Waiting for the birth of a new person is always a difficult and exciting period in a woman’s life. Each week has its own characteristics, so the expectant mother needs to be careful. The 17th week of pregnancy is the beginning of the fifth lunar or obstetric month (there are exactly 28 days in a lunar month). Let's figure out what characterizes this period.
The 17th obstetric week of pregnancy has arrived, which means that your unborn baby was conceived approximately 14 weeks ago. As the expectant mother has probably already learned, the weeks are counted from the first day of the last menstruation, that is, the first two weeks, in fact, there is no pregnancy yet. Thus, the 17th week of pregnancy from conception will occur in about half a month, and during this time your boy or girl will already have time to grow significantly.
What happens in the female body at 17 weeks?
In the fifth obstetric month of pregnancy, the uterus and the fetus inside it grow at an incredibly fast pace. The woman’s cardiovascular system works intensively, as the blood volume has increased significantly due to the placenta being saturated with blood vessels. A rapid heartbeat may be a manifestation of the active work of this organ, which conducts nutrients to the fetus. The fragility of blood vessels due to the increased load on their walls sometimes leads to nosebleeds.
An increase in the total volume of fluid in a pregnant woman’s body affects the volume of vaginal discharge and causes increased sweating. Careful adherence to personal hygiene rules can protect a woman from negative feelings.
A belly that is too small is not a cause for concern, the main thing is that the baby’s heartbeat is clear and audible.
Recommendations
- Try not to expose yourself or your baby to stress, loud noise or irritating light. During this period, the child is very sensitive to sudden and strong changes in the external environment.
- You should give preference to sleeping and resting on your side rather than on your back to avoid squeezing the vena cava.
- When you feel the fetus moving for the first time, it would be a good idea to keep an “observation diary” to track and control the baby’s activity, and consult a doctor if there are serious deviations from the baby’s usual behavior in the womb.
- Do not ignore ailments, diseases and do not self-medicate, but seek help from specialists.
What's happening to the baby?
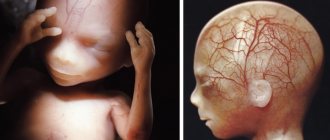
At the 17th week of pregnancy, the formation of fetal adipose tissue begins, but its skin still remains thin and transparent. The fat layer will be used for normal thermoregulation of the baby immediately after birth. The sensitive skin of the fetus is covered with pinkish-white vernix and fluff - lanugo.
Fetal parameters at 17 weeks:
- Weight – 140 g;
- KTR (coccygeal-parietal size) – 13 cm;
- Height – 15-18 cm.
The unborn child's hearing aid is ready for use, and he does not like loud, sharp sounds. Using an ultrasound scanner, you can see how the baby reacts to noise with chaotic, rapid movements. From this week we can say with confidence that he distinguishes the voice of his mother and father, loves melodic singing and pleasant music. Fetal development researchers say that babies who are spoken to by their parents during pregnancy recognize their voices after birth and respond positively to the music they were previously exposed to listening to.
The child distinguishes not only sounds, but also reacts to bright light, turning his face to a bright lamp brought to his stomach, although his eyes are still covered with eyelids.
Development of internal organs at 17 weeks:
- The immune system began producing its own interferon and immunoglobulin to further protect the fetus from infections;
- The endocrine glands (pituitary and adrenal glands) produce their own hormones;
- The heart pumps blood intensively, the fetal heart rate is still twice the mother's heart rate;
- Following the rudiments of milk teeth, the rudiments of permanent teeth are formed;
- The fetus may swallow and hiccup;
- The female fetus develops a uterus;
- The testicles of a male fetus are located in the abdominal cavity, they already contain the rudiments of the first sperm.
The fetus at 17 weeks is actively moving, moving into the uterine cavity. He no longer differs in appearance from a newborn baby in anything except size - his body proportions have returned to normal.
Amniocentesis – when is it necessary and is the procedure safe for the fetus?
Surveys
The optimal pregnancy period for undergoing the second screening is seventeen weeks. Although this examination is allowed during the period of 16-20 obstetric weeks. Indications for undergoing the second screening are:
- cases of frozen pregnancy or late miscarriages in the anamnesis;
- mother's age is more than 35 years;
- presence of genetic diseases in the family;
- viral diseases suffered by a woman in the first trimester;
- taking medications that may affect the development of the fetus, and a number of other factors that could affect the course of pregnancy.
