Ultrasonography
The main indications for additional studies are slowed or increased dynamics of AMD growth.
Unfavorable symptoms detected during uterine measurement suggest selective ultrasound. It is carried out for medical reasons in case of an unfavorable course of pregnancy. Measuring the expectant mother’s abdomen with a “centimeter” is a mandatory measure at every visit to the obstetrician and allows one to suspect a possible pathology during pregnancy. A reliable method to resolve the doctor’s doubts and determine any abnormalities during the gestation period is ultrasound. Using ultrasound you can find out:
- the most accurate gestational age;
- fetal height and weight;
- determine whether the embryo/fetus is alive or dead;
- localization of the placenta;
- size and thickness of the placenta;
- whether the pregnancy develops in a short period of time (exclude frozen one);
- identify trophoblastic disease;
- exclude ectopic pregnancy;
- determine the position/presentation of the unborn baby;
- diagnose fetoplacental insufficiency.
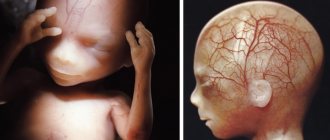
What is ventriculomegaly and what types of it occurs?
Ventriculomegaly can be isolated asymmetric (expansion of one ventricle or its horns without changes in the brain parenchyma), symmetric (observed in both hemispheres) or diagnosed in combination with other pathologies of fetal development. Ventricular pathology is divided into three types:
- mild - organ dilatation is 10.1–12 mm, usually detected at 20 weeks and needs to be monitored before birth;
- moderate – the size of the ventricles reaches 12–15 mm, which impairs the outflow of cerebrospinal fluid;
- pronounced - ultrasound readings exceed 15 mm, which disrupts brain function and negatively affects the vital functions of the fetus.
If the lateral ventricles are enlarged to 10.1–15 mm (deviation from the table standards by 1–5 mm), borderline ventriculomegaly is diagnosed. It may be asymptomatic up to a certain point, but in fact it indicates the emergence of a complex pathological process that gradually changes the functioning of many important organs.
Is an enlarged yolk sac dangerous?
Since this structure is so important, it is only natural that it is examined during an ultrasound examination. You can see it starting from the sixth week from conception. The yolk sac can no longer be examined using ultrasound.
At weeks 5-10, the size of the sac should not exceed 5.5 millimeters. But in women, the size of this formation is usually about 2 mm.
But sometimes the doctor notices that the yolk sac is enlarged. What does this mean and how dangerous is it? In fact, any deviation from the norm may indicate a threat to pregnancy. Naturally, this is not a final diagnosis, since other, additional studies are needed. For example, an enlarged yolk sac may be related to diet, certain medications, or severe stress. In any case, with similar ultrasound results, you need to go to a gynecologist. Only a specialist knows why the yolk sac may be enlarged, what it means and whether special treatment is required.
Reasons for reducing CTE
Non-developing pregnancy
This pathology is confirmed by the absence of movement and heartbeat in the fetus. However, this can only be assessed in an embryo if the CTE exceeds 6 mm. If the coccygeal-parietal size is more than 6 mm and the heartbeat is not detected, then, depending on the situation, either a repeat ultrasound scan after 5-7 days or emergency surgery is recommended.
Late fertilization due to later ovulation
This is possible, for example, if pregnancy occurs in a short time after stopping hormonal contraceptives. To confirm this reason, it is necessary to conduct a control ultrasound after 10-14 days to determine the CTE to more accurately determine the gestational age.
Maternal hormonal imbalance
More often this is caused by progesterone deficiency. In the absence of adequate prescription of replacement therapy, early pregnancy termination is possible. For diagnosis, laboratory methods are used to determine hormone levels.
Infectious diseases in the mother
This is especially true for infections of the urogenital tract (chlamydial, mycoplasma infections). In this regard, it is necessary to conduct examinations for sexually transmitted infections in pregnant women, as well as carry out the necessary antibacterial therapy within the acceptable time frame.
Genetic diseases
For example, Down syndrome, Shereshevsky-Turner, Patau. If this pathology is suspected, it is necessary to conduct a biochemical examination of pregnant women. If changes are detected in the results of ultrasound and biochemical tests, amniocentesis (sampling of amniotic fluid during puncture for further research) or cordocentesis (sampling of umbilical cord blood) is recommended. However, due to the invasiveness of the method, the consent of the pregnant woman to conduct this study is required.
Pathology of the uterus
In particular, uterine fibroids, changes as a result of previous abortions and miscarriages. This reason is indicated by anamnesis and previous ultrasound data.
Development of multiple pregnancy. With such a pathology, it is also possible that the obtained CTE values do not correspond to the data from the table, but this is not a pathology.
The scope of examination required to detect a deviation of the CTE from the norm is individual in each case and is determined not only by ultrasound data, but also by anamnesis and clinical data.
Determination of hormonal levels, examination for the presence of sexually transmitted infections, exclusion of chromosomal diseases. While the examination is being carried out, it is necessary to carry out an ultrasound examination in dynamics, but it is not advisable to conduct it more often than after 5 days.
In addition to determining the coccygeal-parietal size, during a screening ultrasound examination, other important indicators are determined:
- The presence of heartbeats and their frequency.
