is one of the following conditions:
Change in blood pressure. If the pressure is high or low, there is a chance that small vessels in the child's eye will burst, causing a hematoma (which causes red whites)
This defect does not need to be treated. It is only important to eliminate the cause of its appearance. Carry out systematic monitoring of the baby’s blood pressure, consult a doctor.
Heavy loads. If a child lifts weights, the pressure in his capillaries temporarily increases and hemorrhages occur (a red spot or dot inside the white of the eye)
In this case, there is no need to panic, the hemorrhages will go away on their own.
A sharp increase in eye pressure. Only a doctor can measure blood pressure. It is worth consulting with him if spots or red blood vessels appear too often and do not disappear for a long time.
In addition to these reasons for the formation of hemorrhages, there is another one - red vessels on the sclera in a newborn can be a congenital defect
. Red spots do not impair the baby's vision and are completely harmless.
Red capillaries in the eyes of a baby spoil the appearance of the child; consult a doctor to determine the possibility of removing them.
The causes of redness can be diseases:
- Diabetes and other disruptions in hormonal balance, due to which the walls of the capillaries become thinner.
- Infections with fever.
- , keratitis, accompanied by hemorrhages, increased lacrimation and discomfort.
- Tumors. Neoplasms grow and put pressure on the organelles of the eye, stretching the blood vessels, which leads to their damage.
- Deficiency of vitamins A and C in the body, which are responsible for the flexibility of the walls of blood vessels.
- Meteosensitivity.
Some more useful information about why children may have red eyes:
Causes of red eyes in children
- A number of diseases of the organs of vision - uveitis, blepharitis, conjunctivitis, cyclitis, scleritis and others - are characterized by one common symptom - redness of the whites of the eyes. The nature of these diseases is different - bacterial, fungal, viral, caused by protozoa or has a combined nature - as well as the approaches to their treatment. Therefore, it is important that the child sees a doctor for a diagnosis and treatment plan. The doctor may prescribe ophthalmic antibiotics, antiviral, antifungal, antiprotozoal agents, which are dangerous to select on your own. In young children, the eyes may turn red with developing dacryocystitis - blockage of the nasolacrimal duct with its further inflammation. This condition requires observation by a doctor and the use of a whole range of medications, as well as being accompanied by special massage and hygiene measures.
- Redness of the eyes often accompanies an increase in body temperature. Moreover, redness of the whites of the eyes is caused not by the temperature itself, but by the pathogens of the disease that caused it. Thus, eyes often turn red during ARVI, influenza, tonsillitis and other infectious diseases. In addition to red eyes, the child experiences hyperthermia, nasal congestion, hoarseness, sore throat and/or nasopharynx, weakness, joint and muscle pain, drowsiness, and lethargy. Redness of the eyes will go away along with the symptoms of the disease with proper and timely treatment. In this case, you do not need to contact an ophthalmologist. Recommendations for treating the disease will be given by a pediatrician or otolaryngologist.
- If pain and pain in the eyes, mucous or purulent discharge from the lacrimal canal, and visual disturbances are added to the indicated clinical picture, then a visit to an ophthalmologist is necessary, since it is obvious that the infection, in addition to the respiratory tract, has also affected the eyes. For example, an infectious disease such as measles, for example, causes conjunctivitis and requires treatment not only from an infectious disease specialist, but also from an ophthalmologist.
- Children's eyes turn red after swimming in open water and swimming pools. Microorganisms living in reservoirs and disinfectants used to purify water adversely affect the mucous membranes of the eyes, causing redness of the whites, dryness, and pain. You can get rid of these symptoms by rinsing your eyes with clean warm water, miramistin or saline and instilling drops with a softening, lubricating and vasoconstrictor effect (any drops from the “artificial tear” series will do). If, after swimming in a river, sea or pool, in addition to redness, the child experiences pain or pain in the eyes, or mucus or pus is released from the lacrimal canal, then the parents should visit a doctor with the child. If the condition persists even after treatment and resuming bathing, doctors usually recommend using a special goggle mask to protect the eyes from splashes.
- Eyes also turn red from smoke. If a family went on a picnic, barbecued, or made a fire for other needs, and the child hung around nearby, then the redness in the eyes is probably a kind of reaction to the components of the smoke. It greatly irritates the mucous membranes, causing a feeling of dryness, burning, itching. The same scheme will help to soothe the eyes and relieve a complex of unpleasant symptoms as if water from the sea or pool gets into the eyes - rinsing and instilling drops from the “artificial tear” group. If something gets into the eye when the child was near an open fire, it is necessary to rinse the eye and see a doctor. Ashes, ash and other combustion products can significantly harm a child.
- Another reason for red eyes is a child being outside during strong gusts of cold wind. In such cases they say “blown”. If there are no other symptoms of eye diseases, then you just need to give the child the opportunity to rest and sleep. Then the redness will go away on its own. Severe redness sometimes goes away only after a few days. Vasoconstrictor drops will help speed up the process.
- Children who experience excessive visual stress often have red eyes. Redness is accompanied by a feeling of heaviness in the eyelids (it is difficult to open the eyes), increased sensitivity to light, and painful sensations. The child urgently needs rest, proper sleep and reduced visual stress. It is important not only to limit watching TV and playing on a computer or tablet, but also reading, drawing, sewing, in a word, all types of activities where you need to look intently in one direction. Otherwise, the child will begin to quickly lose vision. Children must follow a daily routine, rules of personal hygiene, take complex vitamin preparations to maintain their eyes, and do special relaxing exercises.
- Young children do not always know how to properly follow the rules of personal hygiene. They may wash themselves in such a way that they get soap in their eyes. You can solve the problem by simply rinsing your baby's eyes with plenty of clean water. The same should be done if shampoo or shower gel gets into your eyes. If the parent does not know what kind of substance has gotten into the child’s eyes, or he knows that it is a caustic agent (for cleaning plumbing fixtures, detergent for ceramics, bleach or stain remover for laundry), vinegar, brine, marinade, and so on, then the child needs Immediately show a doctor or call an ambulance. Prolonged exposure of the eye to acidic or alkaline environments can cost children both their vision and the eye itself. First aid is to wash the eyes. Do not bury anything to avoid an aggressive chemical reaction.