Advice! If all pregnant women need to undergo the first screening, then the second, as a rule, is prescribed according to indications. You can undergo examinations at your own discretion if a woman wants to make sure that everything is fine with her baby.
The examination consists of two parts - ultrasound and biochemical blood tests.
When performing an ultrasound at 17 weeks of pregnancy, the following is performed:
- fetometry (determining the size of the fetus);
- diagnostics of the development of internal organs;
- assessment of facial structure development;
- amount of amniotic fluid;
- In addition, the specialist will check the condition of the placenta.
During the second pregnancy screening, you do not necessarily need to donate blood. If an ultrasound performed at the 17th week of pregnancy gives good results, it is not necessary to send the expectant mother for biochemical tests. But in some cases, a triple test is prescribed, during which the content in the blood is determined:
- hCG;
- AFP;
- free estriol.
But even if the results of the second screening are not very good, you should not be upset. This examination does not make a diagnosis. If the examination results show a high risk of genetic pathologies in the fetus, the expectant mother will be referred to a geneticist for consultation. And, if necessary, a number of other examinations will be prescribed that will refute or confirm the presumptive diagnosis.
What's happening to mom?
The appearance of a pregnant woman changes. Her nose and lips may swell, her facial features may become somewhat rounded, and an unexpected blush may appear on her cheeks. The thyroid gland is currently experiencing increased stress, intensively producing hormones. Hyperfunction of this organ can cause weakness, rapid heartbeat, and excessive sweating. With such symptoms, you should consult a doctor to correct the condition.
An increase in the size of the uterus leads to displacement of the organs of the digestive tract. Compression of the stomach and intestines results in heartburn and flatulence. The problem can be partly solved by the correct diet - you need to eat 3-5 times a day in small portions.
Increased stress on the kidneys, heart, musculoskeletal and digestive systems leads to increased fatigue and requires frequent rest.
How does the stomach change?
At this stage, the belly will most likely be visible in plump women, as well as in those undergoing a second and subsequent pregnancies. Primiparas with a slender figure, strong abdominal muscles and trained abs can keep their situation a secret for now. The belly may be barely noticeable at 17 weeks if the baby is located at the back wall of the uterus or in its lower section.
The main rule is that you can no longer wear clothes with a tight waistband, tight underwear, or wardrobe items made of synthetic fabrics.
Second screening at 17 weeks
The optimal time to conduct a second screening study is the period from 16 to 20 weeks. Ultrasound at the 17th week of pregnancy is carried out as part of this set of examinations. It also includes a biochemical blood test. It is worth noting that the second screening is often carried out according to indications or in the presence of abnormalities identified during the first study. At 17 weeks of pregnancy, ultrasound determines:
- the structure of the facial part of the skull, the location of the ears and eyes;
- condition of the spinal column;
- presence of visual structural anomalies;
- state of the respiratory system.
If there are suspicions of genetic abnormalities, a biochemical blood test is performed. During implementation, the following indicators are assessed:
- AFP (α-fetoprotein);
- EZ (estriol);
- HCG (human chorionic gonadotropin). The norms for the main parameters of the second screening are given in the tables above.
First fetal movements
At week 17 you can already feel faint fetal movements. They are still so tender that, without experience of pregnancy, it is difficult to distinguish them from the sensations caused by food or gases moving through the intestines. If a woman does not notice fetal movements by this time, it is advisable to contact her gynecologist so that he can listen to the baby’s heartbeat and perform an ultrasound. The onset of movements at 22 weeks during a pregnancy proceeding without pathologies is also a variant of the norm, so you should not be upset in advance.
Woman's well-being
Let's figure out what happens at 17 weeks of pregnancy in the body of the expectant mother. As a rule, the sensations at 17 weeks of pregnancy are neutral. During a normal pregnancy, a woman should not feel pain or discomfort. However, certain discomfort associated with the growth of the uterus may occur.
