Every woman who is in an “interesting position” feels the joy of upcoming motherhood. However, this condition can be overshadowed by a number of problems. If any alarming signs appear, you need to protect yourself and your unborn baby and consult a doctor.
During pregnancy, the uterus becomes very vulnerable. It naturally changes: it increases in size, its walls thicken. Recent metamorphoses increase the risk of developing hemorrhages, which in medicine are called hematomas.
Hematoma in the uterus is a common pathology, which mainly occurs in the early stages, because it is in the first trimester that the probability of detachment of the ovum is high.
What is retrochorial hematoma?
For some reason, the chorion (future placenta) may begin to partially peel off from the walls of the uterus.
Blood clots accumulate in the resulting cavity - this is a retrochorial hematoma. This pathology is typical for the first half of pregnancy (more precisely, the first trimester), when the placenta is forming.
The danger of pathology, its complications
A uterine hematoma is dangerous if, during an ultrasound examination, it is determined that its volume is more than twenty milliliters, and its area is more than forty percent of the total area occupied by the embryo.
One of the possible serious complications of a hematoma that can develop in the absence of timely treatment is a phenomenon called “Kuveler’s uterus.”
The essence of the pathology is the premature detachment of the placenta with the formation of necrotic foci on it due to the accumulation of blood in the endometrium. “Kuveler's uterus” is considered an indication for surgical intervention to remove the uterus.
A woman who has had a complete resection of the uterus will never be able to bear or give birth to children. There may also be heavy bleeding.
Prognosis for retrochorial hematoma
If the hematoma is large (1/3 of the area of the fetal egg has been exfoliated), retrochorial hematoma is a significant threat and can have an unfavorable outcome:
- oxygen starvation of the unborn child;
- slow development of the baby;
- death of the fetus inside the womb;
- spontaneous termination of pregnancy (miscarriage).
If the pregnancy continues, then the presence of a previously small retrochorial hematoma in most cases does not have a negative impact on the further development of the child.
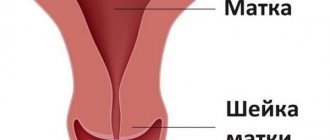
Chorion and placenta
The chorion is the outer membrane of the embryo that forms around the baby in the early stages of its development. Up to 14 weeks, nutrients and oxygen enter the embryo through the chorionic villi, and carbon dioxide is also released. After 14-16 weeks, the function of the chorion is taken over by the placenta (fetal place), which ensures the existence of the fetus until birth.
Normally, there should be no accumulation of blood under the membranes of the chorion or placenta. The appearance of a hematoma is an alarming symptom, indicating a high risk of miscarriage. If you suspect the formation of WG, you should immediately consult a doctor.
Probable Causes
There are many reasons for the occurrence of retrochorial hematoma, and it is not always possible to find out the exact one. The most likely of them are:
- an imbalance in the hormonal system, which leads to the inability of the inner lining of the uterus to normally accept the fertilized egg during the implantation period;
- the presence of chromosomal abnormalities in the fetus (a gene mutation does not allow the “defective” fertilized egg to attach normally to the wall of the uterus, so-called natural selection is triggered);
- increased blood clotting (during implantation, blood clots can form, disrupting both the process of attachment of the fertilized egg to the uterine wall and the nutrition of the fetus);
- severe or chronic stress;
- genital tract infections;
- drinking alcohol, smoking, drug addiction.
Remember that long-term ingestion of infusions, herbal decoctions and herbal remedies that have an abortifacient effect (oregano, marshmallow, aloe, valerian, ginseng, ivy, wormwood, sage, echinacea, etc.) will only worsen the situation!
All the reasons for such a diagnosis are not fully understood in medicine. However, the occurrence of a hematoma during pregnancy is possible for one reason or for several at the same time.
Symptoms of the disease
When the hematoma is located at the fundus of the uterus, there are often no symptoms of pathology (no blood discharge is observed). A pregnant woman does not attach importance to small changes in her state of health and the pathology becomes known only during a routine examination using ultrasound. But more often it happens differently: the woman begins to feel a nagging pain in the lower abdomen, sometimes radiating to the lower back.
If the pathology is established, then bloody, scarlet discharge from the vagina signals a real threat of pregnancy. Scarlet discharge indicates increased growth of the hematoma. Immediate medical attention is needed.
If bright red or scarlet discharge appears, call an ambulance immediately!
When the ovum is detached, a retrochorial hematoma is observed on ultrasound. This condition is a threat of miscarriage. A gynecologist will talk about the causes, signs of a threatened miscarriage (miscarriage) and the rules of behavior for a woman to prevent an undesirable phenomenon in the following video:
Preventive measures
In order for the hematoma to resolve faster, the pregnant woman should lead a healthy lifestyle. Without following the correct regimen, medications will be ineffective. The expectant mother should monitor her moral state, rest, go for walks, and be less nervous. The decision to engage in sexual activity is made by the attending physician. It is necessary to remove foods that cause flatulence from the diet:
- soda;
- cabbage;
- peas, beans, beans;
- tonic drinks;
- Rye bread;
- beet.
This is especially true for women under 12 weeks of pregnancy.
The expectant mother should include the following foods and drinks in her diet:
- fruit salads;
- vegetable soups;
- uzvar;
- fermented milk drinks with low fat content;
- juice from natural fruits.
These products improve digestion.
