What is the cervix
The cervix is a muscular tube that connects the vagina to the uterus. It has an external and internal os, and a cervical canal.
The cervix is a muscular tube connecting the vagina and uterus
After examining the uterus, the gynecologist can easily characterize the patient’s sex life:
- whether she has ever been pregnant;
- whether she gave birth or had an abortion;
- How soon will she get her period?
Thus, in women who have not given birth, the cervical canal is conventionally a “dot,” and in women who have given birth, it is called a “dash.” If a woman is pregnant, then the appearance of the cervix will help determine the gestational age and assess the risk of miscarriage.
When examining the cervix, the gynecologist can immediately give an opinion about the woman’s sex life
The normal length of the muscular organ in a non-pregnant woman is approximately 3–4 cm, and the width is 2.5–3 cm. The endocervix (cervical canal, the membrane lining the organ from the inside) measures 0.2–0.3 cm. Normally, it is smooth and homogeneous, filled with mucous formations.
Video: structure of the cervix (medical certificate)
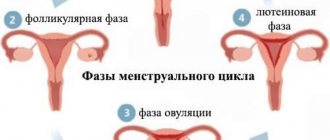
Functional changes during pregnancy
The cervix extends into the vagina. Before pregnancy, this narrow canal remains open and large enough to allow sperm to enter and pass blood during menstruation. From the moment pregnancy begins, the function of the organ is to protect the growing conceptus, so this narrow opening is clogged with mucus, which forms a protective barrier. Effective protection is achieved by maintaining a sufficient length of the closed neck, within which the mucous membrane prevents the penetration of microbes from the lower genital tract by maintaining sufficient strength at the level of the internal pharynx. This prevents the membrane and conceptus from descending through the cervical canal, which can reduce the thickness of the barrier or lead to prolapse of the mucous plug.
During pregnancy, the cervix undergoes great changes, so in the first months of pregnancy it softens, becomes longer, and then shortens, widens, becoming thinner as pregnancy progresses.
How the female organ changes after conception
Nature arranges it this way that during the period of bearing a child, the shape and structure of the cervix gradually changes. This is necessary so that the fetus develops normally until the due date and there is no danger of premature birth. Transformations begin soon after conception. Change:
- color. If in a “non-pregnant” state the cervix is shiny and pinkish in color, then soon after conception the organ swells and acquires a red-blue tint. This is due to intense blood circulation in the genital area, the rapid formation of additional vessels;
- consistency. In a non-pregnant woman it is quite dense (can be compared to the hardness of the nose). For the expectant mother, it is softer to the touch (about like lips);
- location. If during ovulation the “tube” rises, its channel opens slightly to allow sperm to pass through, then when pregnancy occurs, the cervix, due to the action of progesterone, drops much lower than its usual level. However, as the gestational age increases, the organ gradually rises again.
When examined on the chair, the gynecologist sees only the part of the cervix that extends into the vagina. However, this is enough to assess her condition.
Cervical mucus in early pregnancy
Already at the beginning of pregnancy, cervical mucus transforms, becomes thick, viscous and transparent, creating a mucus plug during pregnancy. If the mucus is yellow or green, has an unpleasant odor, and the secretion is accompanied by itching, this may be a symptom of an infectious disease. In this case, you should immediately consult a doctor.
Norms for the condition of the cervix during pregnancy
The doctor examines the cervix of the expectant mother using various methods. He evaluates the size and density of this organ.
Table: normal cervical sizes corresponding to gestational age
| weeks | Average length, mm | Normal range, mm |
| 10–14 | 35,5 | 28–45 |
| 15–19 | 38,5 | 30–48 |
| 20–24 | 40 | 32–48 |
| 25–29 | 41 | 34–49 |
| 30–34 | 37 | 34–43 |
| 35–40 | 29 | 20–37 |
Thus, until a certain period of gestation, the length of the cervix increases, then its stable and gradual decrease begins. It is important that the standard length for each term is not a specific value, but a range. In addition, deviations from the specified parameters are allowed: if they are 4–4.5 mm in one direction or another, then the patient should not worry too much.