- The thickness of the nuchal translucency (as an indirect marker of Down syndrome, is assessed up to 13 weeks).
- Yolk sac, its presence, thickness (determined before 12 weeks, important in diagnosing a non-developing pregnancy).
- Chorion, its location and structure (information about the location of the placenta in the future, the presence of intrauterine infection and Rh conflict).
The norms of all these indicators also depend on the period and have established tabular values.
Pathology of the yolk sac
When performing an ultrasound, the doctor can detect the following conditions:
The yolk sac is not visualized
Normally, the yolk sac is detected by ultrasound in the period from 6 to 12 weeks. The absence of a yolk sac is an unfavorable sign. If such an important organ is resorbed ahead of time for some reason, the embryo ceases to receive the substances necessary for its development. The synthesis of hormones and enzymes is disrupted, and the production of red blood cells stops. With premature reduction of the yolk sac (before 12 weeks), spontaneous miscarriage occurs. It is not possible to maintain pregnancy with medications.
The absence of a yolk sac on ultrasound (from 6 to 12 weeks) is considered one of the signs of a regressing pregnancy. In this case, the heartbeat of the embryo is not determined, its size does not correspond to the gestational age. Treatment is only surgical. In case of regressing pregnancy, the fertilized egg is removed and the uterine cavity is curetted.
The yolk sac is smaller than normal
- The yolk sac is defined as a rudimentary formation.
- The size of the yolk sac does not correspond to the duration of pregnancy (smaller than normal).
Any of these situations indicates that premature resorption of the yolk sac has begun. If at the time of reduction of the sac the internal organs of the fetus are not yet formed and are not able to fully function, the death of the embryo and spontaneous miscarriage occurs. In some cases, contractions of the uterus and miscarriage do not occur after the death of the embryo. This condition is called regressive pregnancy.
The yolk sac is larger than normal
The main reason for this symptom is incorrect determination of the gestational age. This is possible with an irregular menstrual cycle (against the background of various gynecological pathologies or in nursing mothers). In this situation, the doctor should evaluate the size of the embryo and recalculate the gestational age taking into account the available data.
An important point: changes in the size, shape or density of the yolk sac are important only in combination with other ultrasound indicators. If any abnormalities are detected, the condition of the embryo (location, size, heartbeat) should be assessed. If the baby is growing and developing in accordance with the gestational age, there is no reason to worry. Changes in the yolk sac in this case are considered an individual feature that does not affect the course of the first trimester.
Sources:
https://vseprorebenka.ru/beremennost/plod/zheltochnyj-meshok-norma-po-nedelyam.html https://www.baby.ru/blogs/post/247928541-180965938/ https://spuzom.com/zheltochnyj -meshok-pri-premennosti.html
Table of the dependence of the coccygeal-parietal size of the fetus on gestational age
| KTE, mm | Gestation period, week + day | KTE, mm | Gestation period, week + day | KTE, mm | Gestation period, week + day |
| 3 | 4 | 26 | 9 + 6 | 61 | 13 + 1 |
| 4 | 5 + 2 | 27 | 10 | 62 | 13 + 2 |
| 5 | 6 + 1 | 28 | 10 + 1 | 63 | 13 + 2 |
| 6 | 6 + 3 | 30 | 10 + 2 | 64 | 13 + 3 |
| 7 | 6 + 5 | 31 | 10 + 3 | 65 | 13 + 3 |
| 8 | 6 + 6 | 32 | 10 + 4 | 66 | 13 + 4 |
| 9 | 7 | 33 | 10 + 5 | 67 | 13 + 4 |
| 10 | 7 + 2 | 34 | 10 + 6 | 68 | 13 + 5 |
| 11 | 7 + 3 | 36 | 11 | 69 | 13 + 5 |
| 12 | 7 + 5 | 38 | 11 + 1 | 70 | 13 + 5 |
| 13 | 7 + 6 | 39 | 11 + 2 | 71 | 13 + 6 |
| 14 | 8 + 1 | 41 | 11 + 3 | 72 | 13 + 6 |
| 15 | 8 + 2 | 42 | 11 + 4 | 73 | 14 |
| 16 | 8 + 3 | 44 | 11 + 5 | 74 | 14 |
| 17 | 8 + 4 | 46 | 11 + 6 | 75 | 14 + 1 |
| 18 | 8 + 5 | 47 | 12 | 76 | 14 + 1 |
| 19 | 8 + 6 | 49 | 12 + 1 | 77 | 14 + 2 |
| 20 | 9 | 50 | 12 + 2 | 78 | 14 + 3 |
| 21 | 9 + 1 | 51 | 12 + 3 | 80 | 14 + 3 |
| 22 | 9 + 2 | 53 | 12 + 4 | 82 | 14 + 4 |
| 23 | 9 + 3 | 55 | 12 + 5 | 84 | 14 + 5 |
| 24 | 9 + 4 | 58 | 12 + 6 | 87 | 14 + 6 |
| 25 | 9 + 5 | 59 | 13 | 88 | 15 |
| KTE, mm | Gestation period, week + day |
| 3 | 4 |
| 4 | 5 + 2 |
| 5 | 6 + 1 |
| 6 | 6 + 3 |
| 7 | 6 + 5 |
| 8 | 6 + 6 |
| 9 | 7 |
| 10 | 7 + 2 |
| 11 | 7 + 3 |
| 12 | 7 + 5 |
| 13 | 7 + 6 |
| 14 | 8 + 1 |
| 15 | 8 + 2 |
