Scarlet fever is an infectious disease that occurs as a result of exposure to erythrotoxin (from Greek - “red toxin”). It is produced by group A beta-hemolytic streptococcus (S. Pyogenes). These bacteria may be part of the normal microflora of a healthy person. Most often they create colonies in the nasopharynx, less often in the intestines, genitals or on the skin.
The disease mainly affects children from 2 to 12 years old. The peak occurs in the autumn-winter period. Adults and children under one year of age rarely get scarlet fever. Epidemics of scarlet fever occur every 3–5 years. The disease is very rarely fatal.
The natural susceptibility to the disease in children is quite high. After the child has recovered, he remains with type-specific immunity (he is not susceptible to bacteria of the subspecies that caused the disease). In some cases, re-infection is possible.
Causes of scarlet fever in children
The disease is transmitted from a person suffering from scarlet fever, streptococcal sore throat and other forms of respiratory infections. In most cases, the patient sheds bacteria within 3 weeks from the onset of the first symptoms. It poses the greatest danger in the first days of the disease.
Absolutely healthy people who are its carrier can isolate hemolytic streptococcus. This process can take years.
Possible routes of infection:
- Airborne. When sneezing, coughing or talking through droplets of saliva and mucus from a carrier of the infection.
- Contact and household. Streptococcus bacteria, depending on air humidity and ambient temperature, can live on the surface of dishes, toys or household items from several hours to several days. Infection can also occur through the nutritional route, through food.
Prevention of disease occurrence
Reducing the spread of the disease and its prevention is facilitated by the isolation of sick children and the introduction of quarantine in children's institutions where there are cases of scarlet fever.
There is no special vaccine or vaccination for this disease. The room where a sick person is located should be wet cleaned regularly. The cutlery and bedding he uses are disinfected by boiling. All children who have been in contact with a person with scarlet fever undergo a medical examination to identify signs of infection.
For preventive purposes, they are prescribed irrigation of the throat with Tomicide for 5 days. The same therapeutic rinses should be performed for children who have chronic inflammatory processes in the nasopharynx.
source
Stages of scarlet fever in children
The clinical course of scarlet fever in children is divided into three stages:
- Incubation period. Its duration is 1–12 days (in most cases – from 2 to 7 days). At this time, the pathogen multiplies in the body. There are no symptoms of the disease, the child’s general well-being is not affected.
- The period of developed manifestations. Its duration is 5–10 days. Manifested by the appearance of clinical symptoms characteristic of scarlet fever.
- The period of recovery (reconvalescence). Its duration is 10–15 days. By the end of this period, all signs of the disease disappear.
Complications of scarlet fever and the possibility of relapses
Scarlet fever can cause such dangerous complications as otitis media, sinusitis, myocarditis, glomerulonephritis, pneumonia, arthritis, and rheumatism. They usually occur in the 3rd week of illness - during the period of formation of antibodies to the pathogen, sometimes mistakenly mistaking the body’s own tissues for it.
There are no relapses of the disease, as those who have recovered from the disease acquire lasting immunity. But other types of infections caused by streptococcus may occur, such as tonsillitis or otitis media.
Symptoms of scarlet fever in children
The characteristic initial symptoms of scarlet fever in children are:
- Increase in body temperature to 39–40 °C.
- The appearance of headache, general weakness, lethargy, drowsiness, apathy. But in some cases there is hyperactivity.
- Pain in the throat when swallowing.
- Decreased appetite.
- The appearance of abdominal pain. If the disease is severe, nausea and vomiting may occur.
With a milder course of the disease, the child may experience a slight rise in temperature, which is accompanied by a rash. Other signs of scarlet fever in children are mild or completely absent.
With timely diagnosis and adequate treatment, the prognosis is favorable. Within 10–14 days, complete recovery is possible without the development of subsequent complications.
In addition to the described symptoms, the disease is characterized by certain signs.
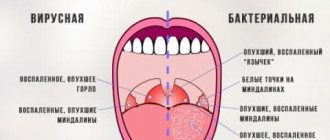
Sore throat with scarlet fever
Scarlet fever in children is accompanied by follicular or lacunar tonsillitis. In this case, the child experiences the following symptoms:
- Redness and swelling of the tonsils and back of the throat.
- Pain in the throat when swallowing. The pain can be very acute, causing the child to refuse to eat.
- Enlarged lymph nodes. They become dense and painful.
Changing tongue color
This symptom allows you to distinguish scarlet fever from other diseases. At the initial stage of the disease, the tongue becomes dry, and a white or brown coating appears on it. From about the fourth day of the disease, it clears and acquires a characteristic crimson color. At the same time, the papillae on it increase.
This characteristic sign of scarlet fever in children is called raspberry tongue. It is observed until the twelfth day of the disease.