- A common cause of red eyes is allergies. Typically, children's eyes turn red during the flowering period of various plants, that is, with an allergy to pollen. But in the same way, allergies to house dust, medications, food, fur and animal excretions manifest themselves. Antihistamine eye drops help with this condition. They are prescribed by an allergist or ophthalmologist (you need to go to him if the allergic diagnosis is known). Allergic redness of the eyes is often accompanied by watery eyes, itching and photophobia. But allergies do not affect the quality of rhenium if you take medications on time and avoid contact with allergens.
- If one eye of a child is red, then the nature of the redness is most likely traumatic. Sand or other foreign matter may have gotten into the eye. It is better not to try to remove it yourself, but to go to an eye emergency room. Some foreign bodies cannot be noticed and removed without special equipment. And massaging the eyelid, pulling back the eyelashes, and frequent blinking often not only do not alleviate the condition, but also aggravate the situation by the fact that the foreign body moves along the cornea and causes minute mechanical damage to it. Such damage scars and will reduce the quality of vision over time.
- A red spot on a child's eye may indicate that a blood vessel has burst in the eye. This happens in several cases: with an eye injury (impact, foreign object), with excessive physical activity (for example, after intense sports training), prolonged loud crying (in infants). A visit to the doctor in this case is advisable, but if the eye tissue is not damaged, the red spot will go away on its own. If a child’s blood vessels often burst, the ophthalmologist will prescribe special drops that help strengthen the vascular walls.
Prevention measures
Prevention of eye diseases begins with parents observing basic hygiene rules. Children under one year old and those who are older may often rub their eyes with their hands.
When a child is an infant, adults monitor hygienic conditions on their own, but a grown-up baby needs to be explained the importance of clean hands and taught to keep them clean. In addition, you need to control the effect of natural irritants on the body, such as:
- sun while relaxing at sea;
- cold wind;
- dirty water;
- influence of third-party objects.
When the first signs of an inflamed eye appear, you should immediately consult a doctor; you should not self-medicate. With home therapy, you can delay time and aggravate the situation, which will negatively affect the development of the disease and timely diagnosis. Since even the most attentive parents will not be able to independently determine the culprit of the disorder, and self-medication can threaten vision loss.
Related and recommended questions
A 2-year-old child has swelling and redness in the corner of the eye 5 days ago, the child has…
The skin of the outer corner of the eye is red. A 5-year-old child has red skin (outer...
Problem with eyes (redness) I have such a problem, one day I got itchy...
A lump in the corner of a child’s eye Anastasia Mikhailovna! my daughter is 6 and a half months old...
The corner of the eye is irritated. Let’s decide on a diagnosis.. It’s been a constant for a couple of months now...
Redness in the corner of the eye Redness began from the corner of the eye, then tugging, burning,...
Redness in the corners of the eyes. Child 5 years old. Some redness appeared in the corners of the eyes...
The child's eye is swollen, red and festering. The child is 1.8. The right eye is swollen, sometimes watery,...
The child's eyelid is red. The child is 11 months old. The eyelid under the eye is red...
The child’s eyes turned red, transparent pimples Two days ago the child’s eyes turned red...
Pus in the eyes after sleep I have a 3 year old child in the garden today I saw that the eyes after...
Redness and suppuration of the eye. My daughter is 3 years old, yesterday before going to bed something got in her...
A child's eye turned red after a blow. A child running on the street fell and hit his eye on...
Redness of the outer corner of the eye Dear Doctor. My seven year old daughter blushed...
Redness and dry crusts in the inner corners of the eyes. My son is 9 years old and has been...
Swelling in the inner corner of the eye Two days ago, the upper eyelid began to hurt…
The child poked his finger into his eye. The child poked his finger into his eye. Immediately there was a feeling...
Red skin on the outer corner of the eyelid My son (4 years old) has redness on the outer corner...
Redness in the inner corner of the eye The inner corner of my right eye is red...
Redness of the outer corner of the eye in an elderly person. Please tell me. To grandma...
What should parents do?
If one eye of a baby turns red due to temporary external factors, parents take the following measures at home:
- sleep in a calm environment;
- elimination of bright lighting, dust, drafts;
- exclusion of watching TV and computer equipment;
- care for the eyes, hands and nails of a newborn;
- exclusion of communication with other children.
Red white of the eye occurs when a foreign object enters the eye. The item should be removed as follows:
- Examine the reddened eye by gently pulling back the eyelids.
- Use a cotton swab to remove dirt.
- Rinse with boiled water, chamomile infusion or weak brewed black tea at room temperature. The liquid is drawn into a pipette or syringe without a needle.
- The baby is placed on the side other than the injured eye. The other eye is covered with a cotton pad. Rinsing is carried out from the outer to the inner edge of the eye.
If a child is diagnosed with a disease, drug therapy is carried out with eye drops, ointments, tablets and rinses. The form of admission and duration of the course are determined by the doctor based on the examination. The main treatment methods are described in the table:
| Disease | Procedures | Drugs |
| Dacryocystitis | Do eye rinsing with furatsilin | Antibiotics |
| Probing (performed by a doctor) | ||
| Massage of tear ducts and eye area | ||
| Allergy | Rinsing with chamomile solution, weak brewing of black tea | Antihistamines |
| Immunotherapy | Glucocorticosteroids | |
| ARVI | Rinsing with a solution of furatsilin or chamomile | Antiviral |
| Inhalations | Vitamins | |
| Uevit | Plasmapheresis | Immunosuppressants |
| Glucocorticosteroids | ||
| Hemosorption | Anti-inflammatory | |
| Anesthetics | ||
| Autohematotherapy | Antibiotics | |
| Antiviral | ||
| Antimicrobial | ||
| Blepharitis | Washing with tar soap, tansy decoction | Glucocorticosteroids |
| Antibiotics | ||
| Antiseptics | ||
| Antimicrobial | ||
| Conjunctivitis | Washing with furatsilin, potassium permanganate | Antibiotics |
| Antiseptics | ||
| Antimicrobial | ||
| Disinfectants | ||
| Antiviral | ||
| Vegetative-vascular dystonia | Massage | B vitamins |
| Physiotherapy | Sedatives | |
| Swimming | Nootropics |
When glaucoma develops in a newborn in the initial stages, drug therapy with drugs is possible. To normalize the outflow of fluid, lower intraocular pressure and prevent complications, surgical intervention in infancy is recommended.
