What you need to know about a frozen pregnancy, how to reduce the likelihood of miscarriage, says Doctor of Medical Sciences, Professor Igor Makarov.
In a non-developing pregnancy, which is also called a “frozen pregnancy,” the embryo/fetus dies, but there are no clinical signs of spontaneous miscarriage.
Causes of non-developing pregnancy
The reasons for a non-developing pregnancy are very diverse. Thus, stopping the development of the embryo/fetus can be caused by an inflammatory process as a result of the action of various microorganisms. Most often, the causative agents of inflammation are: streptococci, staphylococci, Escherichia coli, Klebsiella, rubella virus, cytomegalovirus, herpes simplex virus, Coxsackie virus, mycoplasma, chlamydia, treponema, mycobacteria, toxoplasma, plasmodia, fungi (thrush).
Chronic infectious diseases in women most often do not directly lead to intrauterine fetal death, but cause certain disorders that contribute to it. For example, as a result of direct exposure to an infectious factor, a heart defect is formed in the fetus, which prevents its further normal development. However, not always and not every infection leads to the death of the embryo. The impact of the infection depends on the route of its penetration, the involvement of the fetus and amniotic membranes in infection, the type and activity of the pathogen, the number of penetrating microorganisms, the duration of the mother’s illness, the activity of the body’s protective capabilities and other factors.
Microorganisms can penetrate the uterus from the underlying parts of the reproductive system, infecting the amniotic fluid, which is then swallowed by the fetus. The infection can spread through the amniotic membranes and further to the fetus, causing damage to its internal organs, which, in turn, is the cause of its death. The infection can reach the fetus from chronic foci of inflammation in the fallopian tubes and ovaries.
The death of the embryo/fetus may be due to a violation of the immune relationship, taking into account that the fertilized egg is half foreign to the mother's body. In this case, rejection reactions are activated, aimed at damaging the fertilized egg and removing it from the uterus. A non-developing pregnancy can be caused by various chromosomal abnormalities : in the first 6-7 weeks of pregnancy, chromosomal changes are present in 60-75% of cases of spontaneous abortion, in 12-17 weeks. - in 20-25%, in 17-28 weeks. - in 2-7%. With age, the likelihood of developing chromosomal disorders increases. The causes of the development of chromosomal disorders are also unfavorable external factors. Stopping the growth and development of the embryo/fetus can be caused by thrombotic complications caused by genetic defects in the blood coagulation system of a pregnant woman. The most common among them are: factor V Leiden mutation, prothrombin G202110A mutation, methyltetrahydrofolate reductase mutation, plasminogen activator gene polymorphism, platelet receptor polymorphism.
Blood coagulation disorders caused by antiphospholipid syndrome also determine the unfavorable development of the embryo/fetus. In the early stages of pregnancy, the role of direct damaging effects of antiphospholipid antibodies on the structures of the fetal egg, followed by spontaneous termination of pregnancy, cannot be excluded. With this pathology, the process of implantation of the fertilized egg is disrupted. In addition, with antiphospholipid syndrome, there is a decrease in the formation of blood vessels in the placenta and a decrease in its function, which can cause a non-developing pregnancy. Another cause of impaired development of the embryo and placenta in antiphospholipid syndrome is thrombosis and damage to the uteroplacental vessels.
Hormonal changes are also among the causes of miscarriage . Impaired formation and decreased function of the corpus luteum in the ovary leads to a decrease in progesterone and inadequate preparation of the uterus for implantation of the fertilized egg. In this regard, the formation of the uteroplacental blood circulation is disrupted, which entails a decrease in the blood supply to the embryo/fetus and its death. Often, such disorders occur with excessive accumulation of male sex hormones in a woman’s body (Stein-Leventhal syndrome, adrenogenital syndrome), with decreased or increased thyroid function.
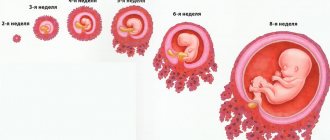
The shorter the gestation period, the higher the sensitivity of the embryo/fetus to the action of damaging factors. However, it decreases unevenly throughout intrauterine development. There are critical periods during pregnancy in which the fertilized egg, embryo, fetus are especially vulnerable to adverse effects: the period of implantation (7-12 days), the period of embryogenesis (3-8 weeks), the period of placenta formation (up to 12 weeks), the period of formation the most important functional systems of the fetus (20-24 weeks).
Abnormal development of the fertilized egg
In addition to deformation of the fertilized egg, the development of any anomalies is possible. Many of them can cause miscarriage or fetal death. The most common anomalies are presented below.
1. If there are two embryos in the fertilized egg, then this is not an anomaly, but rather the norm for the development of twins. The sizes of embryos may differ from each other. A difference of several millimeters is most often characteristic of monochorionic twins. However, at an early stage it is impossible to accurately determine whether the children will be twins or twins.
2. Small fertilized egg. This pathology is diagnosed by comparing the gestational age and the size of the ovum. Such studies help determine the correct development of the fetus in the uterus. The gestation period is also determined by the size of the fertilized egg. It is necessary to carefully monitor the development of the fertilized egg; too slow growth may indicate fetal fading. In this case, it is advisable to prescribe the patient a blood test for hormone levels.