These changes in the size of the cervix are characteristic primarily of the first pregnancy. If a woman has already given birth, then the length of the muscle “tube” will increase at a faster pace. For example, at 10–14 weeks it will be an average of 36.5 mm.
As for other parameters of the cervix when carrying a child, before the 32nd week of pregnancy it is normally slightly tilted back, the cervical canal is tightly closed, and it is very difficult (almost impossible) for the doctor to insert a finger into it. The entrance to the uterus is blocked by a special mucus plug that prevents infection. If there is a threat of miscarriage, then the tissue of the organ will be loose to the touch, and the internal pharynx will be more or less open. In this case, the woman is admitted to hospital to take measures to maintain the pregnancy.
A too rigid cervix may be a sign of uterine tone, which is dangerous for premature birth.
In the third trimester of pregnancy, based on an examination of the cervix, the gynecologist already assesses the body’s readiness for childbirth: the organ becomes softer, the internal os gradually expands (direct dilatation occurs during contractions).
In the third trimester (from the 32nd week), a special scoring scale is used: it assesses the maturity of the cervix (its readiness for childbirth). Each indicator is characterized by 0–2 points. The greater the total amount, the correspondingly more mature the organ.
Table: cervical maturity scale
| Indicator, points | Consistency | Length, mm | Position | Opening degree |
| 0 | Quite dense | Over 20 | Leaned back | The finger does not pass into the cervical canal |
| 1 | Slightly softened | 10–20 | Tilt forward | Only one finger goes through |
| 2 | Soft | Less than 10 | Located centrally relative to the wire axis of the pelvis | Passes more than two fingers |
The cervix finally ripens at the 37th week of gestation. This is facilitated by the fruit, which presses on it with its mass.
Gradual changes in the uterus
The enlargement of the organ occurs gradually, which allows the female body to adapt to the new reality. The growing fetus compresses the surrounding tissues, forcing you to change your usual lifestyle.
Lifting the uterus into the abdominal cavity
Each stage of development is accompanied by conventional boundaries:
- Week 8. The uterus increases to twice its original size, but obvious visual changes are not yet observed.
- Week 12. The uterus protrudes above the symphysis pubis; this is the peak period of pregnancy toxicosis.
- Week 14 The organ increases to 12 cm, the first movement is felt.
- Week 16 The size of the organ is 14–15 cm. All vital structures of the embryo are fully formed. The upper border of the uterus can be felt in the midline between the womb and the umbilical fossa.
- Week 18. The organ increases to 18–19 cm and moves closer to the umbilical cavity.
- From 20 weeks, the height of the uterine fundus is set at 20 cm and increases by a centimeter every subsequent week.
After 36 weeks, the size of the organ changes slightly - 5-2 mm per week.
At what time can you palpate the uterus?
A woman can independently determine the boundary at about 12 weeks. It will be felt as a small painless lump above the symphysis pubis. In the presence of pathologies (fibroids, fibroids), the organ enlarges faster. During multiple pregnancies, the size of the uterus increases at a faster rate.
Table of norms for the cervix
Not only the uterine cavity, but also the cervix undergoes changes. From the moment of conception, it lengthens, softens, and changes color. Its length reaches 4.0–4.5 cm. Subsequently, a gradual shortening of the canal is noted.
The following parameters indicate the successful development of pregnancy.
Important! Rapid shortening of the cervix is a threat to full pregnancy. Such progress is especially dangerous for a period of up to 34 weeks.
Table of norms of UMR - fundal height of the uterus
Fundal height of the uterus is measured weekly, starting at 14 weeks. The data is recorded in the patient’s individual table to monitor the dynamics. A physiologically normal pregnancy corresponds to the following indicators.