| 16 | 8 + 3 |
| 17 | 8 + 4 |
| 18 | 8 + 5 |
| 19 | 8 + 6 |
| 20 | 9 |
| 21 | 9 + 1 |
| 22 | 9 + 2 |
| 23 | 9 + 3 |
| 24 | 9 + 4 |
| 25 | 9 + 5 |
| KTE, mm | Gestation period, week + day |
| 26 | 9 + 6 |
| 27 | 10 |
| 28 | 10 + 1 |
| 30 | 10 + 2 |
| 31 | 10 + 3 |
| 32 | 10 + 4 |
| 33 | 10 + 5 |
| 34 | 10 + 6 |
| 36 | 11 |
| 38 | 11 + 1 |
| 39 | 11 + 2 |
| 41 | 11 + 3 |
| 42 | 11 + 4 |
| 44 | 11 + 5 |
| 46 | 11 + 6 |
| 47 | 12 |
| 49 | 12 + 1 |
| 50 | 12 + 2 |
| 51 | 12 + 3 |
| 53 | 12 + 4 |
| 55 | 12 + 5 |
| 58 | 12 + 6 |
| 59 | 13 |
| KTE, mm | Gestation period, week + day |
| 61 | 13 + 1 |
| 62 | 13 + 2 |
| 63 | 13 + 2 |
| 64 | 13 + 3 |
| 65 | 13 + 3 |
| 66 | 13 + 4 |
| 67 | 13 + 4 |
| 68 | 13 + 5 |
| 69 | 13 + 5 |
| 70 | 13 + 5 |
| 71 | 13 + 6 |
| 72 | 13 + 6 |
| 73 | 14 |
| 74 | 14 |
| 75 | 14 + 1 |
| 76 | 14 + 1 |
| 77 | 14 + 2 |
| 78 | 14 + 3 |
| 80 | 14 + 3 |
| 82 | 14 + 4 |
| 84 | 14 + 5 |
| 87 | 14 + 6 |
| 88 | 15 |
The coccygeal-parietal size of the fetus practically does not depend on the individual characteristics of the pregnant woman (gender, age, nationality). If, when determining this indicator, fluctuations are detected that significantly exceed the norm (more than one week or more than 7-10 mm), this may be a sign of a pathological course of pregnancy.
Thus, an increase in CTE may be caused by a Rh conflict between the mother and the embryo, subcompensated by diabetes mellitus in the pregnant woman. Enlargement is also an early sign of the development of a large fetus. This criterion helps to further adjust the tactics of managing such a pregnancy: limiting the unnecessary use of metabolic drugs and multivitamin complexes.
Development and structure
The growth of the fertilized egg begins from the moment of conception. The fertilized egg begins to move through the fallopian tube, during which cell fragmentation occurs. Making its way to the uterus, the fertilized, crushed egg needs nutrients and oxygen, so after a week a chorion begins to form on top, which subsequently transforms into the placenta.
The surface of the chorion has villi, which help the formation to attach to the uterus. In the future, these villi are contained only at the site of implantation of the formation into the uterine wall. The rest of the structure loses lint and remains smooth. The chorion provides the fetus with all vital functions, one of which is protection against infections.
Twenty days after menstruation, during a hardware examination, you can see the yolk sac, which is designed to provide the fetus with nutrients. The presence of a yolk sac in the fertilized egg does not guarantee a normal pregnancy, but if it is absent, this indicates pathology. Inside the shell, surrounding
The embryo contains the amnion, a hollow sac that produces the optimal environment and amniotic fluid for the development of the child.
Often, during an examination, an ultrasound specialist may detect a second fertilized sac. In this case, the woman can be congratulated, as she will have twins. Such a pregnancy develops when two eggs are simultaneously fertilized or two zygotes develop from the same egg.
If a woman is expecting twins, the fertilized egg may form one or two placentas at the time of division.
If the moment of attachment of the egg to the uterus occurs after 8-13 days from the day of fertilization, then 2 fetuses and one placenta are formed for two. This means that both fetuses will develop in the same amniotic sac. If division occurs earlier than this period, then each embryo will develop in its own fertilized egg.
Human organ
After the embryo attaches to the walls of the uterus, its very rapid development begins. The growth of an embryo is a true miracle of nature. After birth, no creature is capable of developing as quickly as an embryo in the mother's womb.
Within a few weeks after conception, an endoblastic vesicle gradually forms at the site of the fused sperm and egg. He becomes a kind of “prototype” of the future human being. After a few more weeks, the yolk sac begins to form from the endoblastic vesicle. It will not last long - its “life” takes no more than three months, but without it the fetus will not be able to form normally.
The yolk sac is classified as a so-called provisional organ. They exist only temporarily. Their function is to replace for the embryo those organs that an adult has, but has not yet formed in the embryo. In addition to the yolk sac, the following provisional organs are known:
- 1. Amnion, whose task is to form an aquatic environment in which a future person could fully develop.
