A clinical blood test includes a complete blood count (hemoglobin, red blood cells, platelets, etc.), leukocyte count, and ESR.
A clinical blood test is a primary test that helps in the diagnosis of various diseases.
Considering that the safety of our little patients is our top priority, at the Sanare Medical Center we use only disposable materials (gloves, scarifiers - lancets, test tubes) to take blood tests.
We care about our patients, so we use exclusively low-impact lancets to take a finger prick (capillary blood) test in our treatment room. Lancets are modern automatic devices that have replaced the metal “spears” - scarifiers, which were used for many years to draw blood from a finger.
The use of a lancet has significant advantages: the volume of blood required for analysis is provided, finger tissue is less injured, pain is significantly reduced (when drawing blood, the nurse does not apply force, the lancet mechanism is activated automatically).
Also, during the procedure, children do not see the needle, which causes discomfort while waiting for the injection.
A special needle is housed in a plastic case, ensuring sterility and safety for both the patient and the medical staff collecting blood. The device is equipped with special “antennae” - protective mechanisms that make reuse of the lancet impossible.
Taking blood from a finger, donate on an empty stomach or not and how to prepare
During the next appointment with the doctor, it was prescribed to donate blood from a finger prick. But the patient forgot to ask how to take it correctly in order to get the most reliable result. And are there any food restrictions on the day before the test? Can I have alcohol? And why does the blood change in general, and how will it affect it? They take very little there. Let's take a closer look.
Getting ready for delivery
First of all, it’s worth figuring out why you donate blood from your finger. In any case, finger blood is given on an empty stomach and before 11 am, but there is a slight difference in the hours of fasting before donation. The minimum number of hours after the last meal is 7-8. If you need to identify lipids or take a glucose tolerance test, then your last meal should be no less than 13-16 hours ago. This is important, as it can blur the real picture of the body’s condition, and the doctor will prescribe unnecessary medications, seeing a distorted picture of reality.
In the morning you cannot eat or drink anything except non-carbonated pure mineral water. You cannot drink coffee, tea, sweet soda or compote. This will especially affect glucose and diabetes tests. You should not drink alcoholic or toxic drinks on the eve of the test, and especially in the morning. This not only harms your health, but also turns reliable results into false ones, which will have to be taken again.
Is it necessary to donate blood from a finger prick on an empty stomach? Of course, otherwise all the results will be either completely or partially incorrect.
If you have to donate blood several times at regular intervals, you should try to donate each time at the same time and at the same time on an empty stomach.
You should not eat fried, salty or spicy foods the day before the test. Also, you should not dramatically change your diet on these days. After all, significant changes in a person’s routine can also provoke strange changes in the blood for a short period. For example, if a person has never eaten spicy adjika, then the evening before donating blood, you should not start consuming it. It is advisable to avoid heavy physical exertion and emotional stress. A break in food at the time of donating blood should not exceed 16 hours, as this will provoke undesirable consequences and the release of toxic substances into the blood.
If the patient takes certain medications daily, then you must tell the doctor about their use, who will clarify whether they need to be stopped before donating blood.
In no case should you voluntarily discontinue vital medications, which may not even affect the parameters being studied.
Also, do not rub your hands or fingers before drawing blood. This will increase white blood cells, which will spoil the results of the study. You should not take it immediately after running or long brisk walking. Any stress that affects breathing requires at least minimal rest before donating blood.
Donating blood by a pregnant woman
There are several recommendations that should be followed by a pregnant woman who is going to donate blood from a finger prick on an empty stomach. How to donate blood from a finger on an empty stomach during pregnancy:
- If you are taking any medications, you should ask your doctor when they are eliminated from the body so that you can take the medication on time and by the time of the test so that it has time to be eliminated.
- If the path to the laboratory was long, then you should sit for a few minutes near the laboratory, calm down, restore your breathing and balance, and then go into the room.
- If you feel excessive stress, fatigue or extreme agitation, then donating blood should be rescheduled to another day when your health condition becomes stable.
- If tests and procedures are scheduled for the same day, you must first donate blood so as not to put unnecessary strain on the body before taking the test.
