Characteristics of the disease
Biliary dyskinesia (BDH) is a functional disorder of the motility of the bile ducts , a decrease in their tone.
As a result of these negative phenomena, the process of bile outflow from the gallbladder into the duodenum is disrupted.
Normal outflow of bile promotes proper digestion, because bile is a digestive juice necessary for the breakdown of fats and the removal of toxic substances from the body. With JVP, this process is disrupted .
Possible consequences and complications
Biliary dyskinesia in children can lead to complications if it is not treated promptly.
The consequences of the disease include:
- formation of stones in the bile ducts;
- biliary pancreatitis;
- chronic cholecystitis;
- inflammation of the bile ducts;
- weight loss.
Biliary dyskinesia is a pathology that has a favorable prognosis. In children, the disease progresses in waves, with periods of exacerbations and improvements. Drug therapy and dieting alleviate the child’s condition, putting the disease into a state of prolonged remission.
Causes of development and risk groups
Negative factors as:
- Frequent stress that negatively affects the condition of the body as a whole.
- Dietary disorders, in particular, overeating, excessive consumption of fatty foods, insufficient amounts of foods containing fiber, coarse dietary fiber.
- Weakness of muscle tissue (VSD), sedentary lifestyle.
- Congenital malformations of the biliary system.
- Genetic predisposition.
- Infectious and other diseases of the gastrointestinal tract.
Based on the reasons stated above, we can conclude that school-age children .
A child entering 1st grade experiences stress associated with a sharp change in his usual daily routine.
In addition, modern schoolchildren do not always adhere to the principles of proper nutrition; they lead a sedentary lifestyle due to the need to intensively engage in educational activities; accordingly, the student has significantly less time for active games and walks.
Gallbladder problems in children: symptoms and treatment
— What nutritional recommendations are important for children with gallstone problems?
— First of all, an adequate drinking regime is necessary. Bile is 97% water. If a child drinks little and has problems with the gallbladder, it is important to correct this. If a child is from 3 to 7 years old, then he can drink about a liter and a half of liquid a day. This can be any harmless drink, but it should also include clean water. There are children who don't even drink a cup of water a day. Accordingly, the bile is thick and it will be difficult to come out. It is also important that the child does not starve, but does not overeat. For each meal, the gallbladder contracts, releasing certain substances that help start the process of bile secretion. Therefore, it is necessary that the child eats often, but does not constantly chew or bite something. The regimen should be clear - 3 main meals and 2 snacks.
— Can feeding against your appetite cause a problem with your gall bladder?
- Yes. This can create a stressful situation for the child and in response there will be a spasm of the gallbladder sphincter, and as a result, uneven secretion of bile. Food should be according to your appetite. If a child wants to eat, he will eat.
— What is the diet of a child who has a tendency to dyskinesia?
— Fatty foods, fried foods, smoked foods are excluded. Regular lard, by the way, is, on the contrary, useful, since the gall bladder needs fats to work well. But not overheated. Among vegetable fats, pumpkin oil is very good for the gastrointestinal tract. Food should not be very cold or hot. And, of course, no processed foods, fast foods or other junk food. By the way, ice cream is also not a very good product for the gastrointestinal tract, especially when it is given instead of food and not as a dessert. And for anyone at risk for gallbladder problems, it's wise to keep a food diary. When, what and how much the child ate, including water and snacks. And in this food diary you need to note the reactions that occurred. It is enough to keep these notes for a week before your visit to the doctor. Then you can understand what the negative answer is and remove the problem by simply adjusting your diet.
— Can herbal infusions help with problems with the gallbladder?
- Yes. And some are very helpful. The only question is what kind of herbs they are and to whom they will be prescribed. You cannot “prescribe” this to yourself. If you have a stone and have started taking a choleretic preparation? What if the problem is not with the gallbladder at all? Herbal remedies can be used, and they help a lot, but in no case as self-medication. There is a myth that herbs are safer than drugs. In fact, they also contain chemicals with different mechanisms of action, including possible toxicity. The same applies to nutritional supplements. After such incorrect “natural” treatment, toxic hepatitis in a child is not uncommon in the practice of a gastroenterologist. Therefore, herbal medicines are prescribed by a doctor who has experience in the use of herbal medicine and only after examination.