3. If the fertilized egg is larger than the embryo, then the pregnancy may be frozen. Pregnancy can also be anembryonic. All signs of pregnancy are characteristic, the membranes of the fetus are formed, but the embryo is missing. Anomalies can only be diagnosed by ultrasound examination of the fetal egg no later than 6-7 weeks after conception. In this case, it is very important to establish the exact duration of pregnancy.
4. Elongated shape of the fertilized egg. Normally, the fertilized egg should be round in shape. Elongated contours may signal the possible loss of a child. The reason most often lies in uterine hypertonicity. It is important to diagnose the deformity in time and take measures to reduce tone with the help of antispasmodics. The fetus can be saved if it continues to develop and a heartbeat can be heard. The patient needs to stop sexual activity, minimize physical activity and avoid emotional turmoil. If this pathology is present, complete bed rest is prescribed. Ultrasounds are performed every few days to monitor changes in the gestational sac.
5. Abnormal location of the fertilized egg. Usually the egg is implanted at the bottom or center of the uterus, but sometimes it occurs in the area of the internal os.
6. Death of the fetus inside the womb. Diagnosed by listening to the heartbeat using ultrasound. The cause may be inflammatory processes in the mother's body, the presence of infections, late toxicosis, placenta previa or abruption, diabetes mellitus, pyelonephritis, pneumonia, influenza, polyhydramnios or oligohydramnios, intoxication with harmful substances.
Such diagnoses are usually made in the very early stages of pregnancy, which makes it possible to control the process. Thus, there are many chances to maintain the pregnancy and give birth to a child.
Clinical signs of frozen pregnancy
There are a number of sequential disorders characteristic of a non-developing pregnancy : reduction and cessation of uteroplacental circulation against the background of damage to placental structures; cessation of uteroplacental circulation; disruption of the structure of the inner layer of the uterus (endometrium), caused by the presence of dead elements of the fertilized egg in the uterine cavity.
Clinical signs of a non-developing pregnancy can be extremely scarce against the background of a cessation of increase in the size of the uterus and their discrepancy with the gestational age. However, the uterus can be of normal size, it can be reduced, and it can even be enlarged if it is filled with blood due to detachment of the fertilized egg.
For some time after the death of the embryo/fetus, the patient may feel pregnant. However, over time, subjective signs of pregnancy gradually disappear. Spotting bloody discharge from the genital tract and cramping abdominal pain are periodically noted. Chorionic gonadotropin in a woman’s blood, as a rule, is at an extremely low level or even completely absent.
Diagnosis of non-developing pregnancy
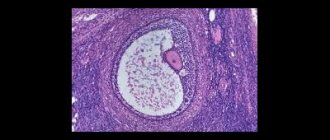
The most reliable way to identify a non-developing pregnancy is by the results of an ultrasound examination in the absence of a fetal heartbeat. One of the most common variants of non-developing pregnancy is anembryonia, i.e. absence of an embryo in the cavity of the ovum after 5-6 weeks of pregnancy. In this case, the fertilized egg is smaller than expected, and the embryo is not visualized.
In other cases of non-developing pregnancy, according to ultrasound examination, the fetal egg is similar in size or lags behind in its development, the embryo can be visualized, but without a heartbeat. Often, a retrochorial hematoma can be detected, which is an accumulation of blood at the site of detachment of the fertilized egg from the uterine wall.
If the dead embryo remains in the uterus for a longer period, visualization of the embryo is impossible; there are no signs of its vital activity. The size of the uterus lags behind the gestational age, and there is a deformation of the fertilized egg with unclear contours.
Sizes by week
Measuring the gestational sac allows you to determine your due date. A value of 5-6 mm corresponds to about 5 weeks of pregnancy. However, thanks to modern transvaginal ultrasound devices, it is possible to detect a fertilized egg even with parameters starting from 1 mm.
The table, which shows the sizes by week, will help you find out about the standards.
At week 6, the parameters are 11 mm in diameter. At 7 weeks the diameter increases to 19 mm, at 8 - 27 mm, 9 - 35 mm, 10 - 44 mm. However, it is impossible to call the correspondence of terms and sizes correct with complete confidence, since the size of the fetal formation may exceed or, conversely, be less than generally accepted norms, and this is completely normal. After all, every woman has her own body characteristics and menstrual cycle. Each embryo is also individual. There are only average values indicating that the size of the fertilized egg should increase by 1 mm per day.
An embryo is considered a fertilized egg only up to 12-14 weeks from conception, since then the next stage of pregnancy begins, when the embryo becomes a fetus.
Removal of a dead ovum
The death of the embryo/fetus is not always accompanied by its spontaneous expulsion from the uterus. There are often cases where a dead fertilized egg lingers in the uterus for an indefinitely long time. The reason for this delay may be: the primary tight attachment of the fertilized egg to the wall of the uterus during implantation, the inferiority of immune rejection reactions of the dead fertilized egg, and a decrease in the contractile activity of the uterus.