At week 38, the height of the uterine fundus is no more than 32 cm, and the fetus descends into the pelvic cavity.
What affects VDM
All described sizes vary within 2–3 cm and depend on many factors:
- Genetically determined embryo weight. A large fruit adds several centimeters, but the positive dynamics remain.
- Position of the fetus in the cavity. With longitudinal presentation, the height of the fundus is less than with transverse presentation.
- Pelvis width. With a narrow pelvis, the uterus is located higher.
- The amount of amniotic fluid. Polyhydramnios increases the volume and size of the organ.
- Frozen pregnancy, in which there is a lack of dynamics.
- Several embryos.
Toxicosis, the occurrence of infectious diseases, and low weight gain play a negative role.
How does multiple pregnancy affect
During a multiple pregnancy, the abdomen grows rapidly; it can protrude above the symphysis pubis as early as 10–11 weeks. When measuring VMR, the parameters have a gap of 5–7 cm. By the peak indicator (36–38 weeks), the upper limit is at a distance of 42–48 cm above the symphysis pubis.
The stretching of muscle fibers and skin is much stronger, and labor occurs earlier - at 36–37 weeks. With multiple pregnancies, the cervix becomes shorter and denser. And its physiological shortening occurs more quickly.
Methods for studying the length of the cervix in a pregnant woman
The gynecologist evaluates the condition of the cervix during regular examinations (at least once a month). In this case, mirrors and two-handed examination are used. The cervix is examined especially carefully at the 20th, 28th, 32nd and 36th weeks of pregnancy.
When there is a risk of miscarriage or other problems, visits to the gynecologist should be more frequent.
During the examination, in addition to visually examining the cervix, the doctor periodically collects material. This allows us to exclude a potential inflammatory process and emerging cancers.
At each routine examination, the gynecologist also evaluates the condition of the cervix
In addition, the doctor periodically directs the patient to undergo testing for sexually transmitted infections (STIs). This is necessary to ensure the absence of pathogenic microorganisms (chlamydia, mycoplasma, etc.) that can harm the fetus and affect the cervix.
Testing for sexually transmitted infections is carried out twice during pregnancy (in the 1st and 3rd trimester), but if problems are identified, the examination will have to be repeated more often.
Sexually transmitted infections can affect the condition of the cervix.
The most reliable method for determining the length of the cervix is ultrasound. This study is the most informative for determining the threat of premature birth. In addition, when it is carried out, the structure of the muscle “tube” is assessed (homogeneity, absence of pathological formations).
Typically, during pregnancy, an abdominal ultrasound is used (the sensor moves along the surface of the abdomen). However, if the doctor suspects a problem (the cervix is shortened), he will most likely recheck this through a transvaginal test, during which a sensor is inserted into the vagina.
Using ultrasound, the exact length of the cervix is determined
Pathological disclosure
Signs of cervical dilatation during pregnancy before the onset of labor are considered pathological and may occur due to:
- hormonal deficiency;
- inflammation of the genital organs;
- frequent abortions or miscarriages in history;
- injuries that occurred during previous births;
- erosion;
- acute infectious process;
- placental abruption.
At a period of 28 weeks or more, this phenomenon can result in premature birth, and in the early stages - spontaneous miscarriage. If you experience pain in the lower abdomen, you should consult a doctor. If early dilatation is confirmed, the woman is recommended to have bed rest, use hormone replacement therapy, and suture the pharynx area until the normal delivery date.
Insufficient cervical length
Marked shortening of the cervix (when its length is less than 2.5 cm long before birth) is a serious signal that can put pregnancy at risk. After all, this phenomenon often leads to isthmic-cervical insufficiency - premature dilatation of the cervix in response to increasing load.