Classification of pathology
JVP can manifest itself as an independent disease (primary form), or as a secondary pathology that develops as a result of other diseases of the gastrointestinal tract.
Depending on the location of the disease, pathology of the gallbladder and its ducts, as well as disruption of the biliary sphincters, are distinguished.
Depending on the nature of the lesion and the clinical picture of the disease, JVP can be: hypertensive, hypotonic, combined (mixed).
Drug treatment of dyskinesia
- Choleretic drugs are necessary to remove bile accumulated in the bladder.
- Choleretics are drugs that stimulate the formation of bile.
- For hypotension, cholekinetics are prescribed - drugs that increase the tone of the gallbladder.
- It is recommended to carry out tubages according to Demyanov; this procedure helps eliminate stagnation of bile and cleanse the bladder and its ducts.
- With intense pain in the right hypochondrium, antispasmodics help.
- The child is also recommended to take a course of mineral water and resort treatment.
JVP is largely due to the state of the child’s nervous system and is often provoked by stress, criticism from parents or their quarrels. Therefore, it is important to include a psychological aspect in complex therapy. It is recommended to create a favorable microclimate at home for the child. Massages, relaxing baths, visits to the pool, individual and group sessions with a psychologist are also effective.
Author: Olesya Butuzova, pediatrician
The material used photographs belonging to shutterstock.com
Clinical symptoms
Manifestations of pathology can be different, depending on its form.
| Form | Clinical manifestations |
| Hypertensive |
|
| Hypotonic |
|
| Combined |
|
An infant, due to his limited capabilities, cannot tell his parents about what is bothering him . At the same time, unpleasant sensations cause him significant discomfort and anxiety.
Parents should pay attention to changes in the child’s condition and behavior. In particular, during painful attacks, the baby presses his legs to his stomach, this helps reduce pain.
In addition, the baby does not gain weight well, often refuses to eat, cries, and sleeps poorly.
Functional disorders of the biliary system in children
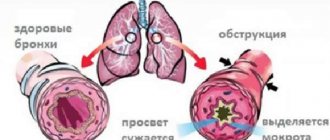
Biliary dyskinesia is a classic representative of functional disorders (diseases) of the gastrointestinal tract. The modern definition, according to DA Drossman, is that “functional impairment is a varied combination of gastrointestinal symptoms without structural or biochemical abnormalities.” Functional diseases include conditions in which it is not possible to detect morphological, genetic, metabolic and other changes in organs. Functional pathological syndromes arise as a result of violations of the mechanisms regulating the functions of a particular organ or system. Disorder of the motor-tonic function of the biliary tract - or dyskinesia of the biliary system - is one of the most common diseases in childhood. Violation of the outflow of bile or its irregular flow into the intestinal lumen affects not only the functioning of the digestive tract, but also the entire organism as a whole, since bile, being a multicomponent biochemical substrate, provides a number of functional processes. These include the following: neutralization of hydrochloric acid and pepsin, emulsification of fats and thereby participation in their hydrolysis, activation of intestinal and pancreatic enzymes, enhanced absorption of fat-soluble vitamins A, D, K, E, fixation of enzymes on villi, support of peristalsis and intestinal tone, antibacterial and antiprotozoal action; metabolites of xenobiotics, medicinal and toxic substances are excreted into the intestinal lumen with bile.
The structure of the biliary system consists of the right and left hepatic ducts, the common hepatic duct, the gallbladder (GB), the cystic duct, and the common bile duct. The common bile duct opens into the duodenum along with the main pancreatic duct through the large duodenal (Vater) nipple protruding into its lumen, in the thickness of which there is a true anatomical sphincter - the sphincter of Oddi, which regulates the flow of bile and pancreatic secretions into the intestine. The sphincter of Oddi consists of the sphincter of the major duodenal papilla, the sphincter of the common bile duct and the sphincter of the pancreatic duct. In rare cases, these sphincters open separately into the lumen of the duodenum. In addition to the anatomical one, there are two functional sphincters in the biliary system - the sphincter of Miritsi (at the confluence of the right and left hepatic ducts) and Lütkens (at the junction of the neck of the gallbladder into the cystic duct). The main task of the sphincter apparatus is to regulate the flow of bile into the intestine and prevent reflux. The biliary system has a layered structure common to the entire gastrointestinal tract, including the mucous and submucosal membranes, a muscular layer of longitudinal and circular fibers and a loose outer connective tissue membrane in which vessels and nerves are located. In addition to ensuring the passage of bile, the biliary tract takes part in the formation of the final composition of bile, since the mucous membrane is responsible for the processes of absorption and secretion of water, chlorides, bicarbonates, etc.
