The child's first tests.
When and what kind of research is done for children?
Tests for a child up to a month to a year old Why should a child take tests? Do newborn tests mean something is wrong? Why do they take a general blood test from a newborn? What tests and why does your baby need to undergo? Is there a need for them and how and when should the child be tested for the first time?
FIRST TESTS OF A CHILD: WHAT, HOW, WHY?
An integral part of a medical examination is laboratory diagnostics. The reasons why tests are prescribed for children are varied: clarifying the diagnosis, collecting information about the general state of health, preventing infectious diseases in children. Firstly, preventing a disease is always easier than treating it later. Secondly, the treatment of many diseases directly depends on the timeliness of diagnosis. And the reliability of the results of research tests depends largely on the parents’ ability to correctly collect the material. Therefore, let's find out what tests the baby needs to be carried out and when, and how to do it correctly?
FIRST TESTS OF A CHILD IN THE MATERNITY HOSPITAL
The first tests of newborns are taken in the delivery room, literally in the first seconds of life. Using a drop of blood taken from the umbilical cord, doctors determine the baby's blood type. On the 3-4th birthday, a blood test is performed in the maternity hospital from the heel, the so-called neonatal screening, which allows you to identify hereditary, congenital diseases such as hypothyroidism (decreased thyroid function in the child’s body) and phenylketonuria (metabolic disorder). Blood taken from the baby is applied to a special test form, which is subsequently sent to the laboratory for testing. The child in the maternity hospital is informed about the results of such an analysis only if a disease marker is detected in the blood within 1 month. Just in case, all babies born to mothers with negative Rh factor blood are tested at birth in the maternity hospital from the umbilical cord, in order to prevent hemolytic disease of newborns and other diseases. Sometimes you have to take a blood test in the maternity hospital from a finger or even from a vein, but this is only if necessary. The reason for this is jaundice of newborns. In this way, specialists determine with great accuracy exactly what form of the disease the child has. Normal, that is, physiological jaundice is a fairly common phenomenon, generally not threatening the child in any way. If a newborn’s jaundice turns out to be pronounced and causes serious concern among doctors, then the child has to be tested in the maternity hospital, taking blood from a vein. Such tests of newborns make it possible to determine the content and form of bilirubin in the blood and understand how dangerous the current situation really is.
ANALYSIS OF A CHILD AT 1 MONTH
If newborn tests for hypothyroidism and phenylketonuria, done in the maternity hospital, give a positive result, after discharge from the maternity hospital you will be informed of the need to undergo additional examinations, tests of the child at 1 month, and, if necessary, appropriate treatment. Since the screening test is still an indicative analysis, then, after receiving information about the positive test results, the pediatrician prescribes a more in-depth examination of the baby with suspected hypothyroidism, in particular: consultation with an endocrinologist, additional studies of absolutely all thyroid hormones, x-ray examination thyroid gland, ultrasound of the thyroid gland. If a baby is suspected of having phenylketonuria, after discharge from the hospital, additional special tests are performed on newborns, which include more accurate methods for identifying and determining the amount of the amino acid phenylalanine and its derivatives. To do this, they conduct research by doing blood tests and urine tests on the child.
ANALYSIS OF A CHILD UNDER 1 YEAR OF AGE AND ANALYSIS OF A CHILD AT 1 YEAR OF AGE
If the baby’s health condition does not cause any concern either to the mother or to the doctor who provides patronage, then the following tests for newborns are prescribed only at 3 months, before preventive vaccinations, for which a general blood and urine test is taken from the newborn.
Why do they take a general blood test from a newborn?
Such tests of children are necessary to monitor their health status, not to miss the development of the disease and contraindications to vaccination. A general blood test is taken from the newborn's ring finger. To do this, wipe the outer phalanx with a cotton swab soaked in alcohol and puncture the skin with a disposable scarifier. The results of the analysis will allow you to evaluate the level of hemoglobin, leukocytes, red blood cells and other blood factors. You should not be alarmed when you find that the indicators differ from the “norm” indicated on the standard form. The fact is that the composition of the blood of a newborn baby is qualitatively different from the composition of the blood of an infant, and that, in turn, is different from the blood of older children.