Shortening of the cervix is a serious problem that jeopardizes the continuation of pregnancy
Shortening of the cervix can be caused by a number of reasons:
- an innate feature of the female body;
- hormonal disorders: lack of progesterone and increased production of androgens (testosterone derivatives). The problem is especially aggravated from the 16th to the 26th week of pregnancy, when the fetal adrenal glands additionally begin to produce androgens;
- previous injuries. For example, forced dilation of the cervix during abortion or research, violation of the integrity of the muscles of this organ during previous natural births. Muscles can be partially replaced by connective tissue, which prevents the “tube” from fully stretching and contracting;
- in the past - three natural births or more (with each subsequent pregnancy, the likelihood of shortening the cervix increases);
- sexually transmitted infections;
- large size of the fetus, which puts too much pressure on the cervix;
- multiple births;
- abnormal amount of amniotic fluid: polyhydramnios or oligohydramnios;
- uterine bleeding.
One of the reasons for the shortening of the cervix is trauma suffered in the past, provoked by a surgical abortion, in which the cervix is forcibly dilated with instruments.
The danger of a shortened cervix is that under the pressure of the weight of the fetus, it can open at any time. Moreover, the tone of the uterus sometimes remains normal, and in general the woman often does not feel any alarming symptoms (sometimes there is a nagging pain in the lower abdomen and an admixture of blood in natural discharge). If the expectant mother neglects to regularly visit the doctor, she may find out about the problem already during premature birth. In addition, when the pharynx of a short “tube” is further deformed, infection can enter it, and during childbirth there is a risk of organ rupture.
A short cervix can dilate at any time, causing premature labor.
If the gynecologist has detected a shortened cervix, then the expectant mother should be closely monitored. She is ordered to rest completely. If the pathology is caused by a hormonal factor, then appropriate medications are prescribed.
Sometimes an obstetric pessary or a special ring is placed on the cervix: it reduces the load on the organ. In serious cases, when the risk is very high, sutures are placed on the organ, which are removed only before childbirth.
To prevent a short cervix from dilating prematurely, a ring (obstetric pessary) can be placed on it.
Of course, there are cases when patients with a short cervix, without any medical measures, safely carry a child until birth. However, it is better not to take risks and strictly follow medical recommendations.
So, one of my colleagues suffered from isthmic-cervical insufficiency during pregnancy, and she had stitches on her cervix. When they were removed shortly before the PDR, labor began literally immediately: the short and weak cervix could not hold the fetus at all. During her second pregnancy, the same woman was fitted with an obstetric pessary at the beginning of the second trimester, as the problem remained relevant.
To prevent shortening of the cervix, every woman should:
- avoid abortion;
- give up bad habits (for example, smoking, which provokes hormonal imbalances);
- avoid significant physical exertion and nervous shock.
Isthmic-cervical insufficiency
Not only the condition of the uterus can be dangerous when it exceeds normal levels.
A fairly short cervix also poses a threat to the baby. The degree of threat is determined by the results of ultrasound. The condition of the uterus is considered dangerous when the length of the cervical canal is 3 cm. The diagnosis of isthmic-cervical insufficiency is established when the indicator is 2 cm. The soft and very small cervix is not able to withstand the weight of the baby, and as it grows, the surface of the amniotic sac begins to disturb and the infection gets inside. In cases where the external pharynx opens quickly, this can cause prolapse of the fertilized egg.
But thanks to modern medicine, even with this diagnosis established, it is possible to carry and give birth to a healthy baby. Depending on how short the cervix is, surgical intervention is prescribed in which sutures are applied. This helps keep the organ closed.
In some cases, a gynecological pessary is installed. This is a special design consisting of a plastic or silicone ring. The pessary helps distribute the load and acts as a bandage. The structure or sutures are removed immediately before birth.
The cervix is an important organ that facilitates the fertilization process. In addition, it helps prevent infection from entering the appendages and uterus. It is the cervix that plays a major role in inflammation during pregnancy. Based on the changes that occur during fetal development, the doctor determines the risk of miscarriage or premature birth. It is for this reason that it is important to monitor the condition of the organ, especially during pregnancy.