Regulation of the biliary system is coordinated and controlled by the autonomic nervous system (plexus hepaticus, sympathetic and parasympathetic divisions) and neurohumoral factors (cholecystokinin, gastrin, secretin), among which cholecystokinin has the most significant influence. Moderate irritation of the vagus nerve causes coordinated activity of the gallbladder and sphincters, severe irritation causes its spastic contraction. Increasing the tone of the sympathetic link - relaxing the sphincters and reducing the tone of the gallbladder. Looking ahead, it should be noted that the majority of older children, especially with diseases of the upper gastrointestinal tract, are parasympathotonics, which a priori causes a hypertensive type of dysfunction of the biliary system. Normally, the sphincter of Oddi periodically opens and during the interdigestive period, bile flows evenly into the lumen of the duodenum at a rate of 4–5 drops per minute. The most powerful stimulator of gallbladder contraction is food intake. The entry of bile into the duodenum coincides with the time of passage of the peristaltic wave through the pylorus. When food enters the duodenum, a regulatory peptide, cholecystokinin, is produced, which regulates further contraction of the gallbladder. The time of tonic contraction of the gastrointestinal tract depends on the volume and quality of the food taken - with a large meal, especially fatty food, the contraction of the gastrointestinal tract lasts until the stomach is completely emptied. When eating a small amount of food, especially with a low fat content, the reduction in gallbladder is short-term. This pattern of GB reduction must be taken into account when constructing functional tests and only adequate choleretic breakfasts should be used. Of the nutrients, egg yolks cause the maximum reduction in GB - up to 80%. After contraction, the tone of the gallbladder decreases and a period of filling it with bile begins.
Reasons for the development of functional disorders of the biliary tract . The causes of functional disorders are usually associated with a dysregulation of the organ whose function is impaired. These changes in nervous regulation are usually provoked by psycho-emotional and stress factors and are caused by autonomic disorders or organic damage to the central nervous system with the subsequent development of autonomic dysfunction. In children of the first year of life, functional disorders of the gastrointestinal tract are most often a manifestation of perinatal lesions of the central nervous system in the structure of vegetative-visceral syndrome or natal trauma to the spinal parts of the nervous system. At older ages, the role of reflex and neurohumoral disorders in the development of chronic diseases of the gastrointestinal tract increases. The development of motor-tonic disorders of the biliary tract is caused by autonomic disorders, neuroses, psycho-emotional disorders, food allergies, parasitosis and chronic diseases of the digestive system, eating disorders, physical inactivity, smoking, alcohol and much more.
Terminology and classification . In Russian medical literature, the term “biliary dyskinesia” (BDSD) is widely used and familiar. In foreign medical practice, it corresponds to the concept of “dysfunctional disorders of the biliary tract.” There are many definitions of JVP. The most complete definition of dyskinetic disorders of the biliary tract can be considered the definition proposed by domestic gastroenterologists Academician A.L. Grebenev and Professor A.A. Sheptulin in 1997: “DZHVP is a disorder of the motor-tonic function of the biliary system, which is based on uncoordinated (excessive or insufficient) contraction of the gallbladder, sphincters of Oddi, Lütkens, Miritsi, due to disruption of the interaction of the innervation and paracrine systems, coordinating the sequence of their contraction and relaxation.” ICD 10 distinguishes two forms - dyskinesia of the gallbladder and cystic duct (K 82.8) and spasm of the sphincter of Oddi (K 83.4). According to the Rome Consensus III (Los Angeles, 2006), the following forms of dyskinetic disorders are distinguished: E1 - functional disorders of the gastrointestinal tract, E2 - functional biliary disorder of the sphincter of Oddi, E3 - functional pancreatic disorder of the sphincter of Oddi. Disturbance of synchronicity in the work of the gastrointestinal tract and the sphincter apparatus is the cause of the formation of clinical symptoms.