Clinical tests of a child's urine
General urine tests of a child are examined using morning urine collected in a clean, dry container with a lid. To carry out the analysis, a minimum amount of 15-25 ml of morning urine will be required. The delivery time for research material is no longer than 1.5 hours. If urine is stored for a long time, the formed elements decompose, it becomes cloudy and the reaction changes and, therefore, the results are distorted and cannot be considered reliable. The need to undergo this “routine” urine test for a child confuses many parents. Especially parents of little girls. Because collecting material from an infant who is not yet familiar with the potty is not so easy. It is doubly difficult not to miss the first morning urine.
Remember a few important rules and strictly follow them:
1. There is no need to put off collecting tests until “tomorrow,” especially to continue in this spirit for several more weeks in a row.
2. Do not ignore your baby’s diet 2-3 days before testing.
3. Do not try to “decipher” the test results yourself - check them with the indicators that are printed on the forms incorrectly, because each child has his own indicators at different ages.
How to properly collect urine for analysis?
“Squeeze out a diaper or diaper” Unfortunately, this is a popular method, but completely unsuitable. As a filler for disposable diapers, a gel is used that absorbs moisture, which means that even if something is squeezed out, it will be a gel, and not urine for analysis. It is also pointless to wring out the diaper. Urine that has passed such a filter loses at least some of its properties.
“Pour from peas” Option, not the best. If your pot is made of aluminum, then at a minimum it must be boiled before collecting the child’s urine sample. It’s a total disaster with a plastic pot; even a “toilet duck” won’t help clean it. Collected urine, thus, even in a perfectly washed pot, will show a higher than normal number of leukocytes, and bacterial inoculation can completely shock you.
“Adapt a jar of baby food, seize the moment and substitute it” That’s better. But it all depends on the dexterity of the parents and the tractability of the baby. The jar with a lid must be prepared in the evening: wash it, pour boiling water over it and dry it. Immediately upon waking up, wash your baby. It is most convenient to carry out the urine collection procedure in the bathroom. Even the sound of running water from a tap can stimulate urination. It is also good to offer your child a drink of clean drinking water.
The most modern method, which has its pros and cons. A urine collector is a plastic bag with a drop-shaped hole and an adhesive substance that allows you to attach it wherever you need it. There are urine collectors that can be sealed immediately after urine collection and transported directly to the laboratory. Don't forget to wash your child before sticking the bag to the affected area. For greater convenience, we recommend putting a diaper on top. But the main thing: do not glue the urine collector “overnight”! Firstly, the baby relieves himself more than once during a night's sleep, and the package may contain such a mixture, the result of which may result in a referral for hospitalization. While the hospital will figure out whether the suspicions are unfounded, the baby can simply be treated for non-existent diseases. Secondly, the urine collector has a drawback - it can come off. In addition, many children manage to tear off the bag that is bothering them.
Children's tests "for the pool"
To visit the children's pool, you must take a certificate from the pediatrician, which is given based on the general condition of the child, the results of the baby's analysis of helminth eggs and enterobiasis.
Such tests of the baby are carried out based on the results of a scraping examination. The procedure does not require special preparation; it is performed in the morning, before bowel movement. You should not wash your child before giving a scraping. Lay the baby on his left side, bend his right leg at the knee and lift it slightly upward. Using a small special spatula or just a match with cotton wool soaked in glycerin, make a scraping and gently “rub” it on the perianal folds and lower rectum. In the material for enterobiasis, examined under a microscope on a glass slide, pinworm eggs are normally not detected at all.
