How many pathologies await our children in early childhood! Many mothers have lost their minds in search of good pediatricians, gastroenterologists, pulmonologists and neurologists so that they can examine their child and prescribe treatment. After all, in young children, the digestive, nervous and respiratory systems often malfunction. Respiratory diseases account for almost half of the number of pathologies in childhood. It especially frightens mothers when their children cannot exhale and inhale air, turn blue and have difficulty clearing their throat. This indicates the development of obstructive bronchitis.
Description of the pathology
Obstructive bronchitis in children often occurs between the ages of 0 and 3 years. This is a serious pathology of the respiratory system, as the patency of the bronchi is disrupted, making it difficult for the child to breathe. How can you live without breathing? Therefore, if this condition is not treated in a timely manner, the baby’s life is at risk.
Obstructive bronchitis in children develops in a matter of minutes, their condition worsens with every second. But this is not a reason to treat your baby with various unnecessary drugs, so below we will look at the basic principles of determining the disease, the causes of its occurrence and help with this condition.
Basic principles of treatment of bronchitis in childhood
Bronchitis is treated exclusively with antibiotics. If bronchitis is not treated correctly, it can develop into pneumonia, pleurisy, or mediastinitis. These conditions are extremely life-threatening for the child and require treatment in the intensive care unit. Therefore, it is easier to prevent the development of these conditions with the right treatment. The antibiotic is selected taking into account the pathogen.
Currently, there is a huge classification of chemotherapy drugs. Most often, a broad-spectrum drug is used, for example, third or fourth generation cephalosporins. Penicillin antibiotics are used in children of the first year of life. The most common option is amoxicillin in the form of an emulsion. Therapy for bronchitis must be comprehensive and include vitamin therapy, immunomodulators, and herbal medicine. During illness, the child must remain in semi-bed rest. The diet should be predominantly alkaline, high in calories, but not heavy on the stomach. Porridges and broths are ideal. For infants, you need to stop feeding by the hour and give breastfeeding on demand. And most importantly, surround your child with love and care, because the child’s moral comfort is the key to successful treatment. Be healthy!
We advise you to read: Is residual cough after bronchitis dangerous, does it need to be treated?
Manifestations of the syndrome
The symptoms and treatment of this pathology are closely related, since they often manage only with symptomatic therapy. In severe cases, basic therapy is used, which must be used even in the intervals between attacks.
Main signs of the disease:
- The child behaves restlessly until bedtime.
- In the presence of acute bronchitis, even from a distance you can hear wheezing and whistling while breathing.
- If you listen or listen to the child's chest using a phonendoscope, you will hear bubbling. But these are not wet rales, and they are heard in several places and go away after coughing.
- Shortness of breath and suffocation. This is the main sign of the syndrome; while inhaling, the baby tenses.
- Exhausting cough.
- The child is breathing quickly. It is necessary to compare with the norm: up to six months the baby normally breathes 60 times per minute, from 6 to 12 months he breathes 50 times, from one to five years - 40 times.
- The nasolabial triangle turns blue.
Chronic form of obstruction
Treatment of obstructive bronchitis in children should begin immediately, at the first symptoms. Treatment of acute and chronic forms of obstructive bronchitis is slightly different. Chronic obstructive bronchitis periodically occurs as a result of infection and proliferation in the respiratory tract. It manifests itself almost like an attack of bronchial asthma, but there are no allergic causes. This syndrome in its chronic form begins due to infection or aspiration (a foreign body entering the respiratory tract).
Laboratory diagnostics
- General blood analysis.
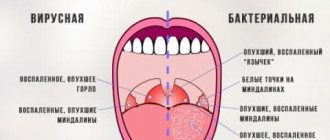
It is better to take blood for analysis at the peak of the temperature. Here the doctor first of all pays attention to the presence of signs of an inflammatory process in the blood. These include: an increase in the level of leukocytes, erythrocyte sedimentation rate (ESR), hematocrit, the appearance of C-reactive protein, plasma cells, and possible changes in the shape and size of erythrocytes (anisocytosis and poikilocytosis). Sometimes there is an increase in hemoglobin due to an increase in hematocrit, but in the stage of bronchial obstruction and increasing respiratory failure, the level of hemoglobin and red blood cells may be below normal. The leukocyte formula is of great importance in the differential diagnosis of types of bronchitis. If the number of eosinophilic leukocytes is increased, then we can safely say that bronchitis is of an allergic nature.