- 2. Chorion. This is practically the external organ of the embryo. Since the child must attach to the walls of the uterus, he needs to “bypass” its mucous protection, and the chorion helps the embryo in this.
- 3. Placenta. This is an important provisional human organ. It is he who helps the future person breathe, eat, secrete waste products, grow and develop before birth. The placenta is a reliable protector of the child and accompanies him until birth.
The main task of the yolk sac in embryo development is the formation of the primary circulatory system and blood vessels. Already on the 15th day after conception, the gradual formation of the very first human capillaries begins in the walls of the organ. A month after fertilization, the yolk sac temporarily becomes the main reproductive organ of the embryo: on the 29th day of the embryo’s existence, the first cells are released that have an influence on the formation of the sex of the future person.
The yolk sac gradually lost its digestive function, which it was endowed with in birds, fish and reptiles. In the human body, it could become the prototype of not only the circulatory system, but also most organs.
Sizes by week
The size of the fertilized egg in the early stages of pregnancy is the main parameter by which the doctor can judge how the baby is developing. The embryo is still very small, it is not possible to measure it and its individual parts, but the growth rate of the fertilized egg is a very informative indicator of the development of pregnancy as a whole.
The size of the ovum indicates not only development, but also compliance with certain obstetric dates. The fact is that at the very beginning of pregnancy, when the embryo is just emerging, there is not much difference in height and weight. It is much later that children in the mother’s womb begin to grow differently, in accordance with their genetic program (some are tall, others are small). In the meantime, all babies develop almost identically, so the growth rate of the fertilized egg is almost the same.
Errors and range of values in diagnostic tables are associated with the likelihood of late implantation, as well as with other factors that may affect the size of the fertilized egg, but do not pose a threat to the development of the baby.
A special technique is used for measurement. The ultrasound diagnostician draws a straight visual line through the fetal egg, which he sees on the monitor, so that the ends of the segment are located at points opposite to each other of the inner membrane of the fetal sac. This size is called SVD - average internal diameter.
This size is determined first. Then the coccyx-parietal size of the embryo itself is added to it. The size of the yolk sac is also considered important.
Growth rates can be seen in the table.
Conversion table for the size of the fertilized egg.
| Obstetric period, weeks | SVD, mm | KTE, mm | Yolk sac, mm | Area of the fertilized egg, mm^2 | Volume of the fertilized egg, mm^3 |
| 5 | 5-18 | 1-2 | – | 245 | 2187 |
| 6 | 13-22 | 4-5 | 3,0 | 363 | 3943 |
| 7 | 21-24 | 5-17 | 4,0 | 432 | 6912 |
| 8 | 29-30 | 10-25 | 4,5 | 675 | 13490 |
| 9 | 33-36 | 16-36 | 5,0 | 972 | 16380 |
| 10 | 39-44 | 24-49 | 5,1 | 1210 | 31870 |
| 11 | 47-51 | 34-58 | 5,5 | 1728 | 55290 |
| 12 | 56-57 | 42-73 | 6,0 | 2350 | 87080 |
| 13 | 63-65 | 51-87 | 5,8 | 3072 | 131070 |
Thus, it is considered completely normal if at 5 obstetric weeks - a week after the start of the delay, a fertilized egg is detected in a woman, the size of which will be 4-5 mm. And at 7 obstetric weeks, a fertilized egg measuring 20 mm will be completely normal. Detection of discrepancies between sizes and timing may indicate certain pathologies. But a lag should be understood as a significant deviation, for example, with a gestation period of 7 weeks, the size of the fetal sac is 4-5 mm. Let's look at what pathologies of the ovum there are and what the prognosis is.
Deviation of the size of the yolk sac from the norm during pregnancy
The parameters of temporary education are sometimes less than normal indicators or, conversely, exceed them. This phenomenon is considered an alarming, but at the same time subjective sign, so it is the doctor’s responsibility to carefully check and decipher it. So, before talking about the presence of any violations, a triple test is carried out. As part of this testing, markers of developmental abnormalities and chromosomal disorders of the embryo are studied.
The same test is relevant when the yolk sac “stayed” in its place for too long. If the presence of any irreversible intrauterine problem is confirmed, the pregnancy is artificially terminated.
The yolk sac is smaller than normal during pregnancy
Too small sizes of the temporary structure indicate progesterone deficiency. The situation can often be corrected with the help of medication. Pregnant women are prescribed Duphaston, Utrozhestan and other progesterone preparations.
In other cases, reduced parameters of the yolk bladder are observed if the organ begins to deteriorate prematurely. At this moment, the vital organs of the fetus have not yet had time to take shape and cannot work normally, so the embryo dies and the pregnancy ends in miscarriage. If spontaneous failure does not occur, the pregnancy is called regressive (frozen).
The yolk sac is larger than normal during pregnancy
When the size of the large yolk sac exceeds the norm, most likely, the gestational age was determined incorrectly, which often happens if a woman cannot boast of a regular monthly cycle. To clarify the situation, the specialist re-evaluates the size of the embryo and recalculates its “age” based on new data.