To make a conclusion about the absence or presence of helminth eggs ("worm eggs" analysis, as this analysis is simply called), feces are examined. To get your baby tested a few days before, you should avoid taking activated charcoal, laxatives and iron supplements, do not use rectal suppositories and do not give enemas. On the morning of the test, collect about 2 tablespoons of your baby's stool from three different bowel movements. For transportation, we recommend using a special disposable container or just a clean, dry glass jar with a wide neck. The time it takes to deliver a child’s test to the laboratory should preferably be minimal. However, it is possible to collect stool in the evening (but no more than 8 hours before submitting it to the laboratory) and store it in the refrigerator until the morning.
TESTS FOR CHILDREN TO CLARIFY THE DIAGNOSIS
Biochemistry of blood To conduct a biochemical analysis of the blood of a child under 1 year old, blood is taken from a vein, the elbow or located on the child’s head. Medical specialists or a therapist can prescribe a test. An analysis is carried out to assess the functioning of internal organs and identify a particular disease at its early stage. It is necessary to carefully prepare for a biochemical study, not only for the baby, but also for the mother. The test is taken on an empty stomach, but many infants simply cannot afford not to eat for 8-12 hours. In this regard, the youngest should not be breastfed for at least 3 hours before the scheduled visit to the clinic. Sometimes laboratories require that children be given water to drink so that the venous blood becomes more liquid. As for the mother’s preparation, it is purely psychological. She may or may not be allowed to attend. It’s worth checking with the clinic in advance – these are internal rules. It would be a good idea for the mother who will be present to stock up on some valerian. Even an experienced nurse will not be able to get into the vein on a tiny hand or head the first time. To help your baby calm down, feed and cuddle him immediately after the procedure. Children forget grievances quite quickly when their mother is next to them.
For microbiological examination, feces for intestinal dysbiosis are collected in a sterile container, closed with a tight lid (for example, in a glass jar, sterilized and dried). The spatula for applying the material must also be sterile. The baby needs to be washed and somehow persuaded to pee, so that neither urine nor discharge from the baby’s genitals gets into the vessel. Flakes, mucus or pus that may be present in the stool, on the contrary, must be included in the sample. The most accurate results of the analysis of children are carried out on material delivered to the laboratory within 2 hours. In extreme cases, it is allowed to store materials in the refrigerator, but no longer than 4 hours before the study.
Baby tests for occult blood
This test is carried out if the baby is suspected of bleeding in any part of the gastrointestinal tract. The material is collected in the same way as for “worm eggs”. But the preparation is different. 3 days “before” the tests, it is necessary to exclude from food: meat, fish, liver and any foods that contain iron (including: apples, bell peppers, white beans, green onions, spinach), and vegetables that color feces ( for example, beets). You should avoid brushing your teeth, since even the slightest bleeding from the gums can distort the results, making them unreliable.
If infectious diseases are suspected, as well as pharyngitis and tonsillitis, tests are performed using swabs from the nose, pharynx and nasopharynx. Smears are collected on an empty stomach; you should not drink, rinse your mouth with water or brush your teeth before the procedure. It is painless for babies, but extremely unpleasant. You need to open your mouth wide, especially when taking a swab of a child from the nasopharynx. You can reach an agreement with older kids by asking them to be patient. But small children will have to be held tightly so that they do not twitch. Because they can hurt themselves or push the nurse’s hands, and if the swab accidentally touches the mucous membrane or tongue, the smear will have to be done again, and this will not work yet.
Child urine tests according to Nechiporenko
Nechiporenko urine tests of a child are carried out if deviations from the norm are detected in the results of a clinical test. It is necessary to determine the content of erythrocytes and leukocytes in order to diagnose inflammatory processes of the urinary system: pyelonephritis, cystitis, hidden hematuria and others. Nechiporenko urine tests of a child are carried out using morning urine. Before collecting the test, thoroughly wash the child’s genitals and prepare a sterile container. You need to collect the “average” portion of urine, that is, only the urine that occurs in the middle of the urination process is collected, and the beginning and end of urination are skipped.