Treatment at home
At home, complete treatment of such a symptom is impossible, although in case of severe redness, symptomatic therapy with the use of ophthalmic ointments and drops is appropriate.
Regardless of the disease, in such cases, rinsing with chamomile decoction or furatsilin is indicated , and when dacryocystitis is diagnosed, the child must be given a simple massage of the lacrimal ducts.
If the cause of redness is blepharitis, long-term complex treatment will be required , which should include:
- regular washing of the edges of the eyelids using disinfectants,
- using Tobrex or Vidisik ointments,
- the use of antiseptics amitrazine and miramideza.
For uveitis, complex treatment is also carried out, including a course of glucocorticosteroids and immunosuppressive drugs (including prednisolone).
You can partially eliminate discomfort and reduce swelling with the help of compresses and lotions , which can be easily prepared at home.
For the treatment of children, it is best to use chamomile decoction, the use of which has a minimum number of contraindications.
Pour two teaspoons of the herb into a glass of boiling water and let it brew for 20-30 minutes.
Note! The eyes are washed with this decoction two to three times a day, and this helps suppress the activity of pathogenic microorganisms and has a calming effect on irritated skin.
For older children, you can use a mint-based decoction.
Two tablespoons of dried herb are poured into 0.5 liters of boiling water and the mixture must be further simmered over low heat for 15 minutes.
A clean cloth or gauze is moistened in the liquid that has cooled to room temperature - such compresses are applied to the eyes before going to bed once a day.
Dacryocystitis
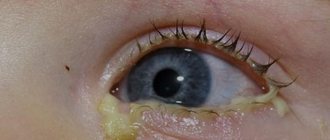
In the structure of ophthalmological diseases of children, one of the most common inflammatory diseases in newborns is dacryocystitis. Develops as a result of obstruction of the nasolacrimal duct. The baby's eye becomes reddish. Purulent contents are released from the nasolacrimal sac.
From 2 months, probing can be performed, which is currently the most common treatment method. Until the age of 2 months. You can perform a massage in the area of the nasolacrimal duct on the bridge of the nose. In 50% of cases, massage avoids the need for probing.
If your child's eyes are red, you should immediately consult a doctor. Almost all ophthalmological diseases are manifested by edema, hyperemia, and discharge, but the treatment is different in each case. To prescribe the correct treatment, consultation with a pediatrician or ophthalmologist is necessary, since eye symptoms occur in a number of somatic diseases. A timely diagnosis will avoid unnecessary costs for unnecessary medications and save the child’s vision.
Natural reasons why infants have red eyes can be due to various factors. Viruses and bacterial infections are no exception, as well as other diseases associated with difficult labor (i.e., consequences of birth injuries). Red eyes in newborns are also a sign of burst blood vessels in the sclera.
The appearance of red spots in the corners of the eyes or around them is a reason to immediately call a doctor. First of all, he will explain to you what is the provoking factor, and if necessary, prescribe medication (sometimes they can do without medications). The main causes of red eyes in infants are:
- entry of a foreign body;
- conjunctivitis (in this case the eye begins to fester and stick together);
- eye fatigue;
- manifestation of a cold (“blown by the wind”);
- the impact of viruses, bacteria, chlamydia, as well as the impact of other infections on the eyes;
- blockage of the tear duct;
- birth injuries (if red spots are visible around the lens);
- blepharitis (inflammation of the eyelids in the eyelash area);
- uveitis (inflammation of the choroid of the eye);
- glaucoma in infants (increased intraocular pressure). We recommend about the details of this disease;
an allergic reaction in an infant to seasonal pollen, dust, and pet hair.
After determining the negative factor, the specialist will tell you how to properly care for the inflamed eye shell.
Typical symptoms
If the redness does not go away within a few days, a dangerous pathology may develop.
Red eyes are a common sign of various pathologies that have different external manifestations. Sometimes the eye turns red due to a burst capillary; there are cases when there is complete redness of the membrane, which even affects the pupils. This problem often occurs in babies, and since a child of several months cannot explain his feelings, it is important to differentiate ophthalmological pathology from fatigue.
Additional signs
By paying attention to what symptoms accompany reddened eyes, you can determine the main factor that provoked the problem:
- Redness and swollen eyes sometimes indicate kidney disease. Fluid imbalance leads to fluid accumulation in soft tissues, including the periocular area.
- A red eye without pus “speaks” of an outbreak of an infectious disease. At elevated temperatures, a cough, runny nose, and headache appear.
- The visual organs become red and itchy in response to the allergen. In addition, children may notice excessive tearing and swelling. The addition of high fever and muscle pain, coupled with redness and itching, may also indicate an allergy.
- A red eyeball and the presence of purulent discharge during conjunctivitis can cause a slight fever.
- Red eye in a baby can be the result of microtrauma, vascular tension that occurred during childbirth. The situation is not dangerous; the symptoms will go away on their own over a period of several weeks to one month.
- When you have a cold, against the background of a weakened immune system, the mucous membrane of the eyes turns red and green snot appears.
- With blepharitis, the eyelash margin is affected, the eyelids or their edges turn completely red. Sometimes redness covers the entire white of the eye without affecting the pupil.
Why might the whites of the eyes turn red?
