Bronchitis in infants is a serious inflammatory process involving tissue from the bronchi. Most often, exacerbation occurs during periods of severe cold - autumn and winter. In infants, the disease begins to progress due to deterioration of the immune system or poor development of the respiratory muscles. Additionally, it should be noted that in children under one year of age the disease is much worse. Certain medications should not be used to treat an infant. A positive effect can be achieved through traditional medicine methods.
Development mechanism
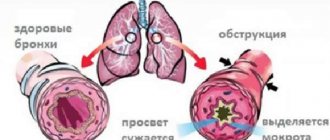
Bronchitis is an infectious disease characterized by the development of an inflammatory process in the respiratory system and an increase in the production of bronchial secretions released during coughing.
Children's doctors say that symptoms of bronchitis are observed in every fifth newborn baby: this phenomenon is due to the weakness of the immune system and the anatomical structure of the child's respiratory organs.
Factors contributing to bronchial inflammation include:
- Defective structure of the bronchi: lack of lumen between them.
- The viscous consistency of bronchial secretions complicates the process of its removal during coughing - leads to the accumulation of mucus.
- Weakness of the immune system. Since the baby’s immunity is just developing, there is a high probability of inflammation of the bronchi due to infection with viral agents.
- Frequent allergic reactions. The baby's body is highly sensitive - this explains the high risk of developing allergies, in most cases food.
- Hypothermia of the child's body.
The mechanism of development of the pathology is as follows: the mucous membrane of the bronchi, being under the influence of pathogenic bacteria, becomes severely inflamed and swells. The formation of edema leads to a narrowing of the lumen between the bronchi and a deterioration in the conductivity of oxygen into the lungs. As a result, the synthesis of viscous exudate increases: in order to slow down the production of mucus, the bronchi often contract, resulting in local spasm.
The manifestation of obstructive bronchitis in infants is preceded by the development of an acute respiratory infection, which is characterized by damage to the upper respiratory system.
There are many types of pathogenic microorganisms that infect the human body - this explains the fact that the risk of infection for a baby is very high.
Symptoms
Symptoms of bronchitis in children under one year of age, as a rule, do not differ in variety. The main sign of a developing disease is a cough. Dry, paroxysmal, it is often accompanied by difficulty breathing and shortness of breath. The temperature rises. Over time, the cough turns from dry to wet, and sputum begins to be released. Since the airways of a newborn are quite narrow, it greatly complicates breathing. It becomes noisy and whistling.
The child has wheezing and whistling sounds in the chest on both sides, and it is difficult to exhale. In medical practice, this condition is called bronchial obstruction. The danger of bronchitis during the neonatal period lies in the fact that, as a rule, bronchial obstruction syndrome develops in most children, and in addition, bronchioles (the smallest airways) may be involved in the process. In this case, symptoms of respiratory failure come to the fore.
Symptoms of the disease also affect the general condition of the newborn. The child is very restless. He may experience dry mouth and lack of tears when crying. He refuses breastfeeding and formula, and the amount of urine excreted decreases.
Classification
There are two forms of bronchitis - acute and chronic.
Acute bronchitis is the result of infection of the body by pathogenic microorganisms - influenza virus, adenovirus or rhinovirus.
Less commonly, acute inflammation develops when bacteriological microflora, fungus, toxins or allergens enter the respiratory tract.
Chronic bronchitis occurs with frequent recurrences of colds, regular hypothermia of the body, as well as prolonged exposure to toxic substances on the respiratory system.
What to do is right?
Now let's logically figure out what conditions need to be created to help a baby with viral obstructive bronchitis remove the already accumulated mucus and not provoke the formation of new one?
- We reduce the room temperature to 18, maximum – 20 degrees. Too warm air contributes to the thickening of mucus, and we need to achieve the opposite. In this case, the baby needs to be dressed warmly so that he does not freeze (warm socks, hats and other clothes are welcome, but keep the air temperature down!).
- We provide frequent ventilation. Firstly, this will help maintain a low air temperature, and secondly, it will provide additional oxygen for breathing (after all, it is difficult now).
- We humidify the air to 60-70%. Throw wet towels on the radiators, spray the curtains, bring a boiling kettle into the room, install humidifiers - there are many ways. Of course, this will require much more effort from parents than stuffing the baby with a bunch of medications. But the choice here should be obvious - all for the sake of the baby’s health! Humidifying the air will thin the mucus and prevent it from thickening.
- Provide the baby with plenty of fluids. This will also help thin the mucus.