Before any analysis of the baby you need:
1. consult with the doctor about the rules for collecting material and its delivery to the laboratory;
2. strictly follow the nutritional and dietary requirements, if any, before taking tests;
3. stop taking antibiotics no later than 14 days before taking the sample or warn the pediatrician and laboratory employee about taking them (however, it is worth warning about any medications you are taking);
4. prepare a container in which you will collect the material (when examining stool or urine): a sterile container, a clean jar with a lid or plastic packaging;
5. refrain from performing ultrasounds and x-rays on the child immediately before tests, as well as any physiotherapeutic procedures.
source
Indications
A clinical blood test is performed in several situations. Usually the procedure is done as prescribed by a doctor. Indications:
- the child’s complaints that cannot be explained do not go away for a long time;
- simple diseases do not go away for a long time, the condition worsens;
- diseases develop into complications;
- assessment of the severity of an already ill child;
- routine prophylaxis for all young healthy children;
- chronic course of certain diseases in children. In this case, blood is taken 2 times every 12 months;
- Sometimes they take an allergy test.
How often does this test need to be done?
Those who are interested in how often they need to donate blood for a general analysis should decide why these studies are being carried out. The need to donate blood to a child or adult usually arises when pathological conditions are suspected:
- when the temperature rises;
- malaise, body aches;
- the appearance of a rash and other changes on the skin;
- general weakness and other symptoms of disease.
It is advisable to obtain a referral for a planned (preventive) general analysis from a doctor, who will interpret the results and notify the patient about them.
Important information
Many parents are concerned about the correct blood levels in the child’s body. A general analysis examines: red blood cells, white blood cells, as well as hemoglobin, lymphocytes, monocytes, and other elements. They also determine the cell size, shape and maturity of red blood cells. Platelets are responsible for blood clotting. The number of these elements is determined using general analysis. Biochemical analysis from a vein helps identify triglycerides. Blood is also taken for allergies.
Below is a detailed transcript:
They participate in most processes: they deliver oxygen to organs from the lungs and remove carbon dioxide. Blood red cells get this color due to the fact that they contain hemoglobin. The norms depend only on age. Immediately after birth, on the 1st and 3rd days, the norms should be as follows: red blood cells - 4.0 to 6.6 × 10¹²/l.
On the 4th, 5th, 6th, 7th days the norm (erythrocytes) is 4.0 to 6.6 × 10¹²/l. Red blood cells at week 2 – 3.6 to 6.2×10¹²/l. If the standards are lowered, the child may develop anemia. It occurs as a result of various reasons, but ultimately weakens the body, since the organs are less supplied with blood.
If red blood cells are low, you should consult a doctor to prevent dangerous conditions and diseases.
In young children, the norms of cells such as red blood cells are rarely elevated. These are usually abnormal conditions called erythremia. The levels of erythrocytes in the blood can be high in case of heart disease, blood diseases, or dehydration of the entire body.
Parents also need to know about rdw. This is an indicator of heterogeneity in the volume of all red blood cells. Drawing blood for rdw helps determine the difference between small and large cells. As soon as cells of different sizes appear in the blood, anisocytosis begins. This happens with age, but sometimes the phenomenon occurs due to anemia or a malignant tumor. To rule this out, doctors recommend taking a blood sample to test for rdw.
Usually, children's blood is taken for RDW when a general analysis is prescribed. If there is a suspicion of illness or anemia, they may suggest taking blood from a vein and then do an rdw test. Typically, a blood test from a vein for rdw helps determine the type of anemia, as well as diagnose it.
Blood is drawn for rdw on an empty stomach, the analysis is taken from a vein. The rdw norm for children under six months is 14.9–18.7%; for a child older than one year, the rdw norm is 11.6–14.8%. If the rdw readings from the vein are high or low, an examination should be performed.