If the whites of the eyes turn red, it means that the blood capillaries have been damaged. These thin vessels penetrate the entire protein membrane, providing nutrition to the organ of vision.
The degree of vascular damage can vary - a few red dots or completely reddened sclera.
The causes of redness in adults are much greater than in children.
- The protein becomes distinctly red after an impact, when a large number of capillaries are damaged. Additional symptoms include severe pain, lacrimation, and blurred vision. A hematoma forms on the skin.
- If the eye hurts, the whites are red and there is increased lacrimation, the cause may be a foreign body. Especially often small specks, slivers, and metal shavings get into the eye.
- Squirrels turn red due to allergies. The person is bothered by itching, burning, and tears constantly flow. Extraocular manifestations include headache, sneezing, and cough.
- Chronic alcoholics develop small hemorrhages in the sclera. Because of this, the whites are red and the eyelids are swollen.
- Red whites of the eyes in newborns are associated with infection during childbirth - chlamydia, gonococcus. There is abundant purulent discharge, sticking together the eyelids, and pronounced swelling.
- Constant redness is observed in patients with gout. With this disease, salt crystals are deposited in various organs. Damage to the organ of vision leads to the development of uveitis, keratitis, and iridocyclitis.
- An attack of glaucoma causes massive damage to the capillaries. The white becomes uniformly red. The person feels severe pain, vision decreases sharply.
- Red streaks in the whites of the eyes appear in some infectious diseases - leptospirosis, tularemia. The patient's temperature rises and pain in muscles and bones occurs.
- Red sclera is observed in a disease such as keratitis. This is an inflammation of the cornea of the organ of vision. Most often caused by infections. Manifested by blurred vision and lacrimation.
- Red sclera is associated with very high blood pressure. There is an expansion of all brain vessels, including the eye capillaries.
- Redness combined with increased fatigue and blurred vision is a sign of vitamin deficiency. Vitamin A and lutein are the most beneficial for the organ of vision.
Incorrectly chosen contact lenses and glasses cause redness of the sclera. Red whites in a person are noticeable after sleep, if it was insufficient in time. The organ of vision does not have time to recover after prolonged fatigue.
Such manifestations disappear on their own with proper rest.
Should you see a doctor: causes of red corners of the eyes in a child
Children's eyes require special care. Often children are not aware of their actions during games, and can injure their vision.
Redness in the corners of the eyes causes concern among parents.
It is worth knowing that the corners most often turn red due to mechanical stress and rubbing , and additional symptoms such as pain and peeling of the skin may appear.
ontakte
Odnoklassniki
- ARVI;
- conjunctivitis;
- blepharitis;
- uveitis;
- allergy;
- injury;
- foreign body;
- dacryocystitis;
- vegetative-vascular dystonia.
In children with colds (ARVI, acute respiratory infections), as well as with sore throat, flu and measles, the visual organs turn red due to viral conjunctivitis. This phenomenon is explained by the fact that with any similar diseases inflammation of the mucous membranes occurs.
Along with red corners, a cold may be accompanied by redness of the visual organ itself, swelling of the eyelids, burning and itching. The reason for this is sinusitis , or inflammation of the paranasal or paranasal sinuses .
When they become inflamed, the nasal septum swells, which prevents the sinuses from naturally clearing phlegm and mucus. This process provokes pressure on the tear duct and leads to severe redness in the corners of the eyes.
The conclusion suggests itself:
first of all, it is important to cure a cold , and then begin treatment for viral conjunctivitis.
Photo 1. A cold and runny nose in a girl causes redness and swelling not only in the corners, but also in the entire eye.
Conjunctivitis
A child, especially at an early age, often cannot tell his mother that his eyes are bothering him. The following symptoms will indicate the disease:
- The eyes become intensely red , including the eyelids and the eyeball itself (not from crying).
- The child is irritated by bright light. He squints, cries, turns away when the curtains are opened or artificial lighting is turned on.
- Pus is released abundantly , and the baby often cannot open his eyes on his own after sleep.
Important! Other family members can become infected with conjunctivitis. It is necessary to be careful and monitor the child’s hygiene, as well as thoroughly wash his toys and change the pillowcase daily.
Considering that inflammation of the conjunctiva is accompanied by itching, the baby will rub his eyes with his hands. That is why maintaining cleanliness is a component of successful therapy.
Blepharitis
The disease is diagnosed based on visual examination of the eyelashes and eyelids using a slit lamp.
Sometimes a laboratory examination is prescribed for the cellular or microbial composition of a scraping taken from the conjunctiva, and the presence of microscopic demodex mites in the eyelash bulbs is determined.
Uveitis
Manifestations of uveitis can be different, depending on the location of the inflammatory focus, the body's resistance and the aggressiveness of the infection. With the combination of several factors at once , the manifestations of anterior uveitis can increase in a certain sequence:
- slight “fog” before the eyes;
- feeling of heaviness;
- significant visual impairment;
- redness of the eyes;
- aching pain;
- narrow pupil that does not respond to light;
- photophobia and redness of the corners of the eyes;
- acute eye pain and increased intraocular pressure;
- complete blindness.
Reference! With posterior uveitis, the symptoms of the disease appear late and are mild - there is no pain or redness of the eye. Vision decreases gradually. In this case, a “spot” appears in front of the eye (scotomy), “fog” or “veil”.
Allergies in babies
Allergies, hay fever, seasonal or allergic rhinitis.
This phenomenon has many names, but the essence is the same - increased sensitivity of the body to certain substances that provoke negative physiological reactions, including redness of the corners.
Whatever factor causes the allergy, it is important to remember a few rules:
- Allergy is not a contagious disease.
- Only by eliminating the patient’s contact with the allergen will it be possible to cope with redness in the corners, runny nose, loss of appetite and weight loss in the child.