Rash
A day after the appearance of the general symptoms of scarlet fever in children, a small rash appears on the child’s skin. Initially, the skin of the face and neck becomes covered, then the rash spreads to the inner surface of the limbs.
The pimples have a pink tint with a brighter center. Their size can reach 2 mm. The rash rises above the surface of the skin. Visually it is not very noticeable, but the skin feels like sandpaper to the touch.
The elements of the rash are located very densely and practically merge. There is redness around the pimples. The rash thickens in the form of dark stripes in the area of natural folds, on the sides of the torso, in the buttocks, axillary, inguinal folds and in the lower abdomen. Elements of the rash occur in areas where sweating is stronger and the skin is thinner, since beta-hemolytic streptococcus toxins are eliminated through the pores of the skin.
Under the neck, in the bends of the elbows and knees, dark stripes are observed that do not disappear with pressure. The reason for their appearance is the fragility of blood vessels, resulting in small hemorrhages.
The child's cheeks become red, while there is no rash in the area of the nasolabial triangle.
Another important symptom of scarlet fever in children is white dermographism. If you rub a blunt object or palm over the skin, a white mark will form (the rash will temporarily disappear).
Elements of the rash disappear in 3–5 days. Sometimes they can last for several hours. When they disappear, they do not leave scars, scars or age spots.
Peeling
After 7–14 days from the onset of the disease, another symptom appears – peeling of the skin. On the hands it starts from the free edge of the nail, gradually moves to the tips of the fingers and covers the entire palm. The skin comes off in layers. Antibodies that bind toxins accumulate in the body. On the face and in the folds, where the rash is intense, peeling occurs.
The toxic form of scarlet fever in children is characterized by the following symptoms:
- Rapid onset of the disease and a sharp rise in body temperature to 40 °C.
- Meningeal phenomena.
- Clouding of consciousness, in some cases convulsions.
- Repeated vomiting, which may be accompanied by diarrhea.
- Severe catarrhal tonsillitis.
- Dry lips.
- Increased heart rate up to 160 beats per minute.
- Decreased blood pressure.
- A pronounced rash.
With severe toxicosis, the skin turns blue, the rash turns pale, the extremities become cold, the pulse becomes thready, and loss of consciousness is possible.
Scarlet heart
This is a characteristic symptom of scarlet fever in children, developing as a result of exposure to streptococcal toxin. The heart increases in size, its walls swell and become soft. As a result, the pressure decreases, chest pain and shortness of breath appear. After the toxin is bound by antibodies accumulated in the body, this symptom disappears.
In the septic form of the disease, against the background of the appearance of scarlet fever symptoms on days 2–4, the child’s condition sharply worsens, and the cervical lymph nodes become denser, increase in size and become very painful. The palatine tonsils are affected by a necrotic process that spreads very quickly to the nasopharynx.
The child becomes lethargic, apathetic and refuses food and water. Abundant purulent mucous discharge from the nose appears. The tongue becomes dry, cracks appear on the lips. Otitis may develop. The disease recedes very slowly.
The hypertoxic form of scarlet fever is characterized by the following symptoms:
- The disease develops very quickly, the temperature rises to 40–41 °C.
- The heart rate increases, repeated vomiting and convulsions appear.
- The skin turns blue, making it impossible to recognize the rash.
- The child quickly loses consciousness and falls into a coma.
In very rare cases, in addition to symptoms of intoxication, hemorrhages in the mucous membranes and skin are observed, which can lead to death.
In typical cases, scarlet fever in children is quite easy to diagnose based on characteristic signs.
With rudimentary scarlet fever in children, the following symptoms are revealed:
- Low-grade fever (37.1–38.0 °C) for two to three days or throughout the entire period of the disease.
- Slightly enlarged lymph nodes.
- Slight increase in heart rate.
- Spot redness of the pharynx.
- Mild pain when swallowing.
- The rash is pale, may be located only in the folds of the arms and legs and on the stomach and disappears within a few hours.
- Peeling begins late or is absent altogether.
The extrabuccal form of scarlet fever is very rare. It differs from other types of disease in that the gateway to infection is not the pharynx, but damage to the skin or mucous membranes (in case of burns or wounds). This form of scarlet fever is not contagious as it is not spread by airborne droplets. It is characterized by the following symptoms:
- Inflammation of regional lymph nodes located at the gates of infection.
- Localization of the rash near the skin lesion.
- No signs of inflammation in the throat.
With the erased form of scarlet fever in children, signs of the disease are absent or are of an unexpressed nature. Patients are carriers of the infection, and it is very difficult to diagnose them correctly.
