Streptoderma in children
If treatment is not started in time, the ulcer reaches a large size, and multiple lesions form around it on the skin, thus large areas of the skin can be affected.
This disease is called streptoderma or pyoderma
It can develop in any person from birth to old age. But children suffer from it much more often, because... their skin is delicate, their immunity is not sufficiently developed, minor skin injuries in children occur more often and are more likely to become infected.
More often than others, children with allergic skin diseases (scratching itchy skin) suffer from streptoderma.
The favorite localization of the lesion is exposed skin: face, arms, legs.
In infants, streptoderma often occurs in the perineum, as a result of prolonged exposure to dirty and wet diapers. With the use of diapers in infants, it began to occur less frequently.
Streptoderma is contagious. It can be transmitted from one child to another through close contact; in addition, strepococcus or staphylococcus, which is its cause, can cause sore throat, pharyngitis, stomatitis, otitis media and other diseases in children. Therefore, streptoderma is a contraindication for a child to attend kindergarten.
Having noticed a sore on the child’s skin, parents, as a rule, think that it is not scary and try to get rid of it on their own. Usually this fails.
Symptoms of the disease
The disease has many different types, the main differences being the location on the body and the shape of the rash.
However, all types of streptoderma have similar clinical symptoms, caused by one pathogen and a toxic effect on the baby’s body.
The various stages of streptoderma in children (bullous and non-bulous) depend on the time the pathological agent is in the child’s body, manifesting itself first by an increase in symptoms, and then by a gradual decrease.
Common symptoms include:
- The appearance of a fever in a child - the temperature of the food reaches high levels and can reach 39 ° C;
- Rashes on the body with purulent foci;
- After a few days, the rashes burst and redness with a yellow crust remains in place, which disappears after a few more days;
- Rashes on the body are accompanied by unbearable itching and often the child scratches the redness until ulcers appear, which also aggravates the process.
Causes of scrofula in children: signs, main symptoms, diagnosis and treatment (105 photos)- Fenistil for newborns - when it is prescribed, for whom it is contraindicated and when to use the drug (125 photos)
The first symptoms of cough in infants - causes, types, features and tips on how to treat coughs and colds (125 photos)
Depending on the type of streptoderma, the pathological agent can be located in different parts of the body.
The total duration of the disease can range from 3 days to 4 weeks - it depends on the state of immunity and on how much the pathological agent spreads throughout the body.
Symptoms of streptoderma in children can be aggravated if treatment is not started in a timely manner.
If the process of the appearance of ulcers is started, then a chronic form of pathology may appear, which is characterized by a severe course and the constant presence of large areas of lesions on the child’s skin.
Treatment of Streptoderma in children
Meanwhile, streptoderma can be treated very well if treatment is started at the very beginning. At this time, the child’s well-being does not suffer. Usually, it is done without taking medications orally.
Therefore, the sooner you see a doctor, the better. First, contact your pediatrician; if necessary, he will refer you to a dermatologist.
The treatment plan is very simple
Do not wet
If necessary, you can gently wipe the skin around with a damp cloth or cotton wool moistened with 70° alcohol without affecting the focus of streptoderma.
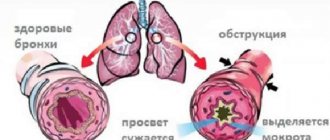
Streptococci and staphylococci love moisture and actively multiply in its presence. On dry skin they stop multiplying. Thus, without moisturizing the skin, we prevent the spread of pathogens beyond the affected area.
It is recommended to treat streptoderma lesions with brilliant green (an alcohol solution of brilliant green) once a day - in the morning, and then leave the affected area of skin open (do not cover it with a bandage).
Zelenka has a disinfecting and drying effect.
Antibacterial ointment
There is no way to do without this point. And those who love all sorts of lotions and powders with herbs can do a lot of harm to the child.
It is recommended to apply a bandage to the affected area with one of the antibacterial ointments: levomikol, gentamicin, syntomycin - once a day - at night. In this case, a bandage is needed for longer and closer contact of the ointment with the focus of streptoderma. In the morning, the bandage is removed - the affected area is treated with brilliant green and left open.
Ointments containing hormonal drugs: triderm, celestoderm - give a good effect, but they are strictly not recommended to be used independently, without a doctor’s prescription, because When applied to a large area of skin, they can affect the body systemically (through the bloodstream).
