Causes of cystic fibrosis
The main causes of cystic fibrosis are mutations in genes encoding a protein that takes part in the water-electrolyte metabolism of epithelial cells. As a result, the secretion they secrete becomes thick and is removed outside with great difficulty. Due to its constant accumulation, the glands undergo deformation and irreversible processes begin to occur in them. As a result, everything ends with the death of the glands and their replacement with connective tissue. Such changes lead to the organ ceasing to function.
Mucus begins to stagnate in the bronchi. This makes it difficult for the ciliated epithelium to work. Dust, small smoke particles, viruses and bacteria settle on the surface of the mucous membrane. In conditions of high humidity and temperature, microorganisms multiply well, causing an inflammatory process. Prolonged, low-grade inflammation leads to a decrease in local immunity, deformation of the ciliated epithelium of the bronchi, and even greater disruption of its function. The bronchi become less elastic, their lumen constantly narrows, creating an even more favorable environment for the proliferation of bacteria.
Constant accumulation of mucus makes breathing difficult. The body does not receive enough oxygen. As a result, the functioning of all organs and systems is disrupted.
Since the pancreas produces too thick a secretion, its ducts become clogged. This further complicates the outflow of secretions and causes inflammation. In conditions of the inflammatory process, the supply of oxygen and nutrients deteriorates. Sclerotic processes are activated in the organ. The gland becomes deformed and its function is further impaired. Since an insufficient amount of enzymes is released into the child’s duodenum, the stool becomes very viscous, constipation and bloating develop. Due to malabsorption of nutrients, the child lags behind in physical development.
Prevention
Since the disease is genetic, the main preventative measure is its detection as early as possible. If there have been cases of the disease in the family, then even at the stage of pregnancy planning you need to consult with a geneticist and undergo a series of examinations.
If a child has been diagnosed with cystic fibrosis, parents may also be recommended to undergo genetic testing. This is useful for confirming the diagnosis and prenatal diagnosis in future pregnancies.
At the moment, a disease such as cystic fibrosis is incurable. However, it can and must be fought, so parents should not give up. Modern science is actively developing, so many experts hope that in the future children born with this disease will have a chance for a complete cure.
Signs and symptoms of cystic fibrosis
Clinical symptoms of cystic fibrosis depend on the form of the disease:
- pulmonary form. As the name suggests, this form of cystic fibrosis affects the respiratory system. The patient develops chronic bronchitis with difficult to separate sputum, and frequent pneumonia is observed. The cough is constant, exhausting, and causes insomnia. As a result, pulmonary and then heart failure develops first;
- intestinal form. It manifests itself as symptoms of gastrointestinal damage, which leads to anemia, hypovitaminosis and weight deficiency. If the liver is affected, jaundice may develop;
- mixed form. Combines the symptoms of intestinal and pulmonary forms of the disease;
- atypical forms. Meconium ileus in newborns. Viscous intestinal contents clog the newborn's intestines, which makes it impossible to pass stool.
The layering of infection is accompanied by a pronounced intoxication syndrome. The patient's temperature rises, complaints of general weakness, sweating, and severe malaise arise. The cough intensifies and often becomes debilitating. The patient loses his appetite, and his performance is greatly reduced. Bronchitis and pneumonia are difficult to treat and tend to be protracted.
In infants, the symptoms of cystic fibrosis are:
- thick and greasy feces, with a pungent, foul odor;
- rectal prolapse; enlarged liver;
- delayed physical development;
- bloating;
- deformation of the chest and phalanges of the fingers;
- dry skin;
- lingering dry cough.
Often, when kissing, a mother notices the salty taste of the baby’s skin. With additional examination, the doctor confirms the diagnosis of cystic fibrosis.
What are the forecasts
Cystic fibrosis is a serious pathology, and it is completely impossible to cure it. The degree of favorable prognosis will depend on the presence (absence) of complications, as well as on the timing of diagnosis of the first symptoms of the disease. Medical statistics show that the prognosis is worse for those children whose first symptoms of the disease appeared in infancy. A positive treatment outcome occurs with early diagnosis of cystic fibrosis and correct, targeted treatment of the newborn.
If you look at the statistics, you can see that child mortality from cystic fibrosis has decreased significantly over the past 50 years (from 80% to 36%). Many children with this hereditary pathology have increased life expectancy due to the achievements of modern medicine.