At the 17th week of pregnancy, the uterus continues to grow, gradually expanding not only to the sides, but also to the top, taking on the shape of a pear. At 17-18 weeks of pregnancy, the uterus can be easily felt independently; it is located 5-7 cm below the navel. Unpleasant sensations may appear due to the fact that the growing uterus increasingly compresses the internal organs, putting pressure on the intestines and bladder.
The fact that by this period the volume of blood in her body increased by about 40% also causes some discomfort to the woman. This leads to increased stress on the heart and blood vessels. Therefore, it is possible that unpleasant moments such as:
- nosebleeds;
- bleeding gums;
- a serious complication is the development of varicose veins.
Pregnancy at 17-18 weeks is often marked by weight gain and a growing belly. You need to monitor your weight gain very carefully, as a sudden gain has a negative impact on the baby’s development. Optimal weight gain per week should not exceed 0.5 kilograms. Of course, you don’t need to starve, but you need to carefully monitor your diet.
Movements
Most expectant mothers really want to feel the fetal movements faster. When can this significant event happen? There is no exact answer, everything is very individual. As a rule, the first movements can be felt between 16 and 22 weeks.
Often, expectant mothers begin to panic and ask the doctor why I don’t feel any movements, although other women already feel their baby pushing in their stomach? There is nothing pathological or scary about the fact that you do not feel fetal movements at 17 weeks. Everything here is very individual. Wait a little and you will definitely feel how actively your little boy or girl can move.
Advice! If a girl is expecting her first child, the first movements are usually felt at 20 or even 22 weeks. And if a woman already has children, then you can feel the baby’s activity earlier.
Analyzes and examinations
When visiting a antenatal clinic, the obstetrician-gynecologist will measure the pregnant woman’s blood pressure, weight, uterine height, offer a urine test and undergo a “triple test” of the second screening, if the expectant mother has not already undergone it.
Blood parameters studied and their norm:
- Chorionic gonadotropin (hCG) – from 6140 to 103000 honey/ml;
- Alpha fetoprotein – from 30 to 90 honey/ml;
- Free (unconjugated) estriol – from 9.9 to 18.9 nmol/l.
Deviation from the norm indicates possible chromosomal pathologies of the fetus and genetically determined diseases.
What examinations need to be completed
If the pregnant woman did not have a scheduled appointment with her gynecologist in the previous week, now is the time to visit him. In the doctor’s office, a woman will have to undergo the usual examinations:
- measure pressure;
- record changes in weight;
- measure the volume of the abdomen and the height of the uterine fundus;
- listen to the baby's heartbeat.
In addition, the doctor will look at the results of urine and blood tests taken the day before.
Also, an appointment at 17 weeks of pregnancy can be scheduled to undergo or decipher the results of a second screening, which includes ultrasound screening and a triple genetic test.
These examinations are needed to determine the possible risks of abnormal development of the child.
In cases where a pregnant woman does not undergo screenings and does not have any indications (pain, suspicion of a missed abortion, spotting), an ultrasound at the seventeenth week is not necessary. Well, if it is prescribed, then the woman has the opportunity to accurately find out the gender of her child.
Pregnancy after IVF
In vitro fertilization of an egg and subsequent pregnancy require a woman to be very careful about the slightest changes in her well-being. High doses of hormones during preparation for IVF can disrupt the endocrine status of the pregnant woman, so it needs to be closely monitored by conducting additional studies.
Hormonal therapy in preparation for artificial insemination leads to disruption of hemostasis (blood circulation), which already carries an additional burden. Women who become pregnant through IVF most often have a history of complications of gynecological diseases, which further increases the risk of miscarriage. During such a pregnancy, an ultrasound is often performed, hormone levels are measured, and the development of the unborn baby is screened.
Painful sensations
The threat of spontaneous abortion at this stage is low, and the sensations from stretching the uterine ligaments come first. The nature of the pain can be aching or “shooting” with a rapid change in body position, its intensity ranges from minor to severe sensations similar to pain during menstruation. The best tactic is to wear a prenatal bandage that supports the uterus, rest more often, and do not make sudden movements.
Pain in the tailbone and in other parts of the spine may be due to the fact that the weight and volume of the uterus have increased, and the load on the spinal column has increased. In this case, swimming, water aerobics, and feasible physical education exercises for pregnant women will help.