Constantly wearing a bandage is not acceptable, because... At the same time, the skin becomes moisturized and warmed up, which can lead to the opposite result.
Treatment usually lasts 7-10 days and leads to complete recovery.
If there are multiple foci of streptoderma, spreading over large areas of the skin - this disrupts the general condition of the child, the temperature rises, the lymph nodes enlarge - this will require systemic use of antibiotics: in tablets, intramuscularly or even intravenously with hospitalization in a hospital.
But such a lesion does not occur instantly; streptoderma always develops gradually. So parents always have time to see a doctor. Streptoderma in children. Treatment.
- Molluscum contagiosum in childrenWhat is molluscum contagiosum in children? Molluscum contagiosum is what it is.
- Scabies in children Quarantine TreatmentWhat is scabies in children? Scabies is a parasitic disease.
- Anemia in children TreatmentAnemia in children in most cases turns out to be iron deficiency and is caused by.
- Runny nose in children Treatment First remedies for a runny nose Runny nose in children causes Runny nose or rhinitis occurs in children.
- Pediculosis in a child Treatment Pediculosis in a child is a parasitic disease of human skin and hair that.
Ulcers on your child’s body can appear for various reasons, but often we are talking about skin damage by streptococci - anaerobic parasitic bacteria that live not only in humans, but also in animals. We will tell you below how to recognize a dangerous infection and cure it. This information will be especially important for parents, since children are the first to be hit.
Methods for diagnosing the disease
To successfully treat the fungus, the patient needs to consult a doctor - he will conduct a visual examination, carefully examining the lesions. Laboratory tests will help determine the type of pathogen.
- Bakposev - the collected biological material is placed in a nutrient medium. If the scraping contains pathogenic microorganisms and growing fungal colonies, the preliminary diagnosis is confirmed.
- Enzyme immunoassay - blood is taken from the patient’s vein to detect antibodies to a specific pathogen.
- Microscopy – the sample taken is processed with special preparations and examined under a microscope.
- Polymerase chain reaction - allows you to determine the type of fungus by identifying the DNA of the pathogen. To conduct the study, a scraping from the affected area is required.
The child has ulcers on his body
The main symptom of the disease is the formation of purulent blisters (phlycten) on the skin, which have a round shape and sometimes a flaky surface. Their number, size and areas of distribution depend on the clinical picture; in one patient they may appear on the extremities in separate formations, in another as a small rash in the lower part of the body. However, in any case, they will contain a cloudy white-honey liquid.
Streptococcal flora is considered conditionally dangerous, since it is often present in the body and does not cause harm. But any weakening of health and bacteria begin to multiply, no longer contained by the immune system:
- Hypothermia;
- Poor nutrition;
- Lack of sleep.
Their waste products enter the bloodstream, poisoning the body.
Causes of streptoderma
The main cause of the pathology is streptococcus, which entered the child’s body through areas of damaged skin on the baby’s body.
The infection does not enter the body on its own; many factors contribute to this, such as:
- Weakened immune system of the child;
- Damage to the baby's skin;
- Violation of child hygiene;
- Pathologies in the endocrine system (rare);
- Sudden changes in climatic and temperature conditions of the child’s stay;
- Burn wounds;
- Some diseases - anemia, malnutrition, worms;
- Contact with water for a long time.
It is important to note that a pathology such as streptoderma is seasonal, most often appearing in summer and late spring. This is due not only to the stability of temperatures, but also to the fact that the child is currently more susceptible to the influence of external agents.
Many people are concerned about the question: is childhood streptoderma really contagious? The answer to this question is yes.
When do the first teeth appear in babies: when do they appear, the first symptoms and the order of teething (95 photos and videos)Do children need ergoferon and why - instructions for use, recommendations and reviews from doctors (95 photos and videos)
Why there might be a bump on a child’s head: what to do and how to treat it quickly and easily. Modern and traditional methods of getting rid of cones (105 photos and videos)
This statement can be confirmed by the presence of outbreaks of the epidemic in preschool and school institutions. One sick child or carrier causes illness in many other children.
How can you get infected?