Note! You can only worry about the qualitative characteristics of the yolk sac, which differ from the norm, if there are other abnormalities detected on ultrasound. If the location of the embryo, its size and heart rate do not cause any complaints from the doctor, all metamorphoses of the yolk sac are perceived as an individual feature of a particular pregnancy, which is in no way reflected in the development of the 1st trimester.
To summarize: if the meeting of the egg and sperm ends in pregnancy, in the absence of critical days, the monitor of the ultrasound machine will display the corpus luteum, and another 6 weeks later the outline of the yolk sac will become visible. If the parameters of this temporary formation do not meet established standards, anomalies of embryonic development in the early stages of pregnancy cannot be ruled out. In this regard, the responsibility of every woman who is preparing to become a mother is to timely register and responsibly follow all doctor’s recommendations.
What can be seen on an ultrasound?
The normal time frame for visualizing the sac with the transvaginal method of examination is 1.5-3 months of gestation. The permissible deviation is two weeks (that is, 1 – 3.5 months). The absence of visualization of the sac indicates that the embryo has either already died or will die because it is not viable. The most informative studies are 6-7 weeks, 12-14 weeks.
During an ultrasound examination, a specialist evaluates the following characteristics of the organ:
- Size.
- Form.
- Location.
At 3-3.5 months, the formation reaches its maximum size, and subsequent ultrasound examinations may not show it at all.
What is a yolk sac?
This is how our consciousness works: for thousands of years, women have carried their children without thinking at all about some little things, for example, what stages of development the fetus goes through - the most important thing is that children are born viable and healthy. However, science has come a long way since then. Fetal ultrasound is now performed on every pregnant woman, and more than once. And just in the results of this examination, many discover that the fetus has some kind of yolk sac (a sac, as many affectionately call it). And, of course, it becomes interesting where it came from, why it is needed and where it is found in an adult.
Less than normal
The length and width of the organ in most patients coincide with standard values. A deviation is considered to be a discrepancy between the size of the uterus and the gestational age by 2 or more centimeters.
There are a number of reasons why an organ will melt more slowly than expected:
- small fruit size;
- failed miscarriage;
- incorrectly determined time of conception;
- lack of amniotic fluid;
- pathologies of intrauterine development.
A smaller uterus is typical for women who carry a pregnancy longer than expected and suffer from late gestosis. Oligohydramnios is especially dangerous in the last weeks of gestation. This condition can result in premature birth and lead to mental and physical retardation of the child.
In the early stages, when the fetus is mobile, the size of the uterus when examined on a chair may be less than the actual size. For example, at 10-11 weeks, fit 5 or 7 week sizes. If your baby is constantly twisting, bending and turning, it's easy to make mistakes. Ultrasound will help determine the actual period.
Yolk sac norm by week table
A special organ that forms in the initial stages of pregnancy and eventually atrophies until the end of the third trimester is called the yolk sac. It resembles the shape of a ring and has thin walls. The size of the yolk sac from the fifth to the twelfth week should be 3-6 millimeters in diameter.
The yolk sac is not visualized:
For example, ladies cite the results of an ultrasound, in which, for example, neither the embryo nor the yolk sac are visualized (that is, not visible). At the same time, the fertilized egg is present. Unfortunately, this situation is called “anembryony” - that is, the pregnancy did not take place.
The yolk sac is enlarged:
In other cases, on the contrary, it means that the yolk sac is larger than normal. The online consultant reassured the woman who came with a similar problem, explaining that this does not indicate any specific pathology and may be an individual feature. But, of course, it is necessary to control the development of the situation.
In general, every expectant mother should imagine what processes take place in her body at one or another stage of pregnancy or the menstrual cycle.
You should know how some medications, stress, and foods can affect the state of the reproductive system and fetus. Treat pathologies that may complicate pregnancy in a timely manner.
But the most important thing is to find a specialist who will actually, and not formally, take responsibility for your health, bearing a child and a successful birth.
Please login to leave comments.
What is the yolk sac during pregnancy?
Many expectant mothers, when entering an ultrasound room, hear about the yolk sac during pregnancy. However, the ultrasound doctor does not always give complete answers to all the questions of pregnant women.
What is the yolk sac during pregnancy - not to be confused with the corpus luteum
Even before conception, an egg is formed in one of a woman’s ovaries; when it unites with a sperm, it will give a new life - the life of your child.
Midway through the menstrual cycle, the sac or dominant follicle containing the mature egg bursts and the egg is sent to the uterus through the fallopian tubes. And in place of the burst sac, the formation of a corpus luteum occurs, the purpose of which is the production of progesterone.
reduce the risk of miscarriage and spontaneous abortion), prepare the mammary glands for lactation, lower blood pressure and suppress the immune system, which ensures the maternal body’s loyal attitude to a new, actively developing life.
Yolk sac, what is it?
After conception, on days 15-16 of pregnancy, the yolk sac is formed. Being a temporary organ of the baby, the yolk sac during pregnancy is an appendage located on the ventral side of the embryo.
It contains a supply of yolk necessary for development.
At first (before the fetus’s own organs begin to function), it performs the functions of the liver, spleen, and is also a supplier of primary germ cells, actively participating in the formation of immunity and metabolic processes.
The meaning of the yolk sac size
According to studies, an increase or, conversely, a decrease in the yolk sac, as well as an irregular shape, are often accompanied by a frozen pregnancy.