They are blood platelets. They do not live long, they exist for 2–10 days, then they are destroyed in organs, usually in the liver and spleen. Platelets perform an important function: they form a clot and close fragments of damage in blood vessels, preventing infections. Platelets stop bleeding and restore damaged tissue.
Normal blood levels of substances such as platelets:
- under the age of one year, platelets – 150–350*109/l;
- in children older than one year – 180–320*109/l;
- in newborns – 100–420*109/l.
If the standards are elevated, the child develops thrombocytosis. Usually occurs during major operations, anemia, unexpected bleeding, pneumonia, malignant tumors, and bone fractures.
There is another reason why platelets are high in the blood. The child's brain cells may not develop well.
If the norms are lowered, this demonstrates thrombocytopenia. Indicates an existing allergy to drugs. Sometimes reduced standards are a consequence of infectious diseases. This can also be influenced by the taking or transfusion of blood, which contains small amounts of platelets.
Important substances - lymphocytes are responsible for the immune system of the whole body. These are one of the main cells. This means that lymphocytes are able to produce protective bodies that protect the body from harmful bacteria and aggressive environments.
The norms for cells such as lymphocytes in children under one year of age are 50. At 4 years of age, the norms do not change. Lymphocytes also remain at the normal level of 50.
Sometimes lymphocytes can be high. Reasons why the rules have changed:
- infections;
- medications that caused hypersensitivity and allergies;
- diseases of the endocrine system, bronchial asthma, other diseases;
- periods of recovery after illnesses, operations;
- starvation, severe anemia.
- the child has flu, inflammatory processes;
- burns, injuries;
- major operations were performed;
- immunodeficiency;
- pustules, inflammation.
Lymphocytes are important substances in the body of infants, so you need to ensure that they are normal. Otherwise, the child’s body will not be able to resist diseases and infections, from which lymphocytes protect.
They are large areas of white blood. Monocytes perform an important function: they destroy bad microbes. Indicators that monocytes should contain:
If monocytes are elevated, this indicates a serious infection. This is why a general blood test is so important if children are diagnosed with the disease. Syphilis, malaria, tuberculosis - elevated monocytes may well indicate these serious diseases. Transcription will be required.
If monocytes in the blood are elevated, parents should be wary: the child may have a serious infection in a fragile body. Monocytes may also indicate existing malignant tumors. Monocytes may also be reduced. The standards are lowered if children have leukemia.
What other factors influence the result of the analysis?
Fat will raise your cholesterol levels, which will negatively affect your erythrocyte sedimentation rate. Donating blood during viral diseases will allow you to find out about the addition of a bacterial infection. However, other indicators may be distorted. Reliable results can be obtained 7 days after recovery.
It is better to refrain from a blood test if the baby had his teeth treated or had a gastroscopy the day before. You should not donate blood after an X-ray examination or physiotherapy - the number of leukocytes may increase. On the eve of the procedure, the baby should go to bed on time and get a good night's sleep. In consultation with the doctor, it is possible to discontinue some medications that the baby is taking.
According to recent studies, the time of eating before taking blood from a finger for a general analysis does not always distort the result. However, mother should not ignore this rule in order to avoid a false diagnosis and the need to repeat tests. If an additional examination is prescribed, blood is taken at the same time, since its morphological composition fluctuates depending on the period of the day.
In the process of diagnostic examination of a patient, one of the first things to be examined is blood - a liquid substance of the internal environment of the body, reflecting its condition. There is a clinical study for this called a complete blood count (CBC).
The result of the OAC is not one parameter, but a whole set of indicators, therefore, despite the small amount of blood taken for research, it can give a completely detailed picture of the pathological changes developing in the body. That is why a general blood test not only should not be neglected, but one should also prepare for it so that the final results are not distorted.