Incubation period
Scarlet fever is not just contagious, but a highly contagious infection. Upon contact with a patient or carrier, infection most often occurs if there is no antitoxic immunity. About 20% of the population is a carrier of group A streptococcus, and the pathogen can be released into the environment throughout the year. The incubation period can last from one to twelve days. The pathogen settles on the mucous membranes of the nasopharynx and oral cavity, primarily on the tonsils. On average, the latent incubation period lasts 2-7 days. Then symptoms appear acutely (or, conversely, inexpressibly). On average, the acute period of the disease lasts about 5 days, after which recovery occurs, which can take from one to three weeks. Most often, scarlet fever affects preschool children who attend kindergartens. But primary schoolchildren, teenagers and adults who did not have scarlet fever in childhood can also become infected with scarlet fever.
Diagnostics
In typical cases, scarlet fever in children is quite easy to diagnose based on characteristic signs.
Laboratory tests include:
- General blood analysis. The study reveals an increased level of ESR and leukocytosis.
- Bacterial culture. The material is taken from the oropharynx and cultured to isolate the causative agent of the disease and determine its sensitivity to antibiotics.
Scarlet fever is differentiated in children with the following diseases:
- Rubella.
- Measles.
- Drug dermatitis.
- Pseudotuberculosis.
- Eneroviral exanthema.
How does the disease progress in a mild form?
Recently, cases of mild scarlet fever have become more frequent, which occurs without fever or with low-grade fever, also without severe intoxication. The child may complain of slight discomfort, but he does not have the typical symptoms: redness and sore throat. The rash, when erased, is not expressed. Only a doctor can determine the signs of scarlet fever in children by the characteristic rash. Parents often mistake rashes for allergies and do not consult a doctor, since there are no other symptoms or complaints. Only after characteristic peeling on the palms and soles and contacting a doctor is scarlet fever established as a diagnosis after the fact. Unfortunately, the erased form of scarlet fever can cause complications, since it has not been treated in any way. The doctor will recommend taking tests and undergoing additional examinations to eliminate dangerous consequences.
Treatment of scarlet fever in children
Most often, treatment is carried out at home. The sick child is isolated. In case of severe infection, hospitalization is indicated for a period of at least 10 days. Then, for 12 days, the child must stay at home and should not be allowed into the children's group.
During treatment, the child must remain in bed and eat properly. Preference is given to pureed, easily digestible food, steamed or boiled. It should be consumed in small portions, at least 4 times a day. Doctors recommend adhering to therapeutic diet No. 13 according to Pevzner, and after two weeks – diet No. 7. It is also necessary to maintain a drinking regime.
For the treatment of scarlet fever in children, the following groups of drugs are used:
- Antibiotics (penicillins, macrolides, cephalosporins). They are used in the form of tablets or injections. Treatment is continued for 7–10 days.
- Antihistamines. They reduce itching, eliminate swelling, and prevent the development of allergic reactions.
- Non-steroidal anti-inflammatory drugs. They are prescribed to lower body temperature and relieve headaches.
- Vitamin complexes. They improve the functioning of the immune system.
- Eubiotics. Drugs in this group are used in combination with antibiotics to restore intestinal microflora.
- Antifungal agents. They can be prescribed by a doctor as part of a comprehensive treatment to prevent or eliminate concomitant fungal infections.
- Antiseptic and anti-inflammatory local drugs.
If the child is in serious condition and refuses to eat or drink, saline solutions and glucose are administered intravenously, which helps remove toxins from the body.
In the septic form of the disease, against the background of the appearance of scarlet fever symptoms on days 2–4, the child’s condition sharply worsens, and the cervical lymph nodes become denser, increase in size and become very painful.
Quarantine measures
Since scarlet fever is a contagious disease, a kindergarten or school class is quarantined for 7 days after the onset of the disease. If children who have been in contact with a sick child have a sore throat, they are suspended from visiting the child care facility for 22 days. At home, prevent the patient from contacting other children.
The duration of treatment for scarlet fever is usually 10–14 days. The body's recovery period lasts 21 days. Even if the child’s health returns to normal and the symptoms of the disease completely disappear, the child must follow a home regime during this period, since there is still a danger of developing complications.
Complications
Early complications of scarlet fever in children:
- Lymphadenitis is inflammation of the lymph nodes as a result of the accumulation of bacteria.
- Pharyngitis is an inflammatory process in the walls of the pharynx.
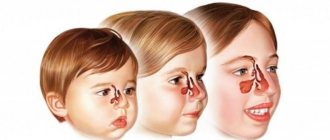
- Sinusitis is inflammation of the sinuses.
- Necrotizing tonsillitis is the death of the mucous membrane on the tonsils.
- Sepsis is a condition caused by the entry of infectious agents into the blood.
Late complications of scarlet fever:
- Myocarditis. This is an inflammatory lesion of the heart muscle, causing disruption of blood circulation and heart rhythm.
- Synovitis. Serous inflammation of the joints, characterized by swelling and pain. This complication may occur in the second week of the disease.