This is why it is so important to assess the size of the yolk sac during pregnancy.
During ultrasound examination in early pregnancy, it is the yolk sac that is an important diagnostic criterion. This is due to the fact that the size of the yolk sac in the first nine weeks of pregnancy significantly exceeds the size of the child.
During pregnancy, the yolk sac begins to be visualized at 5.5 weeks. In a normally developing pregnancy at 5-10 weeks, the size of the yolk sac should be less than 5.5 millimeters.
From 8 to 12 weeks of pregnancy, the size of the yolk sac should be more than 2 millimeters.
Yolk sac reduction
However, there are cases when its reduction (disintegration) is delayed, and its cystic degeneration occurs. This fact should not cause much concern, provided that all other indicators of the screening ultrasound were normal.
If concern persists, you can do an ultrasound again in about 2-3 weeks.
Functions of the yolk sac
What is the yolk sac during pregnancy? In the first 3 months of embryo development, this is perhaps the most important organ. Starting from the 6th week and ending with the period of the first trimester, the yolk sac is able to replace most of the internal systems of an adult in the embryo.
What organs are the prototype of the yolk sac? Among them:
- 1. Liver. At about 6 weeks it begins to produce alpha-fetoprotein, transferrins and alpha2-microglobulin. These proteins are vital for the normal growth and development of the embryo. The yolk sac is also called the primary human liver.
- 2. Sexual. By the end of the first month of development, the first germ cells appear in the embryo’s body with the help of the sac. If a girl is formed, then it is at this time that her eggs also develop. During this period, any stress is dangerous for the expectant mother, since due to impaired fetal development, her daughter may become infertile.
- 3. Kidneys and metabolic systems. One of the important functions of the yolk sac is excretory. At this time, it is a prototype of the kidneys, which function to cleanse the blood and remove excess fluid and dangerous toxins from the body.
- 4. Immune system. It begins to form in the body of a future person quite early, but at the same time it is not able to withstand external threats. The yolk sac perfectly protects the embryo from any external attacks.
- 5. Spleen. The organ allows the formation of macrophage cells in the body, whose task is to maintain “order” inside the small organism. In addition, do not forget about the main function of the yolk sac - the formation of blood cells and blood vessels.
At the end of the first trimester, when the fetus is 3 months old, all the main organs and systems are already present in its body. They allow the small embryo to function like an adult. At this time, the yolk sac is no longer necessary. After its expiration date, the organ begins to decline. Its size changes and decreases sharply. But it doesn't disappear completely. It becomes like a small cyst and is located at the base of the baby's umbilical cord throughout pregnancy until birth itself.
Treatment of pathology
When treating a pathology, the doctor sets two goals: finding and eliminating the cause of abnormal organ enlargement and neutralizing its consequences for the newborn. In case of a mild isolated form, which is not caused by chromosomal abnormalities, the expectant mother is prescribed drug therapy: taking diuretics, vitamins, injections of drugs that prevent hypoxia and placental insufficiency.
In the postpartum period, infants are given several courses of massage aimed at relieving muscle tone, strengthening, and eliminating neurological symptoms. Monitoring by a neurologist is required in the first weeks, months and years of life. Severe forms of pathology require surgical treatment after the birth of the baby.
The prognosis for a child with a severe form and chromosomal abnormalities is unfavorable.
What is a fertilized egg
The fertilized egg consists of embryonic membranes and an embryo. This period of pregnancy is its first stage of development. And it all starts with the fusion of two cells – male and female.
Then the fertilized egg actively begins to divide, first into two parts, then into four, and so on. The number of cells, like the size of the fetus, is constantly growing. And the entire group of cells that continue the division process moves along the fallopian tube to the zone of its implantation. This group of cells is the fertilized egg.
Having reached its goal, the fertilized egg attaches to one of the walls of the woman’s uterus. This occurs a week after fertilization. Until this time, the fertilized egg receives nutrients from the egg itself.
The fertilized egg, 2 weeks after implantation into the uterine cavity, nourishes the swollen mucous membrane of this reproductive organ, which is already prepared for the process of development and nutrition of the fetus until the time of formation of the placenta. The baby's place, or placenta, is created from the outer membrane of the fertilized egg at 3 weeks, which at this time is already thickly covered with villi. These villi at the site of attachment of the fertilized egg destroy a small area of the uterine mucosa, as well as the vascular walls. Then they fill it with blood and immerse it in the prepared area. In general, the fertilized egg is the very first sign of a normally ongoing pregnancy. It can be examined by ultrasound after two weeks of missed menstruation. Usually in this case the fertilized egg is visible for 3-4 weeks. The embryo becomes noticeable only at 5 weeks of pregnancy. However, if the doctor diagnoses the absence of an embryo in the fertilized egg of the 5th week - in other words, an empty fertilized egg, then the ultrasound is repeated again after a couple of weeks. Usually in this situation, at 6-7 weeks, the fetus and its heartbeat begin to be visualized. When the fertilized egg is still empty at 7 weeks, this indicates an undeveloped pregnancy
In addition to this complication, others may appear in the early stages of pregnancy - incorrect location of the fertilized egg, its irregular shape, detachments, and others. It is for this reason that it is important to undergo an ultrasound examination as early as possible, so that the situation can be changed if it can be corrected. Since in the first trimester (fertilized egg up to 10 weeks) there is a high probability of spontaneous miscarriage, detachment and other pathologies
However, enough about the sad things.