Biochemical analysis
Blood is usually taken from infants not only for a general analysis, but also for biochemistry - from a vein. This is especially important for a child, since some elements, such as triglycerides, may indicate Down syndrome. Therefore, it is important to periodically draw blood from a vein from a child and examine the indicators.
A little more about substances such as triglycerides. This is a person’s fat reserve, they accumulate energy. Triglycerides accumulate in special cells - adipocytes. Triglycerides enter the body through diet.
Triglycerides make up a group of lipids and are sources of energy. They are produced in the intestines and kidneys. Triglycerides help determine pathologies in the body, especially in children. The norms for children under one year are 0.34–1.5 mmol/liter. These indicators and interpretation are approximate; you should check the standards with your doctor before donating blood from a vein.
If triglycerides in a child’s body are elevated, this may mean that:
- the child has gained weight;
- lipid metabolism is disturbed. This can also happen at birth;
- improper functioning of the thyroid gland;
- Down syndrome.
If a child's blood triglycerides are elevated, you should consult a doctor, who may prescribe a more detailed diagnosis. If triglycerides have increased due to excess weight, a diet is needed, as well as fish oil. The baby will need serious physical activity.
Another important element is bilirubin. This is a bile pigment. When the baby is born, the standards for a substance such as bilirubin are even higher, since by this time the biliary system has not yet formed in children.
If metabolism is disrupted, bilirubin accumulates, leading to jaundice. Increased bilirubin in a newborn is normal, and you definitely shouldn’t worry about it.
- in newborns, bilirubin in the blood is 2.4–20.5 µmol/l;
- after a month, bilirubin should be from 3.4 to 20.5 µmol/l;
- in children older than one year, bilirubin is 3.4 to 17.1 µmol/l.
Bilirubin in the blood is usually exceeded for the following reasons:
- liver damage. Because of this, it cannot process incoming bilirubin;
- problems and disorders of the bile ducts. Because of this, bilirubin cannot be completely eliminated from the body;
- In children, liver secretion is impaired.
In case of disorders, bilirubin accumulates in considerable quantities, which leads to changes in skin color. It turns yellow and the baby develops jaundice.
source
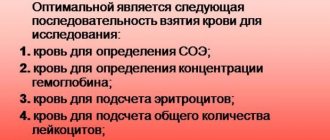
How is blood taken for general analysis?
Blood for clinical analysis in children is taken from a finger. Main indications for analysis:
- diagnosis of diseases based on complaints from the baby and his parents;
- upcoming vaccination;
- planned hospitalization;
- when prescribing drug treatment in order to select the correct drugs;
- prophylactically - carried out once a year.
Donate blood from a finger prick in a laboratory at a clinic or private clinic. You can call specialists to your home. This is especially true when the baby is sick or there is a surge in infectious diseases and you don’t want to expose the baby to the risk of infection. Children under 3 years old can be comfortably held in their mother’s arms during the analysis. She will hold the baby’s hand and calm her down. Older children can enter the office on their own, but it is better if up to the age of 10 they are accompanied by parents who will monitor the process.
Blood is taken from a finger using a disposable scarifier or lancet - a device for automatic painless puncture. It is easier to do it on the ring finger, since the skin there is very thin. The area is pre-treated with alcohol. After the puncture, the first drop is removed with a sterile ball, then blood is drawn.
The material is placed in test tubes, which are sealed and sent to the laboratory. A few drops are placed on a sterile glass and a smear is made. It is used for examination under a microscope. At the end of the manipulations, the puncture site is again lubricated with an alcohol wipe, which should be held for several minutes until the bleeding stops. The baby may be frightened by such actions of the laboratory assistant.
Indications for blood tests in children
The first time blood is taken from a vein from a child immediately after birth, and then a test is prescribed if a particular disease is suspected. The main types of tests that require venous blood are:
- biochemistry;
- determining blood sugar levels (we recommend reading: normal blood sugar levels in children by age);
- serological analysis;
- allergy tests;
- blood type and Rh factor.