What to do
The red corner of the eye can be alarming to many. To get rid of the inflammatory process, it is necessary, first of all, to identify the main pathogen or identify the cause of the problem. If there is purulent discharge, then it is necessary to carry out local treatment, as well as general antibacterial therapy. In order to stop the proliferation of bacteria and the spread of infection, specialists prescribe broad-spectrum antibiotics. This may include ampicillin or various new groups of drugs, if the patient does not have an allergic reaction to such drugs. These drugs can be replaced with sulfonamides.
To get rid of puffiness, various eye drops are used that can remove redness and suppress itching. If a rash has formed on the skin, you can burn it with brilliant green, although this does not look attractive in appearance. This method is time-tested and effective. Among the eye drops, the most effective in combating any inflammatory process are the following:
- Erythromycin solution.
- Sulfacyl sodium.
- “Dexamethasone.”
- “Prednisolone.”
As an application, topical ointments can be applied to the affected area around the eyes. The tetracycline group is considered to be the most accessible and effective. If purulent discharge does not go away after antibacterial treatment, it is necessary to apply surgical correction to eliminate the causes of the inflammatory process in the corners of the eyes.
If the inflammatory process is allergic in nature, then it is necessary to eliminate the main cause of the allergy, after which the symptoms will subside on their own. If inflammation occurs due to physical impact, then traditional medicine methods are used, but they should be used only after consultation with an ophthalmologist.
In order for the treatment to be faster and more effective, it is necessary to remain calm and not strain the organs of vision. Healthy, adequate sleep and diet also play an important role in the treatment of diseases.
What diseases cause inflammation in the corner of the eye?
Inflammation in the corner of the eye is a fairly common symptom and is a manifestation of a violation of the integrity and functioning of the visual organs. There are many reasons for this, and only by identifying them can you get rid of redness, itching and other unpleasant signs of the inflammatory process.
Inflammation in the corner of the eye
The human body is often exposed to various inflammatory processes that develop for various reasons. It can be infectious or non-infectious. By their nature, all these processes have similar symptoms, but depending on the location or severity they may differ.
Whatever the reasons for the development of the inflammatory process, its nature inevitably leads to disruption of the basic functions of this organ. Inflammation in the corner of the eyes, despite the insignificant area of the lesion, affects a person’s quality of life, disrupting the organ’s perception of the environment, as well as blocking its basic functions.
The inflammatory process causes discomfort, bringing discomfort and pain. Symptoms can appear both on the outside and inside the corner of the eyes. The pain syndrome can occur suddenly or be temporary, or it can be permanent.
In addition, inflammation in the corners of the eyes is accompanied by unpleasant symptoms:
- itching;
- burning;
- redness of soft tissues in the affected area;
- swelling;
- redness of the sclera;
- discharge from the eye;
- increased lacrimation.
The appearance of at least one of these signs is a reason to immediately consult a doctor. The process cannot be delayed, since any violations can result in irreversible vision impairment or even loss.
What is the cause of inflammation
The skin around the eyes can become inflamed due to conjunctivitis, which is the result of mechanical injuries, exposure to chemical factors, or bacterial infections.
It can also be caused by natural physiological processes, for example, an ingrown eyelash.
But the main reason for the appearance of unpleasant symptoms are diseases that provoke damage to the mucous membrane, as well as soft tissues in this area.
Canaliculitis
A disease caused by infection in the tear ducts. The proliferation of bacteria provokes pain in the corners of the eyes, as well as swelling and redness. Tear production increases, and in addition to the usual tears, an admixture of pus may appear.
Bacteria enter the tear ducts not only from the environment through the opening in the corners, but also through the sinuses. Without treatment, the infection penetrates deeper and can impair visual function, making it much more difficult to relieve inflammation.
Obstruction of the tear ducts
In case of injury or tumor processes, natural tear production is disrupted. Excessive discharge or, conversely, dryness causes discomfort, and an inflammatory process develops on the outer and inner side of the corner of the eye. This pathology can cause visual impairment and often requires surgical intervention.
Dacryocystitis
The inflammatory process can affect not only the ducts, but also the lacrimal sac. Pain occurs in the inside of the eye. Severe swelling and excessive discharge appears. Instead of tears, purulent masses come out of the ducts. If you consult a doctor in a timely manner, surgical treatment can be avoided, and inflammation in the eyes can be relieved using conservative methods.
Angular conjunctivitis
This type of inflammatory process is caused by the Moracas-Axenfeld bacterium. When it gets into the eyes, it affects the skin on the eyelids and is localized in the corners. In addition to the usual redness and pain characteristic of inflammation, small cracks appear on the skin, which aggravate the symptoms. Pain and discomfort increase with blinking and touching.
Herpetic eye infection
The well-known herpes virus is often localized on the mucous membranes, including the eyes. It usually affects the areas around the eyes, penetrates deeper and multiplies in the tear duct.
When the infection reaches the ducts, symptoms appear in the corners of the eyes. In addition to pronounced swelling and redness of the skin and sclera, photophobia occurs.
Infection of the cornea with the herpes virus can lead to complete loss of vision.
Allergic conjunctivitis
Nasal congestion and watery eyes more than usual can be caused by an allergic reaction of the body. This type of damage to the corner of the eye is called allergic. It usually does not cause complications and can be successfully treated with antihistamines. After eliminating the allergen, everything goes away by itself.
Computer vision syndrome
Recently, vision has become increasingly deteriorating from prolonged exposure to computer monitors and television.
Fashionable smartphones and tablets have many different advantages, including safety for vision, but they still affect visual function over long periods of use.
Increasingly, this becomes the cause of the development of various kinds of disorders and leads to the appearance of unpleasant and dangerous symptoms. This syndrome does not require treatment, but reducing the load and getting proper rest is necessary for the symptoms to subside.
How to relieve inflammation in the corner of the eye
The inflammatory process can only be suppressed by identifying the causative agent or the cause of its development. If there is purulent discharge, local treatment is required first, as well as general antibacterial therapy.
To stop the proliferation of bacteria, as well as the spread of infection, broad-spectrum antibiotics are prescribed until the pathogen is identified. This may be the ampicillin group, if there is no allergy to these drugs.