- We take care of nasal breathing. If we are talking about a viral infection, the baby’s nasal passages will also be blocked with mucus. It must be sucked out, the nose should be washed, and salt solutions should be instilled. We use vasoconstrictor drops so that the baby breathes through his nose - this will warm and purify the inhaled air.
- No imprisonment! If your little one’s temperature stays below 37.5, take him for walks in the fresh air more often. It will help to quickly cope with the misfortune and strengthen the little body.
- Maximum vertical! A supine position and bed rest are needed only for periods of high fever. After this, the baby needs to take a vertical position as often as possible. If he is already sitting down on his own, sit him down. If not yet, carry it in your arms in a vertical position - it provides much greater coughing force and speeds up the healing process.
With this treatment, you can limit yourself to a minimum amount of medications and a minimum period of time.
Symptoms
Signs of bronchitis in infants are determined by the form of the inflammatory process. Symptoms become more pronounced if the infectious disease develops in an acute form: specific signs appear within a few hours.
Chronic inflammation of the bronchi in a baby is difficult to diagnose in a timely manner, which is due to the asymptomatic development of the pathology.
The main factor that provokes the appearance of symptoms of bronchitis is the lack of quality treatment for colds. Parents often interrupt drug therapy, relying on the normalization of their baby’s well-being. As a result, the airways become inflamed again, and the immune system begins to weaken even more: a relapse develops.
If bronchitis in a newborn is of an allergic nature, unpleasant symptoms appear against the background of exposure to the allergen on the child’s body. Bronchitis in infants is manifested by the following symptoms:
- hoarseness occurs as a result of accumulation of sputum in the upper respiratory tract of the newborn;
- pain and discomfort in the throat;
- separation of mucous secretions during coughing;
- difficulty breathing as a result of the development of bronchospasm.
Another symptom characteristic of bronchitis is a cough, which at an early stage of the inflammatory process is dry. As the infection develops, a mucous secretion begins to accumulate in the bronchi, which is released during the cough reflex. If inflammation occurs against the background of bacterial damage, the sputum contains impurities of pus. In the event that bronchitis is provoked by viral agents, clear, sometimes green-tinged, bronchial mucus is released.
On average, a symptom of inflammation such as cough bothers a baby for two weeks. If this symptom persists after all other symptoms have stopped, you should contact your pediatrician.
The inflammatory process that develops in the bronchi provokes an increase in the body temperature of a small patient to 38 degrees: on average, it persists for 7 days.
If bronchitis in an infant is not accompanied by a high temperature, this indicates that a focus of inflammation in the respiratory system has formed due to exposure to an allergen.
Symptoms characteristic of bronchitis are aggravated by lethargy and tearfulness, poor appetite, and general weakness of the child. During the day, the baby is constantly capricious and demands attention, and at night he often wakes up and refuses mother’s milk. The degree of manifestation of symptoms is determined by the degree of damage to the bronchial mucosa of the infant.
Prevention and infant regimen
creating optimal living conditions will help reduce the number of relapses, as well as the number of attacks during the acute period :
- Frequent wet cleaning and ventilation.
- Limiting contact with allergens, cigarette smoke, construction dust.
- Maintaining high humidity (60%) and low temperature (20 degrees) in the room.
- The child should be given water more often to give the body the opportunity to liquefy mucus and remove it.
- There is no need to force your baby to eat.
Obstructive bronchitis looks worse than it actually is . Many parents begin to treat their child with potent drugs .
However, this condition is easily amenable to standard treatment . Don't panic. Consult your doctor for an accurate diagnosis and maintain the correct temperature and humidity in your baby's room.
Diagnostics
Examination of a newborn with suspected bronchial inflammation begins with an examination by a pediatrician. The pediatrician uses a stethoscope to listen to the baby's chest to detect wheezing and whistling sounds, as well as to evaluate respiratory function.
Afterwards, the doctor sends the little patient for a general blood test, which will determine the content of leukocytes: a large number of them indicates the presence of a focus of inflammation in the body. A blood test allows you to assess the condition of eosinophils: their excess is a symptom of the development of an allergic reaction.
An informative method for diagnosing a respiratory disease is sputum analysis, with the help of which a laboratory technician determines the type of bacterial pathogen. If the baby has difficulty breathing, it is also necessary to take a blood test to evaluate its composition of gases.
To exclude the possibility of inflammation of the lungs, the doctor sends the baby for an X-ray examination of the sternum.
Directions of therapy
Treatment of bronchitis in an infant should be carried out only under the supervision of a doctor. For a viral disease, antiviral drugs are prescribed - “Interferon”, “Viferon”, “Kipferon”, “Immunoflazid” and others. Komarovsky believes that in most cases there is no need for them, since within 5-7 days the baby’s body will defeat the infection itself. But many doctors and parents believe that the use of such drugs speeds up recovery and prevents complications.