Clinical manifestations . For patients with ADHD, typical complaints are stabbing pain in the right side or hypochondrium after fatty, fried foods or during physical or emotional stress. Such symptoms are caused by a spastic state of the sphincter of Oddi or excessive contractions of the muscular layer of the gallbladder. When the gallbladder is overstretched (with hypotension or impaired bile outflow due to severe spasm of the sphincters), complaints of a feeling of heaviness and/or fullness in the right side or hypochondrium appear. If you eat fatty or fried foods, you may experience nausea or vomiting.
During an objective examination, one can note pain on palpation in the right hypochondrium, positive cystic symptoms, including a positive frenicus symptom on the right.
Diagnostics. From studies of the clinical minimum, only in the coprogram can signs of impaired bile secretion be noted - neutral fat, fatty acids, soaps. In the biochemical spectrum of blood, an increase in the level of alkaline phosphatase can be noted. According to the Rome Consensus criteria, pancreatic dysfunction of the sphincter of Oddi is characterized by increased levels of lipase and amylase in the blood. Duodenal intubation is rarely used in clinical practice today. The most common and accessible method for studying the condition of the biliary tract is ultrasound diagnostics. Ultrasound examination of the gallbladder is performed on an empty stomach. Normally, the gallbladder has a round, oval or pear-shaped shape. The thickness of the wall of the gallbladder can normally vary from 0 to 4 mm; when describing the wall, the uniformity of its structure is important. The lumen of the bladder is echo-negative. The size of the gallbladder is variable and depends little on age. In our observations, the length of the gallbladder was 7 cm in a newborn and 4 cm in an adolescent. The average length of the gallbladder during ultrasound examination is 5–7 cm, width 1.2–2.5 cm. It must be remembered that the ultrasound dimensions of the bladder do not correspond to its true anatomical dimensions and is categorically incorrect based only on an increase in the ultrasound dimensions without performing a functional research to establish a diagnosis of hypomotor dysfunction of the gallbladder!
A common finding with GIB on ultrasound is the location of thick, heterogeneous bile in the lumen of the GB, which indicates its stagnant changes.
Since the introduction of ultrasound examination into clinical practice, the detection of anomalies in the shape of the gallbladder (kinks) has sharply increased.
It must be remembered that most of the identified kinks are functional (when examined in a standing position, they straighten out) and are associated with the intensive growth of the gallbladder and the small capacity of its bed. As the child grows, such kinks can appear and disappear repeatedly and sometimes take on the most bizarre forms. It is a mistake to make a diagnosis of bile ducts only on the basis of identifying functional kinks, since they rarely impede bile flow, although they can be attributed to predisposing factors.
A functional study of the contractility of the gallbladder (echocholecystography) is best carried out using the method proposed at the Research Institute of Pediatrics in 1987. According to this technique, the size of the gallbladder is taken on an empty stomach and every 15 minutes after taking a choleretic breakfast for 90 minutes. The optimal breakfast is raw yolks or xylitol (5 g/20 kg of weight). The use of other breakfasts (bread and butter, yogurt, sour cream, cheese, chocolate) causes either a weak or delayed contraction of the gallbladder, which leads to an erroneous diagnosis of hypomotor dyskinesia. With normal contraction of the gallbladder, its volume is reduced by approximately 50% 30–60 minutes after taking a choleretic breakfast, then its recovery is noted. Control determination of the size of the gallbladder only an hour after the start of the study (without intermediate measurements) again leads to an erroneous diagnosis of hypomotor dysfunction due to the fact that after 1 hour in many children the volume is restored (
), and the researchers conclude that the motor function of the gallbladder is reduced.
In children with symptoms of GIB on the background of a chronic disease of the gastrointestinal tract, a normokinetic or hyperkinetic variant of GB contraction is more often observed ().
We conducted a study of the contractile function of the gallbladder in children with neurological abnormalities (consequences of perinatal lesions of the central nervous system). The results of the study of the contractile function of the gallbladder in children with consequences of perinatal lesions of the central nervous system revealed such an individual and chaotic kinetic profile of contraction that in these patients it was impossible to talk about normo- or hyperkinesis of the gallbladder, and therefore it was not possible to draw a conclusion about the type of dysfunction. That is why it is more correct in these cases to talk about an uncoordinated contraction of the gallbladder, which in turn is caused by dysfunction of the autonomic nervous system against the background of the consequences of perinatal lesions of the central nervous system. It should immediately be noted that the total reduction in the volume of the gallbladder was 50–95%, which excludes the hypotonic variant of dysfunction.