Elongated cervix
Another anomaly in the size of the cervix is much less common - its elongation (more than 4 cm shortly before birth). The following reasons can provoke it:
- a congenital feature of a woman’s body;
- frequent inflammation in the genital area;
- injuries from previous births;
- surgical intervention.
An elongated cervix can also create certain problems when carrying a baby:
- disrupt the anatomy of the uterine os, which can lead to improper attachment of the placenta;
- mature for childbirth for too long due to its dense structure, as a result of which it can provoke post-maturity;
- lead to prolonged contractions (over 14 hours), physically exhausting the woman and leading to weak labor. Usually in such cases stimulation is used, and if it does not help, a caesarean section is prescribed.
An expectant mother with an elongated cervix at the end of the third trimester of pregnancy is recommended to have an active sex life (prostaglandins contained in male sperm help soften the cervix). It is also worth adjusting your diet - include fatty sea fish and salads seasoned with vegetable oils. The softening of the cervix is facilitated by the dietary supplement "Primrose Oil", containing prostaglandins, for oral (inside) and vaginal (in consultation with your doctor) use.
Prevention of cervical elongation should be carried out even before pregnancy. It is necessary to heal inflammation of the genital area and avoid abortion.
Impact of dysfunction on pregnancy
If the cervix contracts (shrinks) and opens (dilates) before your baby reaches full term, it may indicate cervical insufficiency, which leads to preterm labor. This can happen during the 2nd trimester or early 3rd trimester of pregnancy. As the fetus grows, its weight puts more pressure on the cervix; if it is soft, weak, or abnormally short, labor may begin even if there are no contractions or symptoms of labor onset.
How to deal with cervical insufficiency
A weak or dysfunctional cervix may undergo a surgical procedure called cerclage, which places stitches around the cervix to help keep it closed and strengthen it. This is usually done between 14 and 16 weeks of pregnancy. Stitches are removed at 37 weeks to avoid problems during childbirth. The procedure does not lead to spontaneous labor or miscarriage.
Scraping is not done if:
- the cervix is irritated or inflamed;
- the cervix is dilated to 4 cm;
- membranes are ruptured.
Cervical cerclage may have some complications, which include uterine rupture, bleeding and hemorrhage, bladder rupture, deep cervical tears, premature rupture of membranes, and preterm labor. However, despite the minimal potential for complications, most doctors believe that cerclage is a life-saving treatment that is worth the risks. It is the doctor's responsibility to explain the risks and benefits of treatment.
Other treatments include the use of the hormone progesterone or a pessary (silicone device) placed around the cervix to prevent preterm labor.
Attention! Frequent, regular uterine contractions, vaginal spotting, pelvic pressure and persistent back pain are signs of preterm labor.
Other pathologies of the cervix
The cervix may not only have an abnormal length, but also be affected by various diseases. Some of them negatively affect the course of pregnancy.
Table: pathologies of the cervix not related to its length
| Pathology | Symptoms | Causes | Danger | What to do |
| Endocervicitis, which is caused by infections (for example, staphylococci and streptococci, mycoplasma and chlamydia, etc.) |
| Unprotected sexual intercourse, visiting public places (bathhouse, swimming pool, gym, etc.) | If left untreated, bacteria can:
| Immediate antibacterial treatment |
| Cervical erosion is damage to the mucous membrane (upper epithelial layer) in the form of a red spot. If there is a problem, there is no degeneration of cells; their structure remains normal. | Most often, it does not manifest itself at all, and the doctor records the erosion when examining the pregnant woman. However, sometimes there is bloody discharge from the genital tract and pain during intercourse. |
| Does not cause complications during pregnancy and childbirth | They treat (most often cauterize) after childbirth, since this can cause a scar to form that prevents the opening of the cervix. In addition, in some women, the pathology goes away on its own. However, in rare cases, therapy is necessary - if the affected area is too large and there are pathological changes. |
| Cervical dysplasia is the replacement of its epithelium with an atypical one. As a result, the mucous membrane thickens and ceases to function normally (unlike erosion, the damage is more profound). | It does not manifest itself in any way and does not bring significant discomfort to the woman, although yellowish discharge (similar to ichor) or bloody discharge after intimacy is sometimes possible. The doctor records the pathology during examination. |
| It does not directly affect pregnancy, but it can progress (30% of cases), and there is a danger of degeneration into oncology. Although sometimes there are cases of spontaneous disappearance of dysplasia during pregnancy (25%). | It cannot be treated during pregnancy, as this can lead to cervical injury and scarring. In addition, there may be a risk of premature birth. A severe form of dysplasia sometimes requires termination of pregnancy. |
In what cases does disclosure occur?