Diagnostics, tests
Ultrasound examination is the main way to diagnose retrochorial hematoma. With this procedure, you can detect the following signs:
- Local thickening of the uterine wall is evidence of increased uterine tone. With the transabdominal ultrasound method, short-term hypertonicity of the uterus may occur. In this case, you need to repeat the study with a transvaginal sensor. If muscle tone does not stop, this may indicate a threat of spontaneous abortion.
- Due to the tone of the uterus, a changed shape of the fertilized egg is observed.
- Detection of a hematoma, measuring its size and establishing its exact location.
In addition to ultrasound, the following diagnostics are required:
- general blood analysis;
- checking blood for clotting;
- study of vaginal flora;
- analysis for infectious diseases that are sexually transmitted;
- study of hormonal levels (progesterone, testosterone, TSH);
- Carrying out CTG and Dopplerometry of the fetus in the second and third trimester of pregnancy.
Treatment of retrochorial hematoma
A gynecologist treats diseases related to pregnancy, and retrochorial hematoma is no exception. The gynecologist should offer the patient hospitalization, where the treatment process and bed rest will be under strict control. Hospitalization conditions make it possible to stop bleeding in a short time, relieve the tone of the uterus, thereby increasing the chance of maintaining pregnancy.
Treatment of retrochorial hematoma occurs as follows:
- To relieve spasms in the muscle tissue of the uterus, antispasmodics such as drotaverine (no-shpa), papaverine, and magne B6 are prescribed.
- To improve uterine blood circulation, Actovegin is prescribed.
- Dicynon, tranexam - these drugs can be prescribed by a gynecologist to stop internal bleeding .
- Hormonal drugs - utrozhestan, duphaston. These drugs are synthetic analogs of the female hormone progesterone. Under normal conditions, it is produced in sufficient quantities in the body of a pregnant woman. When the level of this hormone is low, the doctor prescribes the medications listed above to maintain the normal course of pregnancy .
Most pregnant women may be intimidated by such a list of medications. But do not worry, the listed drugs are acceptable for use during pregnancy. But taking them on your own is not recommended! Treatment should be selected individually by a specialist and in the right dose.
You should not self-medicate or use folk remedies: not all herbs are harmless during pregnancy, and some can cause irreparable harm to the fetus.
Will a caesarean section be required?
Retrochorial hematoma is an accumulation of blood as a result of detachment of the ovum. It may occur in the first trimester. If the hematoma occurs after 16 weeks, then it is already called retroplacental hematoma.
In most cases, with timely seeking medical help, the hematoma successfully decreases in size and even resolves.
But if the hematoma forms in the second half of pregnancy and, according to the results of studies, the fetus is suffering, a planned cesarean section is performed, which is performed slightly earlier than the planned date of natural birth.
How does a retrochorial hematoma heal?
Brown vaginal discharge indicates that the hematoma has begun to emerge/dissolve. They can be spotting or even moderate.
On average, a hematoma goes away in a few weeks, sometimes the process lasts for a month.
Can a hematoma not come out?
Maybe. The physiological structure of the pelvic organs is such that emptying a retrochorial hematoma in the form of brown discharge is sometimes not possible. The hematoma can be localized high at the fundus of the uterus. In this case, the hematoma does not come out, but slowly resolves.
Lifestyle during hematoma treatment
With retrochorial hematoma, it is important to maintain bed rest and sexual rest. If the pathology is localized at the bottom of the uterus, the legs must be kept above the body position (use the back of a sofa or bed, or place a folded blanket under the legs). This will help empty the hematoma and improve uterine circulation.
Any physical activity, heavy lifting, or sexual activity is strictly prohibited until the diagnosis of “threat of miscarriage” is removed.
The emotional state of a woman is also very important. It is necessary to avoid stressful situations by any means. Sedatives such as novopassit, motherwort tinctures, valerian and others will help maintain a normal psycho-emotional state. But you need to take the drug strictly according to the instructions and not for a long time.
Nutrition
Normal digestion also plays an important role - the intestines should not create pressure on the uterus, this can lead to an increase in the tone of the uterus. Therefore, you need to adjust your diet to avoid constipation and bloating. Eliminate foods that harden stool (including coffee and chocolate). Also, you should not eat legumes and cabbage, so as not to provoke gas formation in the intestines.
Give preference to porridges made from cereals such as buckwheat, oatmeal, etc. Drink more liquid: compotes, water.
Should you worry if you have been diagnosed with retrochorial hematoma? Not only is it not worth it, but it is also strictly contraindicated. Follow the doctor’s instructions, ensure complete rest and comfortable conditions, and adjust your diet.
Prevention
The development of retrochorial formation can be prevented by following the principles of a healthy lifestyle and regularly visiting your doctor. The main preventive measures include:
- Rejection of bad habits. During pregnancy, you should completely stop smoking, drinking alcohol and taking drugs.
- Timely treatment of acute and chronic infectious bacterial or viral diseases. Pathogenic microorganisms can negatively affect the course of pregnancy and the development of the embryo.
- If there is a risk of developing retrochorial pathology, you should strictly follow all the recommendations of the attending physician (bed rest, use of medications, vitamins, refusal of physical activity).
- Compliance with your diet. You should add to the menu dishes rich in vitamins and minerals that stabilize the gastrointestinal tract and cardiovascular system.
- Prevention of injuries, bruises, falls. During the period of bearing a child, it is recommended to abandon physical activity in which there is a high risk of falls (skating, roller skating, skiing), and give preference to quiet walks and swimming.
- Timely registration for pregnancy. Regular visits to antenatal clinics will help identify the onset of pathology in the early stages.