Disease severity
In determining the severity of cystic fibrosis, signs of damage to the respiratory system play a major role. Depending on their severity, the following degrees of severity of the pathology are distinguished:
- I - cystic fibrosis is characterized by minor changes of a non-permanent nature, cough and shortness of breath appear only during physical exertion;
- II - manifested by a chronic inflammatory process in the bronchi, constant moderate shortness of breath and deformation of the phalanges of the fingers. On auscultation, moist rales are heard;
- III - manifested by progressive damage to the bronchi and lungs, with the development of foci of fibrosis and sclerosis, the appearance of bronchiectasis, and the appearance of signs of cardiac and respiratory failure;
- IV - accompanied by severe heart and lung failure.
Assessing the symptoms, the doctor adjusts the dosage of drugs, thereby ensuring complete treatment of cystic fibrosis.
Examination at home
The diagnosis, of course, is made by a qualified specialist, but attentive parents can pay attention to some features:
- Infants with cystic fibrosis have meconium ileus from birth. The small intestine becomes clogged with original stool. Meconium is so dense and dense that it simply cannot be evacuated from the intestines. If the large intestine is blocked in the first two days after birth, the baby will not have a bowel movement;
- when parents kiss a child, they may notice that the skin tastes salty;
- the child does not gain enough weight for his age, although his appetite is not impaired;
- jaundice. This symptom may also be a manifestation of other diseases, or may be a variant of the norm, so a differential analysis is carried out by an experienced doctor;
- infectious processes of the chest cavity. Thick mucus is a fertile ground for the development of bacterial infections. The child often suffers from bronchial infections, as well as chronic cough. Parents may notice severe wheezing and shortness of breath;
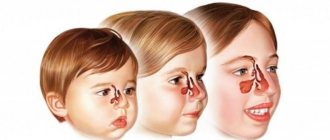
- the disease also provokes the development of sinusitis - inflammatory processes in the paranasal sinuses, as well as tonsillitis, polliposis and adenoiditis;
- abdominal pain and bloating are another manifestation of the disease;
- feces smell bad, they take on a loose shape and have a shiny surface, this is due to the fact that fats are poorly digested by the body;
- part of the rectum may protrude from the anorectal area. This is associated with two problems: chronic cough and hard-to-pass stool.
Diagnosis of cystic fibrosis
Timely diagnosis of cystic fibrosis is of great importance for a child’s life. Before a diagnosis of cystic fibrosis is made, the following measures are taken:
- study of hereditary history, early symptoms and clinical manifestations of the disease; urine and blood analysis (general);
- coprogram is a study of feces for the content of starch, muscle fibers, fiber, fat, with the help of which the degree of disruption of enzymatic processes in the glands of the digestive tract is determined;
- sputum examination (microbiological);
- X-ray examination of the lungs - to identify sclerotic and infiltrative changes in their tissues; bronchography – detect bronchial defects;
- bronchoscopy - determine the presence of viscous and thick thread-like sputum in the bronchi;
- spirometry - determine the functional state of the lungs by measuring the speed and volume of exhaled air;
- molecular genetic testing – DNA or blood samples are analyzed to identify mutations in the cystic fibrosis gene;
- a sweat test is the main test for cystic fibrosis, with the help of which the patient is diagnosed with an increased content of sodium and chlorine ions in the sweat;
- prenatal diagnosis of cystic fibrosis - newborn children are examined for congenital and genetic diseases.
The intestinal form of cystic fibrosis must be distinguished from intestinal absorption disorders observed with disaccharidase deficiency, dysbacteriosis and enteropathy. The pulmonary form is differentiated from bronchial asthma, pneumonia of other origins, whooping cough and obstructive bronchitis.
What is cystic fibrosis in children
Cystic fibrosis is a hereditary systemic disease accompanied by damage to the exocrine glands (exocrine glands).
This is interesting! The name of the disease comes from the Latin words mucus (“mucus”) and viscidus (“viscous”).
In cystic fibrosis, thick, sticky mucus accumulates in the airways
Cystic fibrosis develops due to a mutation in the CFTR (cystic fibrosis transmembrane regulator) gene, located on the seventh chromosome. This mutation leads to dysfunction of a protein that is involved in water-salt metabolism and regulates the passage of sodium and chlorine (that is, salts) through cell membranes, resulting in cells losing these elements.