Other research methods, such as retrograde cholangiopancreatography and biliary tract scintigraphy, are rarely used in domestic medical practice.
Treatment of functional disorders of the biliary system . First of all, when treating any disease, it is necessary to pay attention to optimizing lifestyle and neutralizing the effects of predisposing and damaging factors. Thus, it is recommended to normalize the duration of night sleep, since it is during sleep that regulatory processes on the part of the central nervous system are restored. The physiological duration of night sleep in adolescence is 8 hours a day, in younger schoolchildren it is 9–10 hours. In case of severe asthenic syndrome, additional daytime sleep is recommended. Sufficient daily physical activity and walking are a preventive and therapeutic component in the management of patients with ADHD. Electromagnetic radiation has a significant damaging effect on the central nervous and autonomic systems, and therefore it is necessary to limit the time watching TV shows and working at the computer to 2–3 hours a day. As for the nutritional factor, in case of pathology of the biliary system, diet No. 5 is recommended. Since the very fact of eating is a good stimulator for the flow of bile into the duodenum, meals should be regular, not plentiful, 4-5 times a day. Mechanical and chemical sparing is recommended; food is steamed or boiled. Recommended: vegetable and fruit salads, vinaigrettes, soft-boiled eggs, cheese, cottage cheese, boiled or baked meat and fish, vegetarian soups, dairy and fermented milk products, juices. It is allowed to add vegetable oils to salads in small quantities at each meal. Dishes with a high content of extractive substances (strong meat, fish, mushroom broths, spices, marinades, smoked meats) are excluded, and refractory fats - lard, pork - are limited. Carbonated drinks and cold drinks and dishes are excluded (they contribute to spasm of the bile ducts).
Drug therapy . Drug treatment for dysfunctional diseases of the biliary tract depends on the form of dysfunction and the nature of the underlying disease and must be comprehensive. Considering the large role of disorders of the autonomic and central nervous systems in the development of biliary disorders, it is necessary to use means aimed at restoring impaired regulation; treatment of diseases against which the dyskinetic process has developed is carried out.
In the hypertensive form of dysfunction, antispasmodics are prescribed to relieve pain: No-shpa, Papaverine hydrochloride, Dibazol, etc. The drugs are prescribed in age-specific doses, in a short course of 3–5 days, since they all have a systemic antispasmodic effect. The peripheral antispasmodic mebeverine (Duspatalin) is widely used in clinical practice today. Duspatalin is prescribed 20 minutes before meals, 1 capsule 2 times a day, and can be used long-term (approved for use in children over 12 years of age). After pain relief, further therapy is selected. As a rule, modern drugs used to correct biliary tract dysfunction have a combined effect: mild antispasmodic, choleretic and cholekinetic, hepatoprotective, which makes it possible to individualize the therapy. Below are characteristics of some recommended drugs.
Olimethine. Herbal preparation (oil of calamus, mint, olive, turpentine, sulfur), release form - capsules. It has antispasmodic, choleretic, anti-inflammatory, diuretic effects. Take 1-2 capsules daily before meals.
Holasas. Condensed aqueous extract of rose hips. Release form: syrup. Has a choleretic effect. Prescribed 1/2–1 teaspoon before meals.
Holagol. A combined drug (turmeric, buckthorn, olive oil, magnesium salicylate) has anti-inflammatory and choleretic effects. Release form: drops. Apply 1-5 drops per piece of sugar or bread 30 minutes before meals.
Gepabene. The combined drug (fumitive, milk thistle) has choleretic, cholekinetic and hepatoprotective effects. Release form: capsules (approved for use in children over 6 years of age). Take 1-2 capsules with meals.
Odeston. The active ingredient is hymecromone. It has a peripheral selective antispasmodic and choleretic effect. Release form: tablets. Taken 30 minutes before meals.
LIV-52. A complex preparation of plant origin (prickly capers, chicory, black nightshade, senna, terminalia, yarrow, Tamarix galii), has a wide spectrum of activity, providing anti-inflammatory, choleretic, hepatoprotective and antispasmodic effects. Release form: drops and tablets. Approved for use in children from 2 years of age. Prescribed 10–15 minutes before meals.