So, for the infection to begin to spread in the body, the immune system must be weakened, and it is easy to become infected:
- By airborne droplets. Staying in crowded places, especially in poorly ventilated areas (offices, public transport, schools), increases the chance of infection. People who sneeze and cough are a direct source of streptococcus, especially if you are nearby in a stuffy room, when the concentration of bacteria increases;
- Household - when you share the same dishes and bed linen with someone. Through microtraumas of the skin (and almost everyone has them) or the mucous membranes of the oral cavity, bacteria can easily enter the body if you finished your tea with a friend who was visiting you;
- Sexual – during intimate intimacy, since these microorganisms are also found in the organs of the reproductive system of men and women;
- Nutritional – failure to comply with the simplest rules of hygiene;
- Medical - during examination with a non-disinfected instrument.
Children are more likely to come under attack, since their immune system is less perfect than that of an adult, and the concentration of bacteria in organized children's groups is extremely high (kindergarten, school, hobby groups).
What is streptoderma?
Childhood streptoderma is a purulent skin disease of an infectious nature.
The pathology is characterized by purulent rashes on the baby’s body, which causes discomfort and can lead to infection of the child’s blood. Photos of streptoderma in a child can be found freely available on the Internet.
Streptoderma is bacterial in nature - the main causative agent of the disease is streptococcus. This pathology is also called streptococcal pyoderma.
The sources of infection are most often patients with streptoderma and carriers. However, the disease can be transmitted to a child through household items, toys, or if the baby has lesions on the skin.
Streptoderma is transmitted through contact and household contact. There are known cases of transmission of the pathogen by airborne droplets, when the pathogen came into contact with the baby’s damaged skin as a result of coughing or sneezing of a patient or carrier of the infection.
Other symptoms of pyoderma
In addition to skin ulcers, pyoderma is characterized by the following manifestations:
- Skin itching, sometimes severe, more like a burning sensation;
- Formation of pigment spots at the site of healing lesions;
- Lack of appetite;
- Superficial peeling in the affected area;
- Sometimes – enlarged lymph nodes;
- Rarely – elevated temperature.
Like any disease, pyoderma has an incubation period; the clinical picture begins to develop approximately 7 days after infection, and it is after this that rashes appear.
Streptoderma is often confused with other skin pathologies - eczema, urticaria, lichen, so doctors sometimes prescribe ineffective treatment, especially at the initial stage.
Why is pyoderma dangerous?
If treated incorrectly, there is a possibility of developing a chronic form with a relapsing course. In this case, the ulcers merge into single lesions, which are spots with flaking dead skin.
When the disease calms down, the appearance of new blisters stops, but the previously affected areas continue to peel off, becoming covered with scales.
The prolonged existence of the lesion leads to increased sensitivity of the skin; now any living organisms can harm the epidermis in the affected areas. This process leads to microbial eczema with the appearance of eczematous wells.
Often the raised rash is covered with drops of serous fluid, which prevents the sores from healing.
Among other things, streptoderma can lead to the following complications:
- Purulent otitis;
- Rheumatism;
- Vasculitis;
- Chronic lymphadenitis;
- Sepsis;
- Erysipelas.
There are known cases of the development of more severe diseases - heart defects, kidney pathologies.
Therefore, it is extremely important to treat the disease correctly and not self-medicate.
How to treat streptoderma?
What treatment will be depends on the clinical manifestations:
- If isolated sores appear and there are no signs of poisoning of the body, it is possible to get by with local therapy - the purulent blisters are opened, treated with brilliant green, and a dry bandage is applied on top. The crusts are treated with salicylic petroleum jelly and removed;
- For more common forms, antibiotics are prescribed internally (Amoxicillin, Sumamed, Amoxiclav) and antibacterial pastes externally (erythromycin, linuomycin);
- When the patient experiences severe itching, antihistamines are recommended;
- To prevent the disease from spreading when scratching, the nails are lubricated with brilliant green.
In addition, it is advisable to put the patient on a diet in which he will not eat sweet and spicy foods, as they provoke the secretion of serous fluid. Also, additional vitamin therapy to strengthen the immune system will not be superfluous.
So, if you find ulcers on a child’s body and they are purulent-serous in nature, it may be an infection with streptococcus.