- If it’s completely unbearable, then a pregnant woman can have a little snack. The main thing is to remember that some foods cause increased cholesterol, inflammation and infection in the blood.
Important factors when donating blood will be not only the time of hunger, but also the period of pregnancy of the girl. These factors influence hemoglobin along with the appropriate menopause. Regular blood donation is absolutely necessary if a pregnant woman has chronic problems with internal organs. Using this analysis, you can evaluate many metabolic processes that occur in the body of a woman of reproductive age.
Color and character of blood
In order to correctly interpret the meaning of some dreams, it is sometimes very important to notice their details, for example, the color of the blood or its condition. Why dream of your own blood on your hand or elsewhere if it is black? In this case, dream books promise the sick person recovery, but a healthy person may be overtaken by minor troubles, but they will not cause much harm. Scarlet blood foreshadows love affairs
However, not everyone believes in this
Scarlet blood foreshadows love affairs. However, not everyone believes in this.
Thick blood indicates the likelihood of problems in your relationship with your significant other, which may cause some stress. If you dream of burgundy clots, this means losses, as well as troubles in work and personal life.
By the way, a dream in which you see something that has a blood-red color can be a very bad sign. This may be followed by a big disaster that will be difficult to avoid.
How to donate blood with baby
All children have to donate blood. First in the maternity hospital, then usually at three months and a year, unless otherwise prescribed. Also, sometimes the pediatrician prescribes a blood test if he sees something suspicious in the child’s behavior - he is not gaining weight well, he is restless or nervous. Tests are taken to find the reason for the baby’s behavior. Finger blood is donated on an empty stomach by children who have been prescribed a serious vaccination. This is done to identify possible poisoning or inflammation in the body and not to aggravate the condition with vaccination.
It is not recommended to feed your child before donating blood, as this may distort the results obtained. If you do not comply with this common-sense requirement of medical personnel, then there is a possibility of receiving unreliable tests. Such blood samples usually have significantly higher white blood cells or lower hemoglobin levels.
Attention! The baby should not be sent for blood donation after an X-ray, ultrasound or physiotherapy.
If all this is scheduled for one day, then first of all you need to go to donate blood. If this is possible, the child should sit quietly for some time before being admitted to the laboratory, gain strength and get normal blood counts.
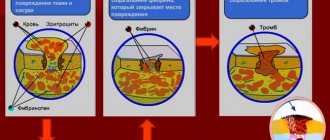
In newborns up to five days old, the results can vary greatly - both a hemoglobin level of 110 g/l and 240 g/l are considered normal. The older the child, the closer his indicators are to normal in adults. An extremely important indicator is an acceptable number of platelets, which impede blood clotting. And ESR is the rate at which red blood cells settle. If the ESR results are exceeded, this indicates the appearance of inflammation or an acute infection.
Products: which ones you should eat and which ones you shouldn’t eat
There are a number of products that will help improve blood composition and eliminate the need for electrophoresis. It is worth paying attention to rutabaga. This plant is unpretentious and rich in large amounts of protein, iron and expectorant properties.
Eating foods such as fatty meats and dairy products before donating blood will cause fats to appear in the blood. And you should not use mayonnaise and margarine at all, especially before donating blood. It is worth limiting your intake of honey, as it contains a lot of glucose.
Don't pay attention to products that have a lot of white parts. The glycemic index may well rise due to eating bananas and green grapes.
It is also forbidden to eat too sweet foods - cake, assorted pastries and jam. You should not smoke at least one hour before donating blood. Before entering the office, you can drink a glass of cold water. This will help you feel more confident and at ease. Try to relax and not think about what is happening at the moment.
source
Blood on the face or coming from the mouth
Seeing blood coming from your mouth in a dream means that soon you will have to defend your point of view in front of your relatives. In disputes, watch your words, because what you say can be regretted. Show interest in your health, go to the doctor, get examined if you are spitting blood in your dreams. If in your dream a stranger is overcome by a bloody cough, then you should refrain from making new acquaintances and exclude participation in dubious events. This can be very risky.