They can be replaced with sulfonamides.
Eye drops are used to relieve puffiness; they remove redness and suppress itching. If a rash appears, it is burned with brilliant green, although this is unsightly from an aesthetic point of view, the method is effective and time-tested.
Among the eye drops effective in combating any inflammatory processes are:
- sodium sulfacyl;
- erythromycin solution;
- prednisolone;
- dexamethasone.
Topical ointments are used as applications to the affected area around the eyes. Tetracycline ointment is considered to be the most accessible and effective.
If purulent discharge does not stop after antibiotic therapy, surgical correction is performed to eliminate the causes of inflammation in the corners of the eyes.
When the inflammation is purely allergic in nature, it is enough to eliminate the cause of the allergy, and the symptoms will subside on their own. In case of inflammation as a result of injury or physical impact, traditional medicine methods are usually used, but this is only permissible with the permission of a doctor.
In order for the treatment to be faster and more effective, it is important to remain calm and not strain your vision. Nutrition and healthy, full sleep also play an equally important role.
How to relieve inflammation at home
You can get rid of discomfort, remove swelling and other manifestations of the disease at home yourself. For conjunctivitis of an infectious nature, compresses from a decoction of elderberry or cornflower are used. If the eyelids are affected, it is enough to apply almond oil or calendula tincture to the affected area.
Chamomile decoction
For any pathological processes, chamomile decoction will be useful. It soothes delicate skin and inhibits bacterial activity.
To prepare the infusion, you need to brew 2 teaspoons of dried chamomile flowers with one glass of boiling water and let it brew.
Mint decoction
To prepare, you need to brew 2 tablespoons of dry herbs in half a liter of boiling water. It is important to boil the broth for no more than 10–15 minutes and let it cool. They moisten cotton swabs and apply to the eyes before going to bed.
Any pathological changes cannot be self-medicated, so when the first symptoms appear, it is important to seek help from a specialist.
Source: https://provospalenie.ru/lico/v-ugolke-glaza.html
Associated symptoms
With the progression of dangerous ophthalmological disorders, in addition to the fact that when blinking and when the eyelids are closed, the left or right eye hurts, the patient is bothered by other symptoms that are impossible not to notice. The characteristic features are:
- itching, redness and tingling of the skin around the eyeball;
- inflammation and swelling of the inner and outer corners of the eye;
- profuse lacrimation;
- purulent discharge;
- deterioration of visual function.
Sometimes infectious pathologies are accompanied by headaches localized closer to the ear or near the temple. With such symptoms, you need to urgently make an appointment with an ophthalmologist, since infectious eye pathologies often lead to inflammation of nearby organs - ear, throat, nose. In advanced cases, the infection penetrates the brain, and the patient develops meningitis, which often causes death.
When to see a doctor urgently
There are a number of situations in which visiting a doctor is mandatory.
- If a problem occurs in an infant, you should definitely consult a pediatrician.
- It is recommended to visit an ophthalmologist in a situation where you cannot cope with the redness with usual means and the child complains of vision problems.
- If hyperemia is accompanied by a rise in temperature, runny nose, cough, sore throat, this is a viral infection that requires adequate treatment.
- There is increased swelling of the eyes and discharge of pus.
- In addition to redness of the eyes, there are periodic pains in the head, blurred vision - see a pediatrician, who will most likely refer you to a neurologist.
Treatment
In order for the fight against redness around the eyes to be effective, it is important to correctly identify the cause of this symptom and follow the doctor’s recommendations. If you suspect chronic tonsillitis, make sure for yourself that there is a source of infection by carefully examining the baby’s tonsils and throat
If you find white or yellow plaque there, consult a doctor immediately. In this case, there is no need to self-medicate: by doing so, you can simply waste time and expose your baby to complications from the cardiovascular system and gastrointestinal tract
If you suspect chronic tonsillitis, make sure for yourself that there is a source of infection by carefully examining the baby’s tonsils and throat. If you find white or yellow plaque there, consult a doctor immediately. In this case, there is no need to self-medicate: by doing so, you can simply waste time and expose your baby to complications from the cardiovascular system and gastrointestinal tract.
If you associate red circles under your child’s eyes with an allergy, then it is necessary to identify the allergen and eliminate contact with it. Of course, here you will need the help of a qualified specialist.
For caries and other diseases of the oral cavity, you will need to consult a dentist. In addition, teach your child from an early age to regular oral hygiene procedures. If vegetative-vascular dystonia is detected, you will need the help of a neurologist. The doctor will prescribe a gentle regimen for the baby, frequent walks in nature, moderate physical activity and regular rest.
In many cases, the appearance of redness under the eyes is a sign of the purely individual structure of the subcutaneous tissue. This is often inherited by the baby from his parents. In this case, light massages will help improve blood circulation and skin color under the eyes.
What to do if your eye is festering, see here.
Symptom treatment
Treatment is the main element of eliminating red eye symptoms as quickly as possible. If the situation is difficult, you need to give the child the opportunity to get a good night's sleep and also reduce visual stress during the day.
The following methods cannot be used during treatment:
- washing with saline solution or potassium permanganate;
- heating using a dry method (for example, using sand);
- instill half the dose of medicinal drops for prevention purposes.
Is it possible to solve the problem without medication?
First aid consists of washing the eyes with a neutral substance - clean water or miramistin. It is worth visiting a doctor in any case: this will eliminate the risk of possible complications. If the situation is acute, you must go to the hospital immediately. The doctor will decide whether to take medications.
Medicines
Medications are used for infectious and allergic processes that affect the mucous membrane of the organ of vision. Any medications are used strictly as prescribed by a pediatrician or ophthalmologist.
Prevention
To prevent the development of red eyes, it is recommended to adhere to the following rules:
- wear contact lenses for a limited time;
- to sleep more;
- Visit an ophthalmologist annually to check the condition of your eyeballs;
- spend less time on the computer, TV, phone;
- wear protective equipment and masks for people who work in conditions of increased risk of eye damage (welders).