Hofitol. A preparation based on field artichoke. Has a systemic complex effect; hepatoprotector of plant origin, increases the outflow of bile, reduces intrahepatic cholestasis, has a mild diuretic effect, reduces the content of nitrogenous substances in the blood, exhibits antioxidant activity, improves the antitoxic function of the liver, in addition, reduces the synthesis of cholesterol by hepatocytes, normalizes intracellular phospholipid metabolism, reduces atherogenic cholesterol fractions , normalizes lipid profile parameters. Approved for use in children from the first days of life. It has the following forms of release: solution (with low volume alcohol content), tablets and solution for injection in ampoules. Taken before meals.
Galstena. Complex homeopathic medicine (milk thistle, dandelion, celandine, Na sulfate, phosphorus). It has anti-inflammatory choleretic and hepatoprotective effects. Release form: drops. Approved for use in young children. Prescribed 30 minutes before meals.
Hepel. Complex homeopathic medicine. It has anti-inflammatory, choleretic and hepatoprotective effects, normalizes the processes of autonomic regulation of the biliary system. Release form: tablets. Prescribed sublingually 30 minutes before meals.
It should be noted that the market of drugs, including choleretic drugs, is replenished every year. As mentioned earlier, to optimize treatment it is necessary to take into account the spectrum of action of the drug and the characteristics of the course of the disease in the patient. If bile thickening syndrome, metabolic disorders are detected, or crystalline changes in the structure of bile are detected (according to ultrasound), it is necessary to choose a drug that has a hepatoprotective effect, or prescribe separate courses of hepatoprotective therapy. The average course of drug treatment for biliary dysfunction is 2–3 weeks. Then, to consolidate the effect, herbal medicine can be recommended. The choice of herbs that have a choleretic effect is quite wide: calamus, artichoke, common barberry, sandy immortelle, dandelion, peppermint, cudweed, corn silk, sage, etc. The average course of herbal medicine is 1 month, you can use medicinal herbal tea Tubages have a good drainage effect; it should be noted that tubages are prescribed only after the spastic state of the sphincters has been relieved, respectively, at the second or third stage of treatment. Tubage technique (according to Demyanov): in the morning on an empty stomach the patient is given a “choleretic breakfast” to drink, which can be 15–20 ml of a 33% warm solution of magnesium sulfate, or 2 egg yolks, or warm olive (corn oil), or 100–200 ml 10% solution of sorbitol, xylitol, warm mineral water (3 ml/kg body weight); then you need to lay him on his right side on a warm heating pad for 1.5–2 hours, during the procedure to open the sphincter of Oddi, take 2–3 deep breaths every 5 minutes. It is recommended to carry out 1–2 procedures per week, a course of 8–10 procedures.
Physiotherapy . Methods are used aimed at normalizing the activity of the central nervous system and autonomic nervous system; photochromotherapy or electrophoresis with Ca and Br according to Shcherbak on the collar zone, transair, EHF puncture on the projection area of the 7th cervical vertebra. Locally - electrophoresis with a 5% solution of magnesium sulfate, paraffin or ozokerite applications, inductothermy to the right hypochondrium, course of 8-10 procedures.
Clinical examination. The nature and volume of dispensary activities carried out are determined by the structure of the existing pathology.
V. A. Aleksandrova , Doctor of Medical Sciences, Professor S. V. Rychkova , Candidate of Medical Sciences, Associate Professor of St. Petersburg MAPO , St. Petersburg
How dangerous is the disease?
Untreated gallstones can lead to chronic inflammatory diseases in the body (cholangitis, chronic cholecystitis), the appearance of a focus of inflammation in the gallbladder itself, the formation of stones, and the development of other pathologies of the digestive system (for example, gastritis).
In addition, with ADHD, metabolic processes in the body are disrupted, which negatively affects the development of the child and the functioning of all organs and tissues of his body.
What diet should you follow for gastroduodenitis in children? Find out about this from our article.