The gene “responsible” for cystic fibrosis was found only in 1989.
This disease affects all organs that produce mucus: bronchi and lungs, pancreas and liver, sweat and salivary glands, intestines, gonads. Cystic fibrosis is one of the most common genetic disorders; today about 1000 types of mutations of this gene are known, which causes a varied clinical picture and individual course of the disease in each child. The disease is diagnosed in utero or before the age of 1-2 years. Cases of later diagnosis are very rare.
Most often, cystic fibrosis is diagnosed in children under one year of age.
This is interesting! Every year in Russia 300 children are born with cystic fibrosis (1 child per 10,000 newborns), in the USA - 2,000 children (7-8 children per 10,000 newborns), in general in the world - over 45,000 children.
The risk of a gene mutation does not depend on the gender of the child; boys and girls are equally susceptible to it.
In Russia, for many years, the treatment of children diagnosed with cystic fibrosis was not given due attention; only in the 90s of the last century did federal and regional centers to combat this disease begin to open. The average life expectancy of people with cystic fibrosis is 16-25 years.
Features of cystic fibrosis in children (video)
Treatment of cystic fibrosis
How to treat cystic fibrosis? Treatment for cystic fibrosis depends on the form of the disease. If the intestinal form of the disease predominates, then a diet is indicated. Food should contain a large amount of proteins (eggs, cottage cheese, fish and meat). The consumption of fats and carbohydrates is sharply limited (only their easily digestible forms are allowed). It is necessary to exclude coarse fiber and milk from the diet (for lactose intolerance). You should also take vitamins and drink plenty of fluids (especially in summer).
Replacement therapy for this form of the disease includes taking enzyme preparations (Mezim, Festal, Panzinorm and a number of others). The frequency and dosage of medications is determined by the attending physician based on the severity of the disease and the severity of excretory insufficiency of pancreatic function. The effectiveness of the treatment is judged by the restoration of the patient’s weight, the absence of neutral fat in the stool, the disappearance of pain and the normalization of stool. Therapy for the pulmonary form of cystic fibrosis is aimed at restoring bronchial patency, reducing sputum viscosity and eliminating the inflammatory process. For this purpose, the prescription of mucolytics (acetylcysteine, mucosolvin), which are used in the form of inhalations or aerosols throughout the patient’s life, is indicated.
If inflammation of the lungs or bronchi develops, antibiotic therapy is indicated. Preference is given to broad-spectrum drugs that are active against most bacteria. Medicines are prescribed both in tablet form and by injection. The daily and course dose is determined by the attending physician based on the individual characteristics of the patient.
Steroidal anti-inflammatory drugs are used according to indications. They effectively reduce the activity of the inflammatory process, eliminate spasm of bronchial smooth muscles, relieve swelling, thereby increasing the lumen of the airways, normalizing breathing. In addition, physical therapy, vibration massage of the sternum and physical therapy are prescribed. For therapeutic purposes, bronchoscopic sanitation is performed using mucolytics. For acute pneumonia or bronchitis, antibacterial drugs are prescribed. In addition, the prescription of drugs that improve the nutrition of the heart muscle is indicated. Patients diagnosed with cystic fibrosis should be regularly examined by a physician and pulmonologist. Parents of a sick child should be trained in the rules of caring for him. The question of whether to prescribe preventive vaccinations for a child is decided on an individual basis. Children suffering from a mild form should receive sanatorium treatment for cystic fibrosis.
It is better for them not to go to kindergarten. As for school, the possibility of attending it depends on the general condition of the child.
Which doctor should I contact?
First, you should show your child to the pediatrician. Afterwards, you will need to consult a gastroenterologist and pulmonologist. Specialists will prescribe the necessary tests and examinations:
- DNA testing of parents and close relatives.
- Test for chlorine and sodium levels in a child's sweat.
- Blood, urine, feces, sputum tests.
- Spirogram of the lungs, study of the secretion of pancreatic enzymes.
If a mixed or intestinal form is detected, treatment will be carried out by a gastroenterologist. In case of mixed or pulmonary form - a pulmonologist. With such a serious illness, a whole team of specialists must fight for the baby.