- General urine analysis.
Drugs and methods for treating obstructive syndrome
Treatment in adult children and children differs in the use of drugs, their dosages and conditions. Children under 2 years of age are treated in a hospital under the supervision of pediatricians. There they determine how to treat the babies.
Features of Baby Mode
If the temperature rises due to the spread of infection, the child needs bed rest. Observations show that most children can behave actively after an attack of obstruction. But it is important to prevent physical overload for them.
Therapeutic activities include walks in the fresh air. It is recommended to walk for an hour twice a day in a park area away from roads and crowds.
Nutrition
Avoid using substances that can cause allergies during illness. Do not use fatty, fried, or too salty foods.
It is necessary to give children foods that are easily digestible and rich in vitamins. It is also important to ensure plenty of fluids: apple juices and compotes, herbal decoctions, vitamin teas.
Hygiene
During treatment, it is important to ensure the hygiene of the child’s room: do wet cleaning, do not use irritating detergents, limit the intake of smoke from smoking.
Use of drugs
The doctor determines how to treat the baby after an examination. He, together with the parents, decides on the advisability of hospitalization based on the child’s condition. Several groups of drugs are used for treatment.
Bronchodilators
These are drugs to relieve bronchospasm. They expand their lumen, helping to increase the flow of oxygen into the respiratory tract and nourish all tissues of the body. The use of these drugs is extremely important for obstructive bronchitis in children; treatment with them should begin during an attack.
Young children are given drugs in syrup form to make them easier to take. Also, after 2 years, it is possible to use inhalations with these substances:
- Ascoril;
- Clenbuterol;
- Salmeterol;
- Berodual;
- Salbutamol.
Some of them are diluted with saline solution for inhalation therapy. They relieve bronchospasm within 15 minutes.
Hormonal agents
If the desired effect is not achieved, hormonal agents are used. But their frequent use causes addiction and side effects. These are drugs such as Pulmicort, Budenit and others.
Mucolytics and expectorants
Treating obstructive bronchitis in infancy is quite difficult. For this purpose, bronchodilators and supportive therapy are used. Older children are prescribed mucolytics and expectorants to thin and remove mucus.
Preparations based on ambroxol, carbocisteine, and plant extracts are prescribed. The following products and their analogues are often used:
- Ambrobene;
- Lazolvan;
- Flavamed;
- Bronchicum;
- Gerbion;
- Gedelix;
- Eresapal.
Inhalation using a nebulizer helps cure obstructive bronchitis very well. You can simply breathe in saline or alkaline solutions. They do not have a therapeutic effect, but they help children cough up mucus and soften coughing attacks. Then you can use the drugs in solutions for inhalation. They are diluted with saline for better penetration into the bronchi and absorption.
This therapy sometimes works better than tablets and syrups. When small particles of medicinal liquid are inhaled, they immediately settle on the mucous membranes, beginning their effect. Whereas medications in tablet form or syrups must first go through chemical processes in the gastrointestinal tract, and then begin their effect on the bronchial mucosa.
When treating a cough, it is important to consult a doctor about what to use and when to do it. Mucolytic agents are used at the beginning of treatment to achieve the desired consistency of sputum, then a transition to expectorants occurs for better and faster removal of pathological mucus from the lower respiratory tract. And these are completely different drugs. Important: mucolytics are not used for children under 2 years of age, since they are physiologically unable to cough up large amounts of mucus.
Allergy medications
The release of histamines into the bloodstream produces swelling, itching, cramping and other allergic reactions. For bronchospasm caused by obstruction, it is necessary to give antihistamines if the child is prone to allergies.
Experts have come to the conclusion that an immune response to the resulting obstruction is present in almost all cases. Therefore, the use of antihistamines is considered justified for all children with obstructive syndrome.
Zirtec and its synonyms are used for small children from six months of age; after 2 years, the use of Loratadine, Clearitin, Erius, Eden is allowed. After 5 years, Telfast and its synonyms can be used.
Immune stimulation
To help the child get rid of the disease as quickly as possible, doctors prescribe immunomodulatory drugs. By the way, the antiviral drugs used for the infectious nature of obstructive bronchitis also stimulate the functioning of the immune system. They are used in different forms of release: rectal suppositories, tablets, drops, syrups. The following drugs are often used:
- Viferon;
- Laferobion;
- Immunoflazid;
- Groprinosin;
- Arbidol;
- Kagocel and others.