Video about baby rashes and skin ulcers
In this video, pediatrician Komarovsky will talk about the causes of rashes and sores on the skin of babies and how to get rid of them:
Help get rid of strange sores on the skin just above the knees. For several years now, the sores on the skin just above the knees have not gone away. I contacted specialists. Scraping and tests revealed nothing. Doctors shrug their shoulders. The sores, the size of a ten-kopeck coin, are located symmetrically on both legs just above the knees. Brown heels are peeling, the skin in these places is wrinkled. Sometimes they hurt, itch, sting. They get worse when I wear synthetic clothes. What could it be? And most importantly, how to get it out?
Woman.ru experts
Find out the opinion of an expert on your topic
Alena Selezneva
Psychologist, Online consultant. Specialist from the site b17.ru
Bondarenko Tatyana Alekseevna
Psychologist, Candidate of Psychological Sciences. Specialist from the site b17.ru
Sakharchuk Svetlana Alexandrovna
Psychologist, Psychologist - consultant. Specialist from the site b17.ru
Neshchadim Dmitry Vladimirovich
Psychologist, Medical clinical psychologist. Specialist from the site b17.ru
Muratova Anna Eduardovna
Psychologist, Online consultant. Specialist from the site b17.ru
Tankova Oksana Vladimirovna
Psychologist, Online consultant. Specialist from the site b17.ru
Natalya Evgenievna Pokhodilova
Psychologist, Kinesiologist Online consultant. Specialist from the site b17.ru
Elena Barkhatova
Psychologist, Consultant. Specialist from the site b17.ru
Irina Viktorovna Baranova
Psychologist. Specialist from the site b17.ru
Yulia Bugrova
Psychologist, Existential approach. Specialist from the site b17.ru
maybe some kind of allergic dermatitis, think about when there is an aggravation, maybe even food-related, you have to think, go to an allergist
maybe some kind of allergic dermatitis, think about when there is an aggravation, maybe even food-related, you have to think, go to an allergist
I had a similar thing on my chin a few years ago. At first I waited for it to go away on its own, after 4 months I got tired of it and went to a dermatologist, who suggested that it was an allergy - but why, I had never been an allergy sufferer and at that time I didn’t eat anything new and didn’t buy any cosmetics or household chemicals! But it turned out to be hormonal, and it suddenly went away within six months as soon as I solved my seemingly unrelated problems like a woman!
Well, there’s a lot of information at once: there could be allergies and hormonal imbalances. Yes, I have big problems with hormonal disorders and women’s issues. What about our skin workers: if only there was no Venus.
allergy 100%. It went away for me at sea, but now it’s showing up again (((I’m all stressed
Well, yes, nothing was sown - a defect in the choice of environments; there is nothing under the microscope - a defect in the choice of dye; Alternatively, the body has already chewed all the microbes. If dyshormonosis played a significant role, these coins would be everywhere - under a belt, under shoes, a hat, a vest, a mobile phone, etc. This area can be rubbed by a laptop, a sexual partner, a steering wheel, and not just a skirt. In general, a vitaminograph-ferrograph, etc. There are very useful units in the hall.
Related topics
Homeopathy would probably help you.
Maybe it’s something mechanical, for example, you often bump into these places against the bathtub?
Maybe it’s something mechanical, for example, you often bump into these places against the bathtub?
Hello, I have an incomprehensible sore on my leg, it’s round like a double ring, it itches, if anyone knows, please tell me
Forum: health
New for today
Popular today
The user of the Woman.ru website understands and accepts that he is fully responsible for all materials partially or fully published by him using the Woman.ru service. The user of the Woman.ru website guarantees that the placement of materials submitted by him does not violate the rights of third parties (including, but not limited to copyrights), and does not damage their honor and dignity. The user of the Woman.ru site, by sending materials, is thereby interested in their publication on the site and expresses his consent to their further use by the editors of the Woman.ru site.
Use and reprinting of printed materials from the woman.ru website is possible only with an active link to the resource. The use of photographic materials is permitted only with the written consent of the site administration.
Posting intellectual property objects (photos, videos, literary works, trademarks, etc.) on the woman.ru website is permitted only to persons who have all the necessary rights for such posting.