In other words, there must be serious reasons for sending a blood test from a vein. The study allows us to identify such serious diseases as hepatitis, diabetes, and infectious lesions. To obtain the result, 5 ml of material is usually enough.
If parents turn to an allergist due to the fact that the child constantly shows a reaction to irritants (skin peeling, rashes, itching), the doctor will also issue a referral for a venous blood test. The material is also taken if the baby has a predisposition to asthma. Blood is studied for sensitivity to hundreds of allergens at once, a list of which is compiled individually for each patient.
Parents should know that not all laboratories do extensive allergen testing. You should study this issue in advance and choose a suitable clinic to donate blood and get a complete picture of the baby’s sensitivity to external stimuli.
Serological testing is required to detect infectious diseases. These include toxoplasmosis, mumps, rubella, herpes, and measles. Only after receiving the results can a specialist prescribe effective treatment.
A blood sugar test is carried out if diabetes is suspected. This analysis is also important in cases of pancreatic dysfunction. for signs of epilepsy (we recommend reading: the main signs of epilepsy in children). A test for Rh factor and blood group is done in an emergency, for example, before a blood transfusion procedure.
How is blood taken from a baby and how to prepare for the test?
Although today few mothers adhere to a strict feeding regime, on the day when the baby needs to donate blood for a general test, it is worth calculating the feeding time so that the OAC procedure falls on the period between the first and second feeding.
It is imperative for the mother not to worry, not to fuss, not to get nervous over trifles, the procedure is simple, does not require much time, everything will be over before the child has time to get scared. This attitude has a very positive effect on the child and greatly facilitates the manipulation.
Features of the structure of blood vessels in infants
The structure of veins in an adult and a child is very different. With age, the position of the veins located as close as possible to the surface of the skin changes. In infants and one-year-old children, the internal venous network is dense, so the superficial veins against its background are difficult to see or are not visible at all. The search for veins is also complicated by the fact that the youngest patients have well-developed subcutaneous adipose tissue, which is loose in structure.
The structure of the vessels themselves also varies at different periods of a baby’s life; some features of their structure are characteristic of all children under one year old. For example, in them, unlike adults, the walls of blood vessels are not divided into three shells, which is why they are less elastic and more fragile. Due to low pressure in the vessels, blood flow is reduced, which is why the procedure for taking material from a vein may take longer.
Leukocytes
Leukocytes (white cells) are round-shaped cells with a central nucleus that take an active part in immune reactions. They carry out phagocytosis (capture and digestion) of pathological microorganisms, toxins and decay products. The norm of leukocytes is – 5.5 – 12.5 x 109/liter;
An increase in the number of white cells, leukocytosis, in a child under one year old may indicate:
- development of pathologies of an inflammatory or infectious nature (the higher the indicator, the higher the severity)
- tumors
- blood diseases
- kidney failure and so on
What needles and syringes are used for babies?
The choice of syringe for drawing blood from a child depends on the amount of blood needed for a particular type of analysis. Currently, laboratories have a wide range of instruments for collecting material. There are various syringe tubes and entire systems for vacuum blood sampling, which differ in the color of the caps. Each of these tubes already contains a specific preservative reagent for research.
The principle of operation of vacuum tubes is simple: there is a vacuum inside, which will not allow blood to flow from the vein in a larger volume than required. Thanks to this, the tube is filled in a matter of seconds. The system's needle does not allow blood to come into contact with the external environment, so foreign impurities cannot get inside and affect the reliability of the analysis.
Syringe tubes for vacuum blood collection
The test tube needle has a special silicone coating, which makes it easier to insert into a vein and makes the process of collecting material more painless. A huge advantage for the laboratory specialist is that the test tube system is equipped with a rubber gasket to prevent backflow of blood, so contact of the material with the skin of the healthcare worker is minimized.
How is blood taken?