Always remember hygiene. Before going to bed, do not forget to wash off your makeup. Wash your hands regularly. Do not strain your eyesight by spending a long time in front of a computer monitor. When working with a welding machine, use a protective mask.
You can avoid pain around the edges of the eye by observing the following measures:
- visual hygiene;
- avoiding traumatic situations;
- avoiding contact with infectious patients;
- regular examination by an ophthalmologist.
You can take away a couple of tips from an interview with a professional ophthalmologist about maintaining visual hygiene.
Hygiene during illness
Treatment of red, watery eyes in children requires compliance with the following hygiene rules:
- The parent who will handle the child’s visual organ washes his hands thoroughly.
- Even if only one eye is affected, both must be treated.
- A separate sterile napkin or cotton pad is used for each visual organ.
- During the procedure, the child is in a horizontal position.
- Rinse the eyes with a stream of furatsilin solution from a clean pipette.
- To instill or lay the ointment, the lower eyelid is gently pulled back without touching the sclera.
- The baby must have his own towel.
- Parents should keep their child's hands clean.
- You should not allow your baby to scratch his eyes.
- Bacterial and viral conjunctivitis are contagious, so other family members need to especially carefully observe the rules of personal hygiene and avoid contact of the patient with newborns.
- You should ventilate the apartment more often and carry out wet cleaning daily.
Traditional methods for getting rid of redness under the eyes
- Before the doctor arrives, you can wash the child’s face with baby wash and make a poultice on the eyes with a decoction of chamomile or tea leaves. You can also make compresses from infusions of other medicinal herbs. They relieve itching, inflammation and flaking. You should definitely explain to your child that you should never touch or rub your eyes with your hands.
- Cottage cheese mask. To remove redness under the eyes, you need to mix cottage cheese and sour cream in a 2:1 ratio. Then put a certain amount of the resulting mass on a cotton swab and make a compress on the eyes (15 minutes).
- Potato mask. Grind the raw vegetable. Place the resulting mixture on a thin cloth and apply a compress to the affected area (20 minutes). After the procedure, rinse your face with water and apply baby cream.
- Cold treatment. It should be done infrequently and for no more than 3 minutes.
- Grate the unpeeled pumpkin. Wrap the resulting pulp in thin cloth or gauze and make a compress (20 minutes). This procedure can be carried out several times in a row, taking a break for 10 minutes.
- Wash the leaves of the young Kalanchoe plant thoroughly, grind it into a pulp and apply it to the eyelids (15 minutes).
- Aloe helps with red eyes. The plant must be more than 2 years old for more effective treatment. Aloe juice is dropped into the eyes (2-3 drops). Drop honey into a large spoon, mix thoroughly and drop the resulting mixture into your eyes (2-3 drops). There may be a feeling of burning and discomfort, which quickly passes.
- Dill seed lotion. Prepare a decoction of this plant in a steam bath and apply compresses to the eyes.
- Marshmallow root lotion. A few grams of the plant must be poured with cold water and left for 24 hours. Then apply compresses to the eyes.
- Lotion from two-leaved mynika. Pour half a small spoon of the plant into a cup of boiling water, leave for half an hour and strain well. Use the compress morning and evening.
- Compress made from infusion of blue cornflower flowers. Brew a large spoonful of the plant in boiling water and leave for 1 hour. Before the procedure, the infusion must be strained.
- Make a mixture of onion broth and honey and wash your eyes with it, but no more than 3 times a day.
- Pour a cup of boiling water over the cucumber peels. Add a little soda to the broth. Leave for 20 minutes, then strain. Use as an eye wash and as a lotion.
You can use traditional medicine to treat a child, but only after consulting a doctor. Some drugs have a very strong effect on the child’s body and can be dangerous.
It should be remembered that it is important to cure not the symptoms (redness under the eyes), but the very cause of the disease. And self-medication will not help here. Parents definitely need to teach their child to maintain hygiene, exercise and eat right.
Then the occurrence of infectious diseases will be minimized, the immune system will be strengthened and the baby will be healthy
Parents definitely need to teach their child to maintain hygiene, exercise and eat right. Then the occurrence of infectious diseases will be minimized, the immune system will be strengthened and the baby will be healthy.
Children always cause anxiety, and when there is a suspicion that there are health problems, then they generally cause panic. For example, if redness appears somewhere on the skin. The site for moms supermams.ru understands that you can think the worst and panic. But you shouldn’t react this way to every redness around your child’s eyes. Although many pediatricians and, following them, caring parents are well aware that the skin in the eyelid area is thin, and therefore allows you to monitor the slightest changes in your health.
What treatment is appropriate?
What treatment regimen will be prescribed by the doctor directly depends on the factors that caused the disorder:
Breasts are prone to allergic reactions.
- Allergy. Antihistamines and rinsing with furatsilin are mandatory. It is not recommended to use herbal infusions due to the possible increase in allergic reaction to herbal components.
- Infection. To treat bacteria, antibacterial drops or ointment (Cephalosporin, Tetracycline) are prescribed. If the infection is viral, do not rush to prescribe medications; after 10 days, the symptoms will begin to go away on their own.
- Inflammation of the mucous membrane. For treatment, immunostimulating drugs and glucocorticoids are used to remove toxic substances from the body (Pilocarpine, Betaxolol). To reduce redness and relieve irritation, Taufon eye drops are prescribed.
- Obstruction of the lacrimal canal. The problem is eliminated surgically; in addition, you need to massage the area of the tear duct and drip eye drops (Vitabact).
- Blepharitis. Complex therapy with antibacterial drugs will be required.
ethnoscience
Strong tea leaves are suitable for washing sour eyes.
To alleviate the condition and to help with medications, therapy can be carried out with publicly available means, such as:
- Cucumber. Vegetable slices should be dipped in water and applied to closed eyes for 5 minutes.