Fine
The opening of the cervix during pregnancy under normal conditions is a sign of the onset of labor. This parameter is measured in the number of fingers the obstetrician misses. Full expansion occurs at 10 cm, which corresponds to five fingers.
The first symptoms of cervical dilatation during pregnancy are as follows:
- Severe pain occurs, to some extent reminiscent of that during menstruation, but over time it tends to increase.
- The pain is characterized by the fact that it is regular and cramping in nature and occurs at strictly defined intervals. Initially - after 20-30 minutes, and then the time decreases on average from 5 to 7 minutes. During labor, the degree of dilation is checked every three hours.
- A mucous-bloody plug comes off, which is present throughout the entire period of gestation; its function is to prevent infection from entering the uterine cavity.
Functions of the uterine cervix
The cervix plays an extremely important role in the female reproductive system. The main purpose of this organ is to securely hold the baby in the mother’s stomach. This allows the fetus to fully develop. If the uterine cervix opens prematurely, this can pose a serious danger to the child - termination of pregnancy or severe developmental pathologies.
What functions does the cervix perform?
- The cervix produces a special secretion - a mucous substance, which serves to reliably protect the uterus from the penetration of various pathogens and bacteria.
- Holding and protecting the child in the mother's womb - the pharynx must have the required length; a small and short neck is not able to fully perform its protective function.
In non-pregnant women, the cervix is hard, dense and elastic; just before childbirth, it becomes soft and loose. In the early stages of pregnancy, the reproductive organ significantly increases in size - this occurs due to the rapid growth of mucous and muscle tissues.
This process also affects the color of the organ. It acquires a more saturated, lilac-bluish hue. This occurs due to increased blood circulation in the cavity of the reproductive organs.
Inflammation of the cervical canal
Inflammation in the external pharynx can be caused by infectious and non-infectious causes. It can occur with gonococci, streptococci, E. coli, chlamydia, herpes viruses, candida and papillomas.
Non-infectious causes of inflammation may include the following:
- erosive lesions;
- traumatic injuries;
- neoplasms;
- cervical prolapse.
It is worth noting! Doctors, in order to accurately establish the cause of the development of the inflammatory process in the cervix, prescribe the necessary examination. Scraping is mandatory.
Typically, inflammation in the cervical canal is detected during initial diagnosis. The examination reveals redness, swelling, and purulent discharge.
To identify the pathogen, it is necessary to submit material for examination, namely a smear and bacteriological culture of the secretions. After this, a study is carried out that will help identify sexually transmitted infections.
How does the cervix feel in early pregnancy?
During early pregnancy, the cervix becomes soft and rises. The feeling of softness occurs because during pregnancy the organ contains more blood due to the increase in estrogen levels in the woman's body.
How to check your cervical position yourself
First you need to find the cervix: it is located about 8 - 15 cm inside the vagina, feeling like a small donut with a tiny hole in the center. Before looking for the cervix, you should wash your hands thoroughly with soap to avoid introducing bacteria. It must be remembered that long nails can injure internal organs. Having assumed a sitting squatting position, you should place the longest finger into the vagina a few centimeters.