But blood on the face, apparently, predicts success in business and financial well-being. You may soon have a new source of income. If in a dream you see blood on your head, this may indicate that you or someone from your environment is under pressure from superiors or relatives.
If in a dream you happen to see blood coming from your eyes, you will probably be disappointed in a loved one in the future, or you may be deceived, which will be very unpleasant.
Finally, it is worth noting that dreams should be interpreted along with an analysis of your life situation. When wondering why you dream of blood on your hands, face, clothes, try to remember how your relationships with your relatives are, put your affairs in order and take care of your health, and also take an interest in the well-being of your loved ones. And most importantly, don’t worry, because only with a clear mind can you overcome all difficulties and truly enjoy your success!
Other articles:
How to get into a lucid dream (3 photos)
About dreams and visions. Symbols in dreams, psychology of dreams (3 photos)
A dark circle was spotted again on the ice of Lake Baikal (4 photos)
Why do a general blood test?
The general analysis itself is quite simple, but informative. Blood from the finger of both a small and an adult patient is taken to determine many of its indicators:
- Sugar level, more precisely glucose (we recommend reading: normal blood glucose levels in a child by year). The main conclusion regarding this parameter is whether or not there are signs of diabetes in the body.
- Platelets are indicators of blood clotting characteristics (we recommend reading: reasons why platelets in a child’s blood may be elevated).
- Hemoglobin will tell you how oxygen circulates in tissues and organs (we recommend reading: what should normal hemoglobin be like in newborns?). Its norm or deviation will indicate dehydration, malfunction of the lungs or heart, the body’s adaptation to changed conditions (for example, among athletes), and poisoning. Most often, hemoglobin levels are tested to find out whether a person suffers from anemia - a lack of iron in the body.
- Monocytes are indicators of the fight against inflammation (we recommend reading: reasons why monocytes are elevated in a child’s blood).
- Leukocytes are the shield of immunity. Their abnormal number will indicate the presence of an infectious attack on the body.
- Eosinophils are cells that signal allergic reactions, purulent infections, and the introduction of parasites (we recommend reading: why are there elevated eosinophils in a child’s blood?).
- The ESR parameter determines the erythrocyte sedimentation rate (we recommend reading: what level of ESR in a child’s blood is considered normal?). The indicator is important in diagnosing inflammation and pathologies.
What is a lancet?
Most often, disposable scarifiers are used in medical institutions. In order to make a puncture with their help, you need to apply a certain amount of force, which may seem excessive and painful to a small child.
The lancet is an excellent alternative to an unpleasant procedure. It is an automatic device that allows you to painlessly puncture the skin. No effort is required to complete the process.
The operating method of the device is simple. The lancet has a durable plastic body containing a set of sterile needles. Upon contact with human skin, a small needle extends, which instantly makes a small puncture. There are other models in which the needle appears when you press a button located on the plastic body. The location of the piercing device is covered with a plastic rotating cap.
Basic rules for preparing for analysis
In order not to distort the results of the study, many experts prohibit eating before donating blood from a finger prick, but there are other factors that can affect the result. For example, it is affected by certain medications that a small patient may be taking. To make the analysis informative, prepare for it in advance:
- A visit to the laboratory is planned for early morning, preferably from 7-00 to 10-00. Many laboratories work until 12-14 hours, but it will be difficult for a child who has not had breakfast to wait for this time. In addition, in the afternoon, blood counts change.
- Before blood sampling, no visits to the X-ray room or physical procedures are planned. This affects the result.
- The interval between the last meal on the eve of the test and the blood sampling procedure is 12 hours. An abundance of sweets, baked goods, and fried foods in the diet is prohibited. Otherwise, the laboratory picture will change, especially regarding the number of leukocytes.
- It is allowed to drink clean water in moderate portions without additives, dyes, preservatives and sugars. Teas, compotes, fruit drinks, decoctions, and milk are also prohibited.
Before taking a general blood test, you are allowed to drink clean water in small quantities.
- In case of ARVI, the test is prescribed to determine the complexity of the course of the disease - it is taken as directed by the doctor. When there is a planned visit to the laboratory, during an acute period of respiratory diseases it is canceled and postponed for 1.5-2 weeks from the moment of recovery.