- Potato. Grind it into a fine grater and squeeze out the juice. Then you need to moisten a cotton pad in it and apply it to the eye area. Such compresses relieve redness and reduce vascular tension.
- Milk. For a wet lotion, you need to warm it up, soak cotton wool in it and apply it to your eyes for 10 minutes.
- Tea. Make a strong decoction of black tea, soak a cotton pad in it and apply for 15 minutes. Repeat up to 3 times a day.
Traditional medicine recipes are not relevant in every case, so you must obtain permission from a doctor to use any medicine to treat a child.
Categories
AllergistAnesthesiologist-resuscitatorVenereologistGastroenterologistHematologistGeneticGynecologistHomeopathDermatologistPediatric gynecologistPediatric neurologistPediatric urologistPediatric surgeonPediatric endocrinologistNutrologistImmunologistInfectious disease specialistCardiologistCosmetologistSpeech therapistElorologistMammologistMedical lawyerNarcologistNeurologistNeurosurgeon NephrologistNutriciologistOncologistOncourologistOrthopedist-traumatologistOphthalmologistPediatricianPlastic surgeonProctologistPsychiatristPsychologistPulmonologistRheumatologistRadiologistSexologist-AndrologistDentistTherapistUrologistPharmacistPhytotherapistPhlebologistSurgeonEndocrinologist
Categories
AllergistAnesthesiologist-resuscitatorVenereologistGastroenterologistHematologistGeneticGynecologistHomeopathDermatologistPediatric gynecologistPediatric neurologistPediatric urologistPediatric surgeonPediatric endocrinologistNutrologistImmunologistInfectious disease specialistCardiologistCosmetologistSpeech therapistElorologistMammologistMedical lawyerNarcologistNeurologistNeurosurgeon NephrologistNutriciologistOncologistOncourologistOrthopedist-traumatologistOphthalmologistPediatricianPlastic surgeonProctologistPsychiatristPsychologistPulmonologistRheumatologistRadiologistSexologist-AndrologistDentistTherapistUrologistPharmacistPhytotherapistPhlebologistSurgeonEndocrinologist
conclusions
If, then this requires immediate contact with a specialized specialist - this is a mandatory procedure if you have determined that the child did not injure his eye at home. The causes of red eyes can be different, ranging from a foreign body getting into it, to glaucoma, the treatment of which requires surgery or taking medications under the supervision of a doctor. A red eye requires careful care - lotions from chamomile decoctions, minimizing eye strain, eliminating stress and nervous experiences. The child should sleep well and suffer from conjunctivitis and other viral diseases.
Quite often, parents have to deal with a variety of health problems in their child. At almost any age of a baby, you can notice an unusual redness in his eyes.
There can be many reasons for this and it is not always worth sounding the alarm. Of course, if the redness of the eyes is quite severe and lasts for quite a long time, it is better to immediately consult an appropriate doctor for advice.
Treatment options
If a child’s conjunctiva of the eye turns red, it is imperative to show it to an ophthalmologist if there are the following additional signs :
- limiting the time spent watching TV and staying at the computer does not reduce the severity of symptoms;
- over-the-counter medications do not help;
- redness is accompanied by sticking of the eyelids in the morning from purulent discharge;
- photophobia develops;
- the child complains of blurred vision and gets tired quickly when the eyes are stressed.
If you consult a doctor in a timely manner, there is always a chance to start treatment on time, and therefore to eliminate the pathology before it leads to the development of serious consequences and complications.
General approach to treatment and prevention
Treatment for this type of redness depends entirely on what disease is diagnosed .
Important! In addition to the fact that parents will have to independently instill and place the prescribed products under their eyelids, it is also important for them to comply with the general requirements for child care and medical procedures:
- Without the approval of a doctor, you should not perform warming procedures on your own . If redness of the eyes occurs due to the development of inflammatory processes, such actions will only contribute to the intensification of pathological processes.
- During the treatment period, it is necessary to reduce the load on the visual organs as much as possible . This means minimal time spent in front of the TV and computer (and if possible, it is better to exclude them altogether).
- The child should go to bed on time and get enough sleep - adequate sleep will eliminate unnecessary irritation of the visual organs.
- Particular attention must be paid to hygiene . Before instilling drops into a child, the adult who will carry out this procedure should wash their hands thoroughly with soap. In turn, when washing, the child should use only a personal towel, so as not to introduce additional infection into the eyes or transmit the disease to other family members.
- If the eyes are severely inflamed and purulent discharge is present, the organs of vision can be washed with furatsilin, tea or chamomile decoction as necessary .
Know! Self-medication for such a symptom is undesirable (at least without the consent of an ophthalmologist or pediatrician). Also, you should not use medications on the advice of friends and family.
Only a specialist can prescribe medications , but before doing this, the child’s vision organs must be examined to accurately determine the cause of the redness.
conclusions
A healthy child is happiness for parents. In many ways, this happiness depends on the care for the baby that responsible mothers and fathers show. Do everything for the healthy development of your child, give him a personal example of attitude to nutrition and a healthy lifestyle. After all, he learns from what he sees in his home. Do not treat the baby yourself. If you see redness in the eyelid or around the eyes, contact a medical facility immediately. Otherwise, you may develop an allergy or other disease such as conjunctivitis in children.
Information from this link will help you understand that your child has purulent conjunctivitis.
Causes
Know! Among the reasons why the corners of a child's eyes turn red, there are several diseases that pose a potential threat to vision.
This symptom most often indicates the following disorders and diseases:
- foreign bodies getting into the eye,
- visual fatigue,
- conjunctivitis of various origins,
- uveitis (inflammation of the blood vessels of the eyes),
- vegetative-vascular dystonia,
- dacryocystitis (obstruction of the tear ducts),
- allergic reaction,
- glaucoma,
- blepharitis.
A non-specialist will not be able to determine what kind of disease the reddened corners of the eyes indicate, so in this case, independent treatment is contraindicated.
Only an ophthalmologist or pediatrician after examination can diagnose and prescribe appropriate .