Treatment for bacterial bronchitis involves oral or injectable antibacterial drugs. The fact that the pathological process was started by bacteria is indicated by symptoms such as:
- purulent nature of sputum discharged after coughing
- very serious general condition
- no improvement on the 4th day of illness
- increased body temperature for more than 7 days
- an increase in the level of certain types of white blood cells in the blood
Regardless of the type of bronchitis, the following are used:
- Antipyretics in the form of suppositories or syrups - paracetamol, ibuprofen in recommended age-specific doses. It is believed that it is not worth lowering the temperature to 38.5 ºС, but with a child under 6 months it is better to be safe and give medicine.
- Vasoconstrictor drops based on phenylephrine or oxymetazoline, if the baby has difficulty breathing through the nose due to swelling or excessive mucus secretion. The average period of use is 3-5 days, but no longer than 7. In addition, it is worth regularly rinsing the baby’s nose by instilling saline solution.
- Agents that thin mucus and facilitate its removal. Vegetable - with marshmallow, ivy, licorice, thyme and others. Synthetic - ambroxol, bromhexine, acetylcysteine and others. Their use in infants is permissible only as prescribed by a doctor in situations where viscous mucus cannot come out freely.
Komarovsky insists that the treatment of bronchitis is based largely not on taking medications, but on proper child care. Key points:
- clean, cool (16-20 ºС) and humid (50-70%) air in the room where the baby is
- drink plenty of fluids – oral rehydration solutions, herbal teas, dried fruit compote, raisin decoction
If these rules are followed, inhalations and medications will not be needed. The sputum will remain liquid and the baby will be able to cough it up easily.
Principles of treatment
Treatment of bronchitis in infants is aimed at relieving the negative impact of the factor that provoked the formation of a focus of inflammation. If the pathology has a viral etiology, drug therapy is based on taking antiviral drugs - Arbidol or Tamiflu. Damage to the bronchial mucosa by bacterial microflora is an indication for antibacterial therapy.
To normalize body temperature, it is recommended to give the baby the antipyretic drug Paracetamol. To facilitate the process of sputum separation, the child is recommended to take expectorants - Lazolvan and ACC.
If necessary, the pediatrician can also prescribe mucolytic drugs: they must be taken with extreme caution, as they increase the synthesis of sputum.
A lingering dry cough is an indication for taking antitussives that contain codeine. If your baby is bothered by a cough with copious amounts of sputum, it is not recommended to take antitussive medications. To relieve bronchial spasms, the bronchodilator "Atrovent" is used.
Drinking plenty of fluids will help speed up the body's recovery process. To improve the baby’s well-being, physiotherapeutic procedures such as electrophoresis and therapeutic exercises can be used.
Massage for obstructive bronchitis in infants
Physiotherapeutic procedures are a prerequisite for successful treatment of the disease. Massage is considered the most effective for infants. It helps ease the passage of mucus and improves blood circulation. For infants, massage is an indispensable procedure, since they cannot cough up mucus on their own. In this case, when carrying out it, the following rules should be observed:
- Expectorants must be taken before the massage.
- The procedure is carried out no earlier than 2 hours before bedtime.
- The duration of one massage session is 30 minutes. It is recommended that infants carry out the procedure 2-3 times a day for a week.
- Massage movements (stroking, rubbing) are performed in the direction from bottom to top.
Possible complications
Advanced bronchitis provokes the development of complications:
- Airway obstruction.
- Heart failure.
- Respiratory failure.
- Pneumonia in chronic form.
- Asthma of bronchial type.
- Inflammation of the lung tissue.
The manifestation of inflammation symptoms in a baby is an indication for an emergency visit to the pediatrician. If the baby’s parents ignore the signs of bronchitis or self-medicate, the inflammatory process worsens, causing dangerous complications to develop.
How does bronchitis occur?
The cause of the inflammatory process is often a common virus , so the disease begins with a standard picture: a reddened throat, dry cough and fever.
Then the cough becomes the main symptom that worries the baby, and turns into a productive form. The bronchi produce a lot of mucus, which is successfully expectorated if favorable conditions are maintained in the room.
The cough is accompanied by respiratory failure , and parents begin to fear the child’s next attack. Treatment and recommendations for parents depend on the cause of bronchitis. With proper comprehensive treatment, the symptoms will go away in 2-3 weeks, but the residual effects may last a little longer.