- It is better to exclude any worries before the procedure and cancel training with increased load.
- After operations and major interventions, the study is planned a week later.
The laboratory assistant or doctor should be notified of any deviations from the rules. If the patient is taking medications that may affect the interpretation of the analysis, the doctor will advise on what can be done in this case. Sometimes a break in therapy is allowed.
Features of blood sampling for general analysis in infants
As in other cases, to perform a clinical analysis, capillary blood will be taken from the baby from a finger.
The rule “not to eat before donating blood” does not apply to babies in their first year of life!
Children under 1 year of age are not required (and most often impossible) to go without food:
- Newborns will have to undergo blood tests more than once in the first week of life. There is no question of abstaining from feeding the baby.
- It is impossible to explain to babies under one year old why they were not fed before the painful procedure. Breakfast is a must for them - milk, porridge, vegetables, lean meat, depending on what the baby is accustomed to eating. Then there is a break of 3 hours, and you can go to the laboratory. The algorithm is this: wake him up early, feed him, go for a walk and wait the right time, go and donate blood.
- Psychological preparation before taking the exam is important. In the evening, the baby is offered a quiet game or shown a cartoon with a doctor character. In the morning they tell him where they are going and why. Be sure to buy a children's scarifier for drawing blood.
Methodology
Capillary blood collection technique
Also, the correctness of the result depends on the accuracy of following the algorithm for taking blood from a finger:
Respecting the patient's right to information, inform him about the progress of the subsequent procedure, obtain the patient's consent for it. Prepare the necessary equipment for examining blood from a finger on the hand (cotton balls - dry and moistened with 70% ethyl alcohol solution, sterile disposable scarifiers - spears or sterile needles, labeled sterile disposable pipettes, clean slide (watch) glasses or, instead, clean plastic tablets, labeled clean test tubes with an anticoagulant, a container with a disinfectant solution for soaking waste material). Carry out hygienic and antiseptic treatment of hands, wear clean gloves. Treat the ring finger of your left hand with a sterile cotton ball moistened with a 70% solution of ethyl alcohol. Using a sterile scarifier or a sterile needle, make a puncture 2–3 mm deep (if the puncture is deeper, it will be more difficult to stop the bleeding). Wipe off the first drop of blood that appears with a sterile dry cotton swab. The next few drops of blood (at least 3 - 4) are dropped by gravity onto an individual glass slide (pressing on your finger to obtain blood is prohibited, since the blood is mixed with tissue fluid, and the analysis results may be distorted). Using a disposable sterile pipette, take 6–8 drops of blood, then carefully move it into a labeled tube with an anticoagulant. Blood can be drained into a test tube by gravity. Using the test tube in a circular motion (at least 10 times), thoroughly mix the collected blood with the reagent. Press a sterile cotton ball moistened with a 70% ethyl alcohol solution to the finger at the puncture site and advise the patient to hold it until the bleeding stops completely. Move the marked glass slide containing biological blood samples to a special table for analysis, and place the marked test tube in a special rack. To maintain infection safety, soak all used consumables in a container with a disinfectant solution.
Should a child over one year old donate blood on an empty stomach or can he be fed?
A general blood test for children over one year old is taken on an empty stomach - this is an unbreakable rule. It applies to both children and adults. The attending physician needs real indicators of how the patient’s body works.
If there is a suspicion of an infectious process, inflammation, or exacerbation of a chronic disease, then this is exactly what the doctor will confirm or refute through analysis. If the patient is getting better, this should be visible in the study results.
Example: a child was fed before the study, food components, when absorbed into the blood, caused a change in its composition, affecting viscosity, leukocyte formula, the ratio of proteins, fats, and more. In the transcript, the doctor sees signs of an inflammatory process that are not actually there. Therapy is prescribed that is unnecessary and dangerous for the patient. This outcome will not please any parent.
It’s good if the doctor finds out the reasons for the false readings. If not, then additional examinations and procedures may be prescribed, which is tiring for the baby and ineffective in general.