- Glomerulonephritis. Kidney damage, causing lower back pain, swelling and impaired urine production. Occurs after the symptoms of scarlet fever disappear. In the absence of timely treatment, renal failure develops.
- Rheumatism. It is the most common complication of scarlet fever and can develop 4–5 weeks after the illness. Sydenham's chorea can be a complication of rheumatism after scarlet fever. This is a pathology in which motor activity is impaired. The child experiences twitching of the limbs, seizures, hearing and vision impairment.
Causative agent of scarlet fever
Streptococci have a round (spherical) shape. Arranged in chains or in pairs. They do not form a dispute. Gram-positive. On gram they are colored blue. They grow well on nutrient media containing glucose, blood and serum. There is pronounced enzymatic activity of bacteria. They are able to decompose glucose, lactose, maltose and sucrose.
Streptococci reproduce by dividing in two. Bacteria quickly die at high temperatures, in sunlight and from the action of disinfectant solutions. In the external environment (in dust, sputum, pus) they persist for months. They tolerate low temperatures and freezing well. Streptococci are sensitive to a number of antibacterial drugs. Resistance to them develops slowly.
Rice. 2. In the photo there are streptococci. Often arranged in chains, less often in pairs. Gram stained blue.
Rice. 3. The photo shows colonies of streptococci. They are small in size, flat, translucent, smooth, shiny. When growing on blood agar, a hemolysis zone is formed around the colonies (photo on the right).
Rice. 4. Streptococci reproduce by dividing in two.
Pyogenic (pyogenic) bacteria are ubiquitous. Group A streptococci cause a number of diseases:
- Superficial infections - sore throats and pharyngitis, bronchitis, pustular diseases of the skin and soft tissues (abscesses, cellulitis, boils, erysipelas).
- Invasive infections (cellulitis, necrotizing fasciitis, myositis, meningitis, endocarditis and pericarditis, pneumonia, sepsis, including postpartum).
- Toxin-mediated infections - rheumatism, scarlet fever, toxic shock syndrome.
Streptococci are capable of producing toxins that damage the tissues of the human body. If, during infection with b-hemolytic streptococci of group A, antitoxic immunity is present in the body, then superficial and invasive infections develop. If there is no antitoxic immunity during infection with group A streptococci, scarlet fever develops.
There are 17 serological groups of b-hemolytic streptococci, designated by letters from A to S. The causative agent of scarlet fever is included in group A, which is divided into 55 serotypes, common to which is an erythrogenic toxin and an allergen (heat-labile and heat-stable fractions of Dick's toxin). Serotypes 1, 2, 4, 27 and 10 are common in Russia.
Hemolytic streptococci are sensitive to various antibacterial drugs. Their distinctive feature is that over many years the microbes have not acquired resistance to the antibiotic penicillin.
Rice. 5. Streptococci in the photo (computer visualization).
What is Dick's toxin?
Scarlet fever toxin or Dick's toxin has allergenic properties and has a toxic effect on the patient's body. The toxin consists of 2 fractions:
- Heat-labile fraction (erythrogenic toxin).
- Heat-labile fraction (allergic component).
Erythrogenic toxin
Erythrogenic toxin has the following properties:
- causes a feverish reaction
- damages tissue cells,
- suppresses the functioning of the reticuloendothelial system,
- increases the permeability of cell membranes,
- causes dilation of skin capillaries,
- causes acute inflammation of the uppermost layers of the dermis and necrosis of epidermal cells.
In just a few hours, an erythrogenic toxin in the body of a person who has not previously had scarlet fever causes fever, intoxication, and the development of catarrhal tonsillitis and pinpoint rash.
Thermolabile fraction
The thermolabile fraction has allergenic properties. Intradermal administration of erythrogenic toxin to previously unaffected persons or to patients during the first week of the disease causes an inflammatory reaction within 4 to 6 hours. The reaction to intradermal administration of erythrogenic toxin to persons who have previously had scarlet fever remains negative throughout their lives. The disease does not develop in such individuals, but when infected with toxigenic strains of group A b-hemolytic streptococci, they may develop a sore throat, erysipelas, or other manifestations of streptococcal infection.
Lifelong antitoxic immunity after scarlet fever
Toxigenic streptococci cause scarlet fever in only a third of infected patients. The remaining infected people develop either a sore throat or a latent form of streptococcal infection, which results in the formation of antitoxic immunity and a negative reaction to Dick's toxin.
In addition to Dick's toxin, endo- and exotoxins and a number of enzymes that they secrete take part in the development of the pathological process. These are protein M of streptococci, C5a-peptidase, streptolysin O, streptolysin S, cardiohepatic toxin, streptokinase, hyaluronidase, etc. Together they can cause severe toxicosis, sepsis and allergization of the body.
Rice. 6. The photo shows streptococci (view through a microscope).