Uterus
The fact that a woman’s body changes due to pregnancy is already noticeable to the naked eye. But even more significant changes occur inside the female body. For example, the uterus can already be compared in size to a melon and weighs approximately 250 g.
The rapid growth of the uterus “forces” the internal organs to shift, which can cause some discomfort and changes in the woman’s well-being. At this time, the muscles of the uterus should not be hypertonic. But if a woman feels a nagging pain in the lower abdomen, it seems to her that her stomach is turning to stone, then she should seek medical help.
Vaginal discharge
Light translucent discharge of a small volume, with a slight sourish odor, is the norm at 17 weeks of pregnancy. The addition of pus, mucus, flakes, curdled clots, a change in color from white to yellow or green are signs of vaginal infection or candidiasis. During pregnancy, local immunity suffers, so inflammatory pathologies appear more often than usual. Any change in the nature of vaginal discharge is a reason to visit a doctor and get a smear for urogenital infections.
Candidiasis (thrush) often accompanies pregnancy, manifested by burning and itching in the vagina, hyperemia of the mucous membrane of the external genitalia and cheesy discharge. Normally, the fungus of the genus Candida is always present in the female intimate microflora in small quantities. The onset of pregnancy is the reason for its rapid growth. For candidiasis, both sexual partners must be treated, otherwise relapses of the disease are inevitable.
Complications
Unfortunately, not everything always goes smoothly. Sometimes various complications occur that can negatively affect the course of pregnancy.
Fading
This is perhaps the most serious complication, as a result of which the fetus stops developing and dies. In the second trimester, such a complication does not occur too often, but it cannot be excluded.
A frozen pregnancy is discovered at the next examination. It is extremely difficult to independently feel that the pregnancy has stopped developing.
Discharge
A dangerous complication is the appearance of bloody discharge, accompanied by nagging pain. These symptoms may be a sign of an incipient miscarriage.
In principle, the reason for contacting a gynecologist should be any atypical discharge at the 17th week of pregnancy. Normally, the discharge is moderate, homogeneous, milky-white in color and practically odorless. There should be no unpleasant sensations in the form of itching and burning.
The appearance of yellow or greenish discharge, as well as heterogeneous foamy or grainy leucorrhoea are signs of a violation of the normal composition of the vaginal microflora or infection. If such signs appear, you need to take a smear from a gynecologist, and then undergo the necessary treatment.
Pain
If your stomach hurts at 17 weeks of pregnancy, this is not always a sign of illness. During this period, the uterus is actively growing, so minor nagging pains may be associated with sprained ligaments. Sometimes women complain that pain occurs in the form of lumbago when suddenly changing position.
To avoid unpleasant sensations, you need to try to move more smoothly and rest more often.
However, stomach pain can also occur for other reasons. Thus, pain in the upper abdomen may be associated with disorders in the digestive system, for example, gastritis. And back pain, accompanied by discomfort when urinating, is a sign of the development of an inflammatory process in the kidneys or bladder.
Cold
During the entire “pregnant period,” the immune system does not work at full strength, so women often suffer from acute respiratory viral infections and other colds. Of course, a cold at the 17th week of pregnancy no longer poses a great danger to the baby, but this does not mean that you can self-medicate or endure the disease on your feet.
Colds should be treated under the supervision of a doctor. Bed rest at fever is required.
So, 17 weeks of pregnancy is the beginning of the fifth obstetric month. This time is quite calm, since the main threats of the first trimester are already behind us. But even during this period, it is important to closely monitor your well-being and regularly visit a gynecologist. In this case, if complications arise, you can take the necessary measures in a timely manner and avoid negative consequences.
Taking vitamins and medications
Cramps in the limbs, brittle hair and nails, unusual taste preferences are possible symptoms of vitamin deficiency and mineral deficiency. Your gynecologist will recommend special complexes for pregnant women. To compensate for the deficiency of essential substances, you need to diversify your diet with vegetables, fruits, and berries. Additionally, you should take Iodomarin or Iodine-active to support the functioning of the thyroid gland.