An exception is made only for young patients suffering from diabetes mellitus and pancreatitis (we recommend reading: features of diabetes mellitus in children and treatment). Long breaks between meals and donating blood on an empty stomach are contraindicated for them. Before blood tests, such children are recommended to eat a small portion of cereal porridge with water, fresh vegetables or crackers, and cheese.
The conclusion is simple - all other categories of children (over 1 year old) undergo a general blood test strictly on an empty stomach, subject to simple rules. Children are prepared in advance for the procedure and its importance is explained. To make everything go smoothly, the visit to the laboratory is made early in the morning. Then the baby can and should be fed.
source
Device modifications
There are two types of lancets on sale: automatic and universal.
Universal
Universal devices are suitable for any portable glucometer handle (except for the Accu Chek Softlix device). They are intended for use by children and adults with diabetes. The tool itself is disposable, and the pen in it is protected by a safety cap.
Some manufacturers supplement this lancet with the function of regulating the depth of invasion. This is convenient if you need to measure the sugar level of a small child with thin and delicate skin. Such devices are sold in packages of 100-200 pieces, because measurements in diabetes have to be done several times a day.
Automatic
Automatic lancets are equipped with disposable needles. The depth of the puncture does not depend on the skill of the laboratory assistant; it is set automatically. After use, the pen is thrown away or placed in a special compartment. In most models, the needle itself retracts back into the body after the procedure. Some models have a replaceable drum for storing needles.
Pen diameter and length
The diameter of the needle depends on the type of device and is 0.25-0.8 mm, and the length is 1.2-2.4 mm. For a child's finger, a needle with a length of 1.5 mm and a diameter of 0.5 mm is usually used. Such a miniature size and triangular shape allows you to make a puncture without pain, but at the same time get a sufficient amount of blood.
Table of lancet types:
| Needle length, millimeters | 1,2 | 1,5 | 1,8 | 2,0 | 2,4 |
| Needle diameter, millimeters | 0,25 | 0,5 | 0,8 | 0,8 | 0,8 |
| When to use | For small children with thin skin and for diabetics | For general analysis of sugar in children and adults | For collecting large amounts of blood, e.g. for coagulation or gas tests | For taking blood from the heel of newborns | For people with very rough skin and for collecting large amounts of blood |
How to properly take a complete blood test for a child
When the baby gets sick, parents call a local pediatrician at home or take the baby to a district or private clinic. After examining a small patient, pediatricians give directions for tests in order to better understand the cause of the disease and prescribe adequate treatment. Other tests include a blood test.
Many babies simply do not respond to blood sampling
Indications for use
In most cases, a blood test is prescribed for newborns for any of the following indications:
- the impossibility of making a diagnosis based on symptoms alone;
- atypical course of the disease;
- the occurrence of complications;
- the need to assess the effectiveness of therapy.
In addition to the above, hematological studies are also carried out for preventive purposes. For healthy children, the frequency of blood sampling is once a year, and for those suffering from chronic pathologies - 2-3 times a year. The frequency of testing is determined by the attending physician.
Why donate blood on an empty stomach?
When doctors say that newborns need to donate blood on an empty stomach, it is assumed that no useful substances will enter the child’s body before the procedure. If you do not properly prepare and feed the baby, the result may be distorted. When a baby eats something, the incoming substances immediately begin to be absorbed, triggering a biochemical process, as a result of which blood composition indicators change.
If you find an approach to a child, taking his blood for analysis will not be difficult
Typically, the following hematological tests are performed before meals:
- general;
- biochemical;
- for sugar;
- for hormones;
- serological;
- for tumor markers.
Important! When a child needs to donate blood, it is important not only not to feed, but also to try not to give him water. Such an action will lead to activation of the enzyme system, change blood viscosity and may change hormone levels. All this will affect the substance under study, and the results obtained will be unreliable.
Tool manufacturers
In the market of medical products that produce devices for painless blood collection, the following stand out: HTL-Strefa, Vitrex Sterilance, MiniCollect, Suyun Medical Materials.
1. HTL-Strefa is a Polish company that produces MedlancePlus lancets. The company has in its assortment six types of products, each of which is colored in its own shade.