When a dead embryo remains in the uterus for more than 4 weeks, elements of the decomposition of the fertilized egg enter the maternal bloodstream, which can cause massive bleeding when attempting to terminate the pregnancy. Therefore, before curettage of the uterus, it is necessary to carry out studies of the state of the blood coagulation system and, if necessary, carry out appropriate treatment.
Advertising
After a thorough examination and appropriate preparation of the woman (carrying out treatment and preventive measures aimed at reducing the risk of developing possible complications), it is necessary to terminate the frozen pregnancy. For this purpose, instrumental or medicinal dilatation of the cervix and instrumental removal of uterine contents are performed. It is also possible to use special medications for non-operative removal of the fertilized egg from the uterus. Immediately during the abortion or immediately after its completion, an ultrasound scan is necessary to ensure complete removal of parts of the fetus and placenta. After removal of the fertilized egg during a non-developing pregnancy, regardless of the chosen method of termination, it is advisable to carry out anti-inflammatory treatment.
In each case, when a pregnancy is not developing, an in-depth examination is required to identify possible causes of termination of pregnancy with their subsequent elimination or weakening of the effect.
Question: Does the gestational age correspond to the size of the fertilized egg?
Hello!
Last month. were from 09/18/13 to 09/21/13, but they arrived with a delay of 10 days. Next month. were supposed to arrive on 10/16/13. They didn’t come, on the 4th day of the delay I took a negative test. Two days later, as expected, I did another test in the morning, it showed a second stripe that was very weak and could only be seen in the light. 11/14/13 According to the obstetrician's calculation, I was 8 weeks into my last menstrual period when I started bleeding in the morning. They did an ultrasound, the size of the gestational sac is 15mm, the embryo is 4.5mm, the uterus puts the term at 4.2 weeks, no heartbeat, it puts Frozen in question. A week later I do a control ultrasound of the fertilized egg, the 19mm embryo has grown to 6.5mm and the heartbeat can be heard. But the doctor said on the ultrasound that the fertilized egg is not growing and puts the term at 5 weeks, but according to obstetrics it should be 9 weeks. Please tell me that the size of my fetal sac really does not correspond and why there is such a difference in terms according to ultrasound and obstetrics. A gestational sac of 19 mm corresponds to a gestational age of 7 weeks, but fluctuations from 5 to 8 weeks are allowed. If there is a suspicion of a frozen pregnancy, it is recommended to test for hCG twice with an interval of 48 hours, which allows you to reliably verify a progressive increase or decrease in this indicator. You can get more information on this issue in the section of our website: HCG analysis. Considering the dynamic growth of the embryo and the detectable heartbeat, a frozen pregnancy is unlikely, so I recommend that you do not panic ahead of time, but undergo a follow-up examination: hCG and dynamic ultrasound.
Hello. My last period was on August 27, 2014. Cycle 30 days. Ovulation occurred on September 12 and on the same day there was sexual intercourse and conception. Subsequently, there were unprotected sexual intercourse, but after B was confirmed. Today, the obstetric period is 5 weeks + 6 days. On an ultrasound with a transvaginal sensor, they did not see an embryo, but a fertilized egg of 13 mm. There is a yolk sac. Is it normal that the embryo is not yet visible? The doctor talks about late ovulation, but sexual intercourse was only on September 12, and the egg lives for a day.
Today, your obstetric gestational age (from the date of your last menstruation) is 6 weeks, and according to ultrasound (gestational age) it is 2 weeks less. As a rule, at a gestational age of 4 weeks the embryo is detected, so in this situation there is a need to exclude anembryonics or a frozen pregnancy. We recommend taking a blood test for hCG at intervals of 48 hours - with normal development of pregnancy, this indicator should increase by 2 times. We also recommend doing a dynamic ultrasound after 5-7 days and personally visiting your gynecologist for an examination.
Based on materials from www.tiensmed.ru
How to reduce the likelihood of embryo death?
To reduce the likelihood of possible damaging factors affecting the course of pregnancy, it is necessary to conduct a screening examination of patients planning a pregnancy, as well as women in the early stages of pregnancy, for urogenital infection. It is also important to conduct medical genetic counseling in order to identify high-risk groups for congenital and hereditary pathologies. If there are endocrine causes of miscarriage, appropriate corrective hormonal therapy should be selected.
It is also important to identify various autoimmune disorders and correct them. Repeated pregnancy is possible if the identified causes of death of the embryo/fetus are eliminated and after the necessary treatment. When pregnancy occurs again, an ultrasound examination is performed to determine markers of possible fetal development disorders in the blood, including: α - fetoprotein, human chorionic gonadotropin, PAPP-A test at the most informative time. According to indications, invasive prenatal diagnostics are also performed, including chorionic villus biopsy, amniocentesis or cordocentesis to determine chromosomal and a number of monogenic diseases of the fetus. In addition, therapeutic and preventive measures are carried out aimed at eliminating the infectious process, specific anti-inflammatory therapy is carried out in combination with immunocorrectors, correction of blood coagulation disorders and prevention of placental insufficiency from 14-16 weeks of pregnancy.