Fertilized egg at 6 weeks
and until this stage of pregnancy it has an oval shape.
And an ultrasound examination usually evaluates its internal diameter - the SVD of the fetal egg. Since the size of the ovum at 7 weeks
or at another stage of pregnancy is a variable value, there is an error in identifying the gestational age using this fetometric indicator.
On average, this error is 10 days. Gestational age is usually determined not only by this indicator, but also by the values of the coccygeal-parietal size of the fetus and other indicators, which are also very important
Diagnostics using an ultrasound machine
The most important ultrasound examination during pregnancy is the first one. It is carried out up to 12 weeks during the 1st trimester of a woman’s pregnancy. During this fetal ultrasound, it is impossible to determine the sex and possible size of the child at birth, but diagnosis at this particular time helps to learn about possible developmental abnormalities and dangerous genetic diseases.
Using ultrasound, a doctor can diagnose pathologies in the development of the yolk sac or disturbances in its functioning during a frozen pregnancy. At this time, it is necessary to have an abortion, since a fetus that has stopped developing poses a mortal danger to the mother.
The provisional organ is most noticeable by 6 weeks after conception. It is at this time that its parameters, in accordance with the size of the unborn child, are greatest. By 6 weeks, the size of the human organ reaches 5 mm. In the future, they may increase, but the yolk sac will not be noticeable as before, due to the sharp growth of the embryo itself.
During fetal development in the first trimester, the size of the provisional organ gradually decreases, which is clearly visible on an ultrasound examination of the fetal egg. After some time, the organ becomes like a kind of bubble. This suggests that the body of the future person no longer needs it.
By the 12th week of pregnancy, the pouch gradually begins to disappear, but does not disappear completely. It literally “retracts” into the child’s body cavity and becomes a small cyst. At the beginning of the second trimester, the size of the organ is so small that it is no longer possible to determine its position using ultrasound.
The disappearance of the yolk sac indicates that the embryo has carefully established itself in the mother’s body and carries out nutrition and respiration through the umbilical cord and placenta.
A special organ that forms in the initial stages of pregnancy and eventually atrophies until the end of the third trimester is called the yolk sac. It resembles the shape of a ring and has thin walls. The size of the yolk sac from the fifth to the twelfth week should be 3-6 millimeters in diameter.
What does the corpus luteum mean during pregnancy?
Like the yolk sac, this organ appears early in pregnancy and is present temporarily. The formation appears immediately after the female cell, ready for fertilization, leaves the follicle. The granulosa cells of the ruptured follicle become the material for the formation of the corpus luteum.
If the meeting of the female and male cells is successful, the corpus luteum begins to develop with the assistance of human chorionic gonadotropin. This structure lives for 10 - 12 weeks after conception, and begins to dissolve as soon as the placenta matures. The main task of the corpus luteum is to supply the mother’s body with progesterone, with a deficiency of which the very existence of pregnancy is in question. Also, with the participation of this hormone, the processes that trigger menstruation are blocked. Later, the placenta will be responsible for the safety of the little man, so there will no longer be a need for additional protection.
Gestational sac and its role in embryo development
The yolk sac is a membrane membrane attached to the embryo on its ventral part. This formation provides early nutrition to the fetus. The gestational sac functions as the development of the cardiovascular system of the human embryo before internal circulation begins.
The gestational sac is the only available structure that can be used to determine the existence of an intrauterine pregnancy as long as the embryo cannot be identified. The yolk sac during pregnancy, if it develops normally, is visible in the early stages using ultrasound. Determination of the gestational sac at the fifth week is a critical reference point in early pregnancy monitoring.
The normal functioning of the yolk sac is important at the beginning of the embryonic circulation. Transportation of blood to the walls of the sac occurs through the primitive aorta. Its circulation passes through a wide network of capillaries and returns through the vitelline vein to the tubular heart of the embryo. Through this circulation, nutrients from the yolk are absorbed and transferred to the embryo.
- At what stage does an ultrasound show pregnancy and gender?
- First ultrasound during pregnancy: at how many weeks
At the beginning of the fifth week, the appearance of the yolk sac is a small pear-shaped umbilical vesicle opening into the digestive tract of the embryo in a long, narrow tube. It is called the vitelline duct. As a rule, the vitelline duct closes completely due to tissue proliferation during the 7th week. Subsequently, the child’s gastrointestinal tract is formed from it.
Ultrasound distinguishes the yolk sac as a small oval body, with a diameter ranging from 1-6 mm. When the development of the fetus inside the womb approaches the end of the 11th week, the functioning of the yolk sac stops, it decreases in size, reduces and appears as a cyst-like formation at the umbilical cord base. The membrane tissues that make up the fetal sac provide hematopoietic, excretory, immunoregulatory and synthetic functions, as well as metabolic processes, until the embryo develops its own organs and begins to function independently.