Any medications during pregnancy are taken only if absolutely necessary and in consultation with your doctor. There is a very small number of pharmaceuticals approved for expectant mothers. When treating somatic diseases, the attending physician must know about the patient’s pregnancy.
Intimate relationships
A woman’s sexuality does not disappear during pregnancy; on the contrary, hormonal changes lead to increased desire. Sexual intercourse gives an emotional surge and provokes the production of endorphin, called the “hormone of joy.” Intimate relationships stimulate blood circulation in the reproductive organs and help strengthen mutual understanding between spouses.
During this period of pregnancy, the following contraindications to sex may occur:
- Placenta previa;
- Risk of miscarriage;
- Infections, inflammatory diseases of the genital organs of both spouses.
The appearance of pain and bleeding is a reason to stop sexual intercourse and consult a doctor.
Discharge
This week, the pregnant woman’s natural vaginal discharge should not change in any way. They remain light/translucent in color, odorless and without any impurities.
Any changes in color (yellow, green, brown discharge), smell (appearance of a sharp sour odor), consistency (curdled, heterogeneous) should be the reason for a visit to the gynecologist who is observing the pregnant woman.
All these changes indicate problems during pregnancy and can harm the health of the mother and child.
Nutrition at 17 weeks
The main requirements for a pregnant woman’s diet are high-quality foods rich in nutrients and their balanced inclusion in the menu. The more varied the dishes that come to a pregnant woman’s table, the easier it is to provide the fetus with material for the formation of organs and tissues.
Diet: frequent meals in small portions. To avoid stagnation in the digestive system (heartburn, constipation, flatulence, bloating), after eating you need to take a walk in the fresh air and move around.
Recommended products and dishes:
- Soups and jellies to prevent heartburn;
- Fermented milk products, cheese, cottage cheese as a source of calcium;
- Foods containing large amounts of iron for the production of oxygen-carrying red blood cells in the blood (liver, beef, pomegranate juice, apples).
You should not overuse fatty and fried foods, pickles and smoked meats, which provoke increased secretion of gastric juice.
A special problem is frozen pregnancy
Cessation of fetal development can occur for various reasons. Among them are hormonal imbalance, Rh conflict between mother and child, and the consequences of infection. The body may not immediately begin to reject the fertilized egg; first, the pregnancy fades. This condition is sometimes not accompanied by any symptoms, but during the next examination, the obstetrician-gynecologist will definitely diagnose the problem.
Symptoms:
- Lack of fetal movements;
- Temperature increase;
- Bloody or bloody discharge;
- No signs of pregnancy (toxicosis, breast swelling);
- Pain in the lower abdomen and lower back.
A frozen pregnancy is terminated in a hospital setting, the woman is prescribed a course of anti-inflammatory drugs and procedures, and is offered psychological assistance.
Fetal growth and development
The fetus at the 17th week of pregnancy reaches a length of 11-13 cm, and its body weight can range from 100 to 140 grams. During this period, the baby is actively gaining weight.
Baby size now
Like an orange
Height13 cm
Weight140 g
At this stage, the following occurs in the fetal body:
- The process of formation of subcutaneous fatty tissue intensifies, the baby looks more developed, his body becomes more proportional.
- The swallowing process is activated. A child can swallow up to 400 g of amniotic fluid during the day, as a result of which he occasionally experiences hiccups.
- The baby reacts strongly to loud sounds, so a pregnant woman should refrain from listening to loud music or attending concerts.
- In girls, the uterus is actively developing. In boys, the external genitalia are sufficiently formed that the sex of the fetus can be determined by ultrasound.
- The process of laying permanent teeth occurs.
- The fetus’s own immune system is activated, so the child at this stage is well, although not 100%, protected from infections.
- Fetal movements become more intense, but during the first pregnancy the woman usually does not feel them at 17 weeks. Therefore, if the expectant mother does not yet have movements in her tummy, there is no need to worry, especially if this is not the second or third pregnancy. Everything has its turn, and the baby will still have time to express himself with his first movements.
If we take into account that the 17th obstetric week of pregnancy is only 15 weeks of development of the fetus itself, then we can answer the question of how many months it is. The 17th week is 3.5 calendar months of fetal development from the moment of conception or almost 4 calendar months starting from the first day of the last menstruation.