Copyright (c) 2016-2018 Hirst Shkulev Publishing LLC
Online publication “WOMAN.RU” (Zhenshchina.RU)
Certificate of registration of mass media EL No. FS77-65950, issued by the Federal Service for Supervision of Communications, Information Technologies and Mass Communications (Roskomnadzor) on June 10, 2016. 16+
Founder: Limited Liability Company "Hirst Shkulev Publishing"
Skin diseases in children can be contagious or non-contagious, in the form of rashes, blisters, and sores. What diseases are most common?
What did this appear?
Trying to figure out what kind of rash, blister or plaque appears on your child's skin? Of course, you yourself can determine the most common skin diseases that appear on your child’s skin, but do not self-medicate, be sure to consult a doctor. The doctor will make an accurate diagnosis and prescribe adequate treatment.
Ringworm in children
Ringworm is a contagious fungal skin disease. A child can become infected from a sick person, from a sick animal, or through contaminated personal hygiene items (comb, towel). Ringworm begins with a red spot or plaque with gray scales and has a round or ring-shaped shape. Treated with antifungal ointments.
Erythema infectiosum
One of the most common childhood diseases. It begins with flu-like symptoms (runny nose, body aches), redness of the cheeks and a rash all over the body. It is transmitted by airborne droplets and is contagious for a week before the rash appears. Treatment includes bed rest, drinking plenty of fluids, and painkillers.
A highly contagious disease, it is transmitted by airborne droplets and spreads quickly. The first signs of chickenpox are a rash all over the body, a high temperature, general malaise and headache. The rash goes through several stages:
- pink spot,
- a small blister filled with clear fluid that itches
- the bubbles dry out after 1-2 days,
- covered with a brown crust.
Treatment includes bed rest, gentle nutrition, and hygienic wound care.
Impetigo in children
A contagious infection caused by staphylococcus or streptococcus is transmitted through close contact and through personal hygiene items. With impetigo, red spots appear on the face that turn into blisters. Gradually, blisters filled with cloudy liquid open, then oozing ulcers form and, at the final stage, honey-colored crusts appear. It is treated with antibiotic-containing ointments; a course of antibiotics and tetracyclines (Unidox, etc.) may be prescribed.
Warts are small skin growths that occur as a result of contact with sick children or through the use of shared objects (toys). Most often, warts appear on the hands and face. In most cases, warts are harmless and painless and go away on their own. If the warts begin to hurt or bleed, you should consult a dermatologist.
Miliaria occurs due to blocked sweat glands and appears as small red or pink dots. Heat rash appears on the head, neck and shoulders when parents, with the best intentions, dress the child warmly, and the child sweats a lot; Miliaria also appears in hot weather. In cold weather, a child is dressed in 1 layer of clothing more than an adult; in the hot season, let the baby’s skin breathe.
Contact dermatitis
Contact dermatitis is a skin reaction caused by contact with an irritant. For example, when in contact with:
- plants - buttercup, spurge;
- caterpillars or insects;
Redness, blisters, and a burning sensation appear. Contact dermatitis usually goes away on its own when there is no longer contact with the irritant.
Hand-foot-mouth syndrome (Coxsackie virus)
It is caused by an enterovirus and most often occurs in children under 3 years of age. 5-4 days after infection, symptoms similar to a normal viral infection appear, but then painful sores appear on the arms, legs and mouth. The disease spreads by airborne droplets. Treatment includes taking anti-inflammatory drugs prescribed by your doctor.
Hives
Urticaria is an allergic disease. Hives manifest as rashes and blisters, which may be accompanied by itching or burning. Hives can appear on any part of the skin and go away in a few minutes or days. Hives can be caused by:
- medications (aspirin or penicillin),
- food (eggs, nuts, shrimp),
- heat,
- infections, such as strep throat.
Rule out the cause of the hives; if the hives do not go away, consult a doctor.
Scarlet fever
Scarlet fever is an acute infectious disease that is accompanied by a rash all over the body. Infection occurs through the air, but hand washing can reduce the possibility of infection. Symptoms of scarlet fever: sore throat, fever, headache, pain in the stomach, inflammation of the tonsils, a rash appears by the end of the first day. The pinpoint rash spreads throughout the body, resembles reddened goose bumps, and is often accompanied by itching. The tonsils may be prone to accumulation of pus. After 2-4 days, the rash disappears; on the 5-6th day of illness, peeling of the skin appears at the site of the rash.