Blood from a vein is donated only on an empty stomach, so it is best to take a small child for analysis in the morning, and immediately feed him after collection. The baby’s hands should not be cold, especially at the point where the needle was inserted, then the laboratory technician will take the right amount of material the first time without any problems.
Blood is drawn in the same way as in adults - from the elbow. First, the desired area is treated with an alcohol swab, then a tourniquet is applied to the arm above the elbow. For older children, the nurse may ask you to clench and unclench your fist several times. A needle is inserted into the vein, then the tourniquet is removed, after which the required amount of blood is drawn into the syringe. After the procedure is completed, the injection site is again treated with an alcohol solution and then sealed with an adhesive plaster.
Where do you get clinical CBC from?
The results of the study are not affected by where the blood is taken for clinical analysis. Many laboratories find it more convenient to take blood from a vein.
Devices such as scarifiers have not lost their relevance either. They are designed to pierce the pad of the ring finger, where capillary blood is taken. Scarifiers must also be sterile, individually packaged and disposable.
A more modern version of the piercing device is the so-called lancets. These medical products are more expensive than scarifiers. They resemble plastic fountain pens with springs inside, ensuring that a sharp needle “shoots” from the rod strictly to a certain depth. Lancets are most convenient when you have to donate blood to a child, since, thanks to the special sharpening of the needle, they ensure almost complete painlessness of the manipulation.
How to make the procedure less painful?
In the process of donating blood from a vein to an infant, two factors are of great importance: the qualifications of the medical worker and the psychological preparation of the parents. It is important to take a responsible approach to choosing a clinic and study customer reviews about the training of staff, and also convince yourself that the upcoming procedure is a common thing and you should not panic.
Often, a child may be frightened not by a laboratory technician with a needle, but by a mother shaking with fear. Some laboratories even practice the process of donating blood without the presence of parents. Specially trained personnel carry out the procedure as quickly as possible with minimal risk of injury, so the baby will not even have time to get very scared.
If parents are with the child during blood sampling, you should think in advance about how to distract him. The big plus is that the baby does not realize what exactly he is about to experience, therefore, if you fully occupy his attention, he will only feel a slight discomfort at the time of the injection, because fears are only in our heads. It would be a good idea to take your child’s favorite toy with you or turn on his favorite cartoon on his phone or tablet.
You can work out the procedure at home: the parent choose the most comfortable position in which it will be convenient to hold the child on his lap, and find an activity that the baby will like. The main thing is that this should not interfere with the laboratory assistant doing his job.
Can a child eat before donating blood?
In order for the result of a child’s routine blood test to be accurate, you must adhere to certain rules: donate blood in the morning (7–11 am) and on an empty stomach. Most experts believe that eating even a small amount of food leads to an increase in the number of white blood cells, which makes diagnosis difficult. Other doctors believe that there is no reason to torture the baby with prolonged fasting; they recommend abstaining from food and drink 3 hours before the procedure.
The question of whether children can eat before a blood test or not is decided individually depending on the age and health status of the baby. The general rules are:
- It is difficult for babies under one year to withstand long breaks between feedings, so it is recommended to donate blood in between. For example, a mother feeds her baby at 6 and 10 am. The best time to submit biomaterial for analysis is about 8 hours. Blood is taken from newborns at any time.
- For children older than one year, the sampling is carried out strictly on an empty stomach. An exception is made for children who suffer from pancreatitis and diabetes. Such children are allowed to eat a small portion of porridge with water or crackers with tea 2–3 hours before the test. The rest of the children are not even allowed to drink water. If your baby is thirsty, you can rinse your mouth with water, but do not swallow. Immediately after the procedure, the child should be fed well.
- The day before the procedure, you should not tire your baby out with physical exercise or feed him sweet, starchy, spicy or salty foods. A calm atmosphere in the home and the psychological preparation of the baby are important. You should not deceive the baby by saying that it will not hurt. It should be said that you need to be patient, because what the doctor does in the medical office is important for the health of the baby.