If the process of reduction of the fetal sac develops prematurely, before the liver, spleen, and reticuloendothelial system of the unborn baby are formed, then a miscarriage or fetal death may occur. Thus, three main stages of development of the yolk sac can be distinguished:
- The primary yolk sac is the umbilical vesicle formed during the second week of gestation.
- Secondary - by the end of the second week, a new cavity is released from the primary sac as a result of the division of hypoblast cells, the walls of which are transformed into two-layer ones. Meanwhile, the cells in the walls of the primary yolk sac degenerate.
- The final yolk sac forms during the fourth week of pregnancy during the development of the embryo's internal organs. Part of the yolk enters the digestive canal of the embryo. The remaining part is the final yolk sac.
Purpose of the yolk sac
The yolk sac plays an important role in the formation of the embryo, especially in the early stages of its development. It performs a number of fundamental functions, without which further successful pregnancy will be impossible:
- Performs the function of the liver and synthesizes important proteins: alpha 2-microglobulin, alpha-fetoprotein, transferrins, etc.
- Transports the first germ cells to the embryo, as a result of which its gender is decided.
- Forms the fetal immunity, acting as a macrophage system (reticuloendothelial system).
- It forms in its walls the first red blood cells and a network of tiny capillaries, from which the circulatory system will be formed, feeding the embryo with all the necessary microelements.
After the 12th week of pregnancy, the bladder stops functioning, gradually shrinks and decreases in size. On the body of the embryo it remains in the form of a cystic formation near the umbilical cord.
Role of the yolk sac
The yolk sac is a temporary (provisional) organ, but without it the normal course of pregnancy and embryo development is impossible. In the early stages, the size of the yolk sac exceeds the size of the embryo and amniotic cavity. The yolk sac actively grows from 6 to 12 weeks of gestation, after which it gradually decreases in size and completely disappears.
On days 18-19 from conception, the yolk sac becomes the focus of hematopoiesis. In its walls, areas of erythropoiesis are formed, and the first red blood cells are formed. Subsequently, a branched network of capillaries is formed here. Primary red blood cells, leaving the yolk sac, enter the circulatory system of the embryo and are carried through the bloodstream throughout the body.
From the 28th day from the moment of conception, the yolk sac begins to produce primary germ cells of the embryo. Subsequently, the germ cells migrate from the yolk sac and reach the gonads (sex glands). 4-5 weeks of pregnancy is an important stage in the development of the fetal reproductive system. Any negative effects during this period (infections, radiation, medication) can disrupt the formation of the gonads of the embryo and cause infertility.
From 2 to 6 weeks of pregnancy, the yolk sac acts as a liver for the embryo. The walls of the yolk sac synthesize important proteins and enzymes necessary for the normal development of the entire organism. In particular, AFP (alpha fetoprotein) is produced here. In the fetal circulatory system, AFP binds to PUFAs (polyunsaturated fatty acids) and transports them to all cells and tissues. AFP also suppresses the immune response to newly synthesized proteins, allowing metabolic processes to proceed at the desired rhythm.
Other functions of the yolk sac:
- regulation of the fetal immune system;
- synthesis of hormones;
- creating conditions for adequate metabolism;
- excretion of metabolic products.
The yolk sac performs all its functions until the main internal organs are formed in the fetal body and take over this work. After 12 weeks there is no need for a yolk sac. By the beginning of the second trimester, only a small cystic formation at the base of the umbilical cord remains from the yolk sac.
What does the yolk sac mean during pregnancy?
The yolk sac is a non-permanent organ located adjacent to the embryo. It is formed 15 - 16 days after fertilization, during the active maturation of placental tissue. The yolk substance of the zygote becomes overgrown with embryonic cells and ultimately takes on the appearance of a rounded closed structure with a thin-walled membrane. It is fixed near the abdominal part of the embryo, works actively in the first days of its existence, and on ultrasound it begins to be clearly visible from the 6th week from the moment of fertilization.
If we talk about the diameter of this specific formation, then from 6 to 10 weeks it is normally 5.5 mm. A little later, starting from week 8, the yolk sac decreases to approximately 2 mm. At week 12, ultrasound no longer detects it.
Sensations during organ growth
The enlargement of the uterus occurs slowly and imperceptibly, so a pregnant woman usually does not feel anything. Only in the 1st trimester can pulling sensations appear caused by softening and tension of the ligaments.
Pain, as a rule, occurs when the uterus enlarges too quickly; discomfort is also noted in the case of scarring on the walls of the organ after previous pregnancies. If any unpleasant symptoms develop, you should consult a gynecologist.
The growth of the uterus after 4–5 months of pregnancy causes great inconvenience. An expanding belly makes it difficult to bend over, making it difficult to find a comfortable position. The internal organs are compressed and displaced under the influence of the uterus, heartburn, flatulence, and frequent urge to go to the toilet appear. Constriction of the rectum leads to constipation. Due to the pressure of the grown fetus on the diaphragm, breathing difficulties and shortness of breath appear.
At the end of the 2nd trimester, many women experience a change in gait - movements become more measured, the body leans back, and the legs are placed wider. The reason for this transformation is a shift in the center of gravity.
Measuring the length and width of the uterus helps to detect abnormalities in time. However, you should not engage in self-diagnosis and worry about minor violations. Remember, every pregnancy is unique and follows an individual scenario.