Roseola infantile (sixth disease)
The causative agent is the herpes , affecting children under 2 years of age. The symptoms resemble a viral infection - fever with high temperature. The temperature suddenly drops after 2-4 days and a small pink rash appears on the body; the rash does not bother the child. At the first stage, the disease is treated with antipyretics. The rash goes away without a trace after 3-7 days.
If you believe the statistics, then more than 2 million people in the world suffer from trophic ulcers. Mostly older people get sick. They begin to have difficulty climbing the stairs, quickly get tired and freeze. Their feet are cold almost all the time and hurt at night. Urgent treatment is necessary, otherwise ulcers will form.
Trophic ulcers are difficult to treat, since cell nutrition and regeneration are impaired.
Prevention
To avoid the penetration of a fungal infection into the child’s body, it is recommended to adhere to the following rules:
- Strengthen the baby's immunity by hardening, choosing healthy foods and taking vitamin and mineral complexes.
- Always dress your child according to the weather, avoiding hypothermia or overheating.
- Avoid items made from synthetic fabrics and wear socks and shoes made from natural materials.
- Make sure that the child does not wear someone else’s shoes, but wears slippers in public places.
- Take care of the skin of your feet and nails using personal hygiene items.
- Periodically take baths with soda solution and after the procedure lubricate the skin with moisturizer.
- Regularly treat insoles with disinfectants and dry them well.
Fungal infection of the skin of the foot is a common disease among young children that requires timely treatment. With the right choice of medications, the pathology will have a favorable outcome, so if you notice the first symptoms of mycosis, you should consult a dermatologist.
The doctor will carry out diagnostic measures and prescribe effective therapy aimed at eliminating unpleasant manifestations and suppressing the mechanisms of disease development.
Trophic ulcers of the lower extremities: main types
Impaired blood flow in the legs is the cause of insufficient nutrition of epithelial cells. Without nutrition, epithelial cells gradually die. According to the reason that caused the formation of the ulcer, the following types of diseases were named:
- venous ulcers;
- diabetic ulcers;
- neurotrophic ulcers;
- hypertensive ulcers;
- pyogenic ulcers;
- arterial ulcers.
Venous ulcers
Such ulcers mainly form on the lower leg. They are caused by varicose veins of the lower extremities, causing first varicose eczema and then ulceration. Before an ulcer appears, swelling of the calf occurs, the leg becomes heavier, and cramps appear at night. Then the veins on the lower leg enlarge, forming a mesh. The veins gradually connect to form a purple or purple spot. It gradually expands, its tissues become dense, smooth and shiny.
Finally, whitish-colored clamps are formed. The leg must be treated urgently, otherwise an ulcer will appear that will further develop. First, the ulcer affects the upper epithelium, then it penetrates further, up to the tibia. The ulcer produces pus with an unpleasant odor. Without proper treatment, the patient will experience erysipelas, thrombophlebitis and thrombosis in the legs, and the appearance of elephant shin. In severe cases, the person becomes ill with sepsis and dies.
Diabetic ulcer
If you have diabetes, a person will face many troubles, one of them is an ulcer, leading to diabetic gangrene. First, the nerve endings die and the leg loses sensitivity.
The surface of the leg remains cold, and the patient suffers pain at night. The ulcer forms at the big toe, sometimes on both feet. Foot injury and corns are the main cause of ulcers. A diabetic ulcer must be treated urgently, otherwise an infection will be added to the disease, which will cause gangrene. Then, to save a person’s life, his leg will have to be amputated.
Hypertensive ulcer
Such ulcers occur rarely in people with high blood pressure. Mostly women who have crossed the forty-year mark suffer from such an ulcer. First, a papule or simple reddish-bluish, slightly painful spot forms. Then an ulcer forms on both legs at once. The ulcer develops very slowly, but causes pain day and night. It can cause bacterial infection.
Neurotrophic ulcers
Such ulcers are formed due to injury to the head or spine. They form on the heel or on the heel side of the foot. The ulcer penetrates deeply into the tissue, reaching the bone or tendon. It is small and not sensitive, but with pus and an unpleasant odor.
Pyogenic ulcer
The reason for the appearance of such an ulcer is low immunity, in which a person becomes infected with furunculosis or purulent eczema. Such ulcers most often form in a person who does not maintain personal hygiene. Oval-shaped ulcers appear throughout the lower leg. They penetrate shallowly into the skin.