Hypotonic biliary dyskinesia in children
Schoolchildren with an asthenic physique are more often susceptible to hypotonic type VA. And the reason for this, first of all, is poor nutrition, a frivolous attitude to the daily routine, as well as psycho-emotional stress. As a result, the motility of internal organs and the consistency of their work are disrupted. With hypotonic dyskinesia, the gallbladder is in a relaxed state. What prevents it from pushing out bile and delivering it portionwise to the duodenum. The digestion process is disrupted. There is also a high risk of bile stagnation in the gallbladder – cholestasis.
Hypotonic JVP in its pure form is quite rare. More often there is a mixed type of JVP.
Since in the human body muscle spasm is periodically replaced by relaxation of smooth muscles, the state of the gallbladder and ducts can also change: move from complete relaxation to increased tone and vice versa.
JVP of the hypotonic type: causes
The causes of gallbladder motility disorders can be primary and secondary. Primary causes - congenital malformations of the gallbladder (duct, (and) or sphincters) - are quite rare. In one case out of ten. But there are quite a few secondary reasons. Starting, of course, with poor nutrition and ending with various viral and intestinal infections.
But most often dyskinesia in children develops as a consequence of chronic diseases of the digestive system. And to carry out adequate treatment, it will not be enough to diagnose ADHD; you need to find and eliminate the cause of its occurrence. For this purpose, a number of studies are carried out, including a general blood test, bile analysis for the presence of parasitic infections, ultrasound, and also FGDS (fibrogastroduodenoscopy).
Diagnostics
Diagnosis of pathology is carried out in several stages. To begin with, the doctor collects an anamnesis of the disease and evaluates the totality of its manifestations. At the next stage, the necessary laboratory tests are carried out:
- blood test (general, biochemical, for the presence of antibodies to viral hepatitis, for lipid content);
- clinical urine analysis;
- stool analysis for worm eggs.
Further, hardware diagnostic methods may be required, in particular, ultrasound of the abdominal organs, ultrasound of the gallbladder and its ducts, and x-ray of the gallbladder.
Treatment methods
How to treat a child? Treatment of ADHD is carried out using specially designed medications, in combination with adherence to a therapeutic diet .
The following groups of drugs are prescribed as drug therapy:
- Prokinetics (Domperidone) are necessary to normalize the motility of the biliary system.
- Choleretics (Allohol) help normalize the process of bile formation.
- Cholekinetics (Magnesium Sulfate) improve the process of bile discharge.
- Enzyme preparations (Mezim) improve digestion.
- Hepatoprotectors (Essentiale) help normalize liver function and restore its functionality.
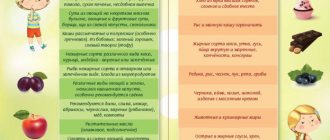
Diet
In addition to taking medications, the child must follow a specially designed diet.
There is a list of products prohibited for consumption. It includes:
- fatty, spicy, fried foods;
- pickles, smoked meats, canned food;
- fresh bakery;
- vegetables with a strong taste (garlic, radishes);
- meat broths;
- sparkling water;
- snacks in the form of chips and other unhealthy foods;
- legumes;
- nuts;
- strong teas, coffee, cocoa.
The basis of a child’s diet should be the following products:
- soups cooked in water;
- milk porridge;
- rye bread (dried);
- lean meat;
- crackers (low fat);
- cheese (low-fat varieties);
- fruits (if there are no allergies);
- herbal teas, compotes, fruit juices diluted with water (1:1 ratio).
Among sweets, it is allowed to consume marshmallows, marshmallows, marmalade candies, jam, honey (in small quantities for older children).
Dr. Komarovsky about JVP
E. O. Komarovsky believes that the symptoms of ADHD are not characteristic of this particular pathology, and may indicate the presence of completely different problems that require, accordingly, different treatment.
Self-prescribing medications to a child can only worsen the situation, because without making a diagnosis, establishing the cause and characteristics of the pathology, it is absolutely impossible to prescribe treatment.
If signs of digestive system dysfunction are detected, the following recommendations must be followed:
- It is recommended to place the child on the right side immediately after eating, so the painful sensations will be less pronounced.
- If your baby refuses to eat, there is no need to force him.
- If problems arise in the functioning of the digestive organs, it is necessary to postpone the introduction of complementary foods.
- The child must be seen by a doctor as soon as possible.
Recommendations from pediatricians for the treatment of dysbiosis in children can be found on our website.