Arterial ulcers
With atherosclerosis, the main arteries become diseased, causing ischemia of the soft tissue of the leg. As a result, ulcers form. The cause of the disease is hypothermia of the feet, wearing shoes one size too small, calluses or wounds. In this case, ulcers form on the foot or on the sole, on the big toe.
These are not large purulent wounds, with dense edges, surrounded by yellowish skin.
The disease is characterized by a deep inflammatory process of the soft tissues of the leg. When the ulcers heal, scars remain on the skin.
general description
Mycosis of the feet is a dermatological disease caused by dermatophytes, molds or yeasts. The pathology has a number of characteristic signs that cause significant discomfort to the small patient, and in the absence of proper treatment can be complicated by severe skin lesions or bacterial infection.
Unlike adults, children are more susceptible to mycosis, since their immunity is not sufficiently developed, and the skin on the legs is too thin and delicate, which allows fungi to easily penetrate the body and multiply.
Important!
According to many doctors, children's skin is ideal for the rapid proliferation of fungi that love a warm and humid environment. In addition, newborns can also become infected if the woman did not have time to get rid of thrush at the time of birth.
How to treat a trophic ulcer
The doctor prescribes individual treatment for each patient. It takes into account the type of ulcer the patient has. Before treating the patient, it is necessary to diagnose the disease. Conduct cytological, histological, bacteriological examination. Only then does treatment begin. The ulcer is treated with medication or surgery. In any case, the ulcer is cleaned of pus and dead tissue, treated with antiseptics and lubricated with healing ointment. The wound gradually heals and the skin of the leg is restored. Home treatments help heal ulcers.
Surgical methods
During surgery, dead tissue is removed.
1. Vacuum therapy. Sponge polyurethane dressings are used. They remove pus from the wound, reduce swelling, and restore blood flow to the lower leg. With such an operation, as a rule, there are no complications. Moisture inside the wound prevents bacteria or viruses from appearing.
2. A catheter is used to treat ulcers that are difficult to treat.
3. For a hypertensive ulcer, the veins are sutured to separate them.
Treatment of trophic ulcers with medications
Medicines are used during any surgical operation. However, they can be used independently to treat some types of this disease.
Treatment is divided into three periods.
1. First, the patient is prescribed antibiotics.
2. Next, anti-inflammatory drugs are used.
3. Then they give injections of pentoxifylline.
Be sure to wash the wound with antiseptics, lubricate the wound with healing ointment and apply a bandage.
Basic treatment methods
Many people are concerned with the question of how to treat streptoderma at home, but it is worth understanding that therapy must be carried out under the strict supervision of a specialist in compliance with all instructions.
The main method of treating the disease is the use of drugs and ointments that attack the streptococcal agent.
Plantex for newborns - instructions for using medicine to improve digestion in the smallest (135 photos and videos)- Vitamins for hair: selection of a vitamin complex for skin and nails. Rating of effective vitamin complexes for hair growth (130 photos)
The first signs of otitis in children - the main causes, symptoms, forms, diagnosis and treatment of the disease (145 photos and videos)
During therapy, drying ointments containing an antimicrobial effect are used. Broad-spectrum antibiotics are also mandatory in treatment.
There are a number of mandatory measures required during the treatment of streptoderma:
- During an infection, do not wash or wet the affected areas;
- Moisturizing ointments should not be used;
- In parallel with antibacterial therapy, it is necessary to carry out immunoprophylaxis of the body.
- In some cases, antibiotic treatment should be accompanied by prebiotics.
To summarize, we can come to the conclusion that streptoderma is a rather dangerous and insidious disease that requires full treatment and an integrated approach to combating infection.
It is important to take preventive measures to avoid such pathology.
Compression bandages
A bandage is used throughout the treatment. It consists of several elastic bandages and gently compresses the affected veins. It is recommended to change the bandage daily. It helps treat venous ulcers. Such dressings improve blood flow in the veins and reduce swelling. The use of Saphena Med UCV venous ulcer is effective. This is a pair of elastic stockings. The use of medical knitwear also has a positive effect. In addition, physiotherapeutic procedures are used to treat trophic ulcers. Traditional methods are also used. The main thing, according to experts, is to start as early as possible, and always under the supervision of a specialist.