2. Vitrex Sterilance is another manufacturer that has earned recognition among buyers. The company produces four types of automatic scarifiers.
3. MiniCollect is an equally popular manufacturer. It presents four types of product, the diameter of the needles varies from 1 to 2 mm.
4. Suyun Medical Materials is a manufacturer that produces scarifiers not only for adults, but also for children. It presents four different options for different skin types and uses.
Is it possible to eat before taking a general analysis?
If it is quite possible to explain to a child of five or eight years old why they refuse to feed him before visiting the hospital, then finding a way for an infant to donate blood on an empty stomach is much more difficult. Due to the fact that an infant cannot withstand a long break without food, the following algorithm of actions is proposed:
- Wake up your baby a few hours earlier than usual;
- Feed the child breakfast (food should not be fatty);
- Wait three hours;
- Go to the laboratory.
As soon as the baby turns one year old, doctors categorically begin to insist that blood donation be done on an empty stomach. Exceptions are possible only for those small patients who suffer from pancreatitis or diabetes, and long breaks in meals can be fraught with serious consequences for them. Before laboratory analysis, such children are recommended to eat a small portion of any cereal porridge cooked in water.
Babies are often frightened not by the blood draw itself, but by the presence of a stranger
How and where to get tested for biochemistry
Most parents learn how to properly take a general blood test for a child in the first days of his life. Not everyone knows how to donate blood to a baby for biochemistry.
The general rules for preparing for a laboratory test for the biochemical composition of blood and a general analysis are actually almost identical. Before visiting the hospital, you should follow these simple recommendations:
- for children over one year old - refrain from eating for at least 12 hours before blood sampling;
- plan a laboratory visit for the morning;
- It is allowed to give the child something to drink, but only with plain water;
- try to distract the baby and prevent him from getting excited before the procedure;
- Eliminate taking any medications for about a week (if possible) or tell the doctor what medications your baby is taking.
It is equally important to choose the right laboratory whose specialists will draw blood. It is important to pay attention to the following points:
- Deadlines for issuing finished results. Parents have the opportunity to choose between two options: standard (5-10 days) and express (less than 2 days). An urgent biochemical analysis will cost more, but when a newborn baby gets sick and an urgent diagnosis is required, any delay can lead to fatal consequences.
- Professionalism and competence of employees.
- Equipment quality.
For the analysis of biological material, a little more is always taken than necessary
Important! Before contacting the laboratory, you should definitely make sure that the selected medical center provides interpretation of the tests.
When answering the question about a biochemical clinical blood test, how to give it to a child, you should pay attention to the fact that it is recommended to do it in the morning. It makes sense to choose a laboratory closer to home so that the baby does not have time to get tired on the road and become capricious.
How to take a general blood test
Parents most often learn how to donate blood to a baby through a general analysis. This is the main type of research that is most often used when making diagnoses.
Blood sampling may be carried out differently in individual clinics. In some laboratories, capillary blood is taken for testing, in others - venous. The first option is more common. This is due to the simplicity of the procedure. A finger or (if the child is a newborn) heel is pierced to collect blood. The disadvantage of capillary blood is that it quickly coagulates and forms clots, which can lead to distortion of the result.
It is worth donating blood in a reliable clinic with good specialists
Venous blood is more suitable for general hematological research. The only reason why newborns rarely undergo such a procedure is that not every nurse can take blood from a vein painlessly.
Important! The first general blood test is taken from the baby in the maternity hospital.
Regardless of where the blood is ultimately taken from infants at 1 month, the procedure turns out to be associated with quite serious stress for babies. Much depends on how parents and medical staff behave. If the child is very nervous, the test result may be unreliable.
A relatively adult child should be explained that taking blood for analysis is not painful, but necessary. During the procedure itself, you should try to distract his attention to something.
Automatic scarifier (lancet) MEDLANCE Plus
An automatic disposable sterile scarifier is used for modern, painless collection of capillary blood from patients in hospitals, clinics, veterinary clinics and other medical institutions. The ultra-fine needle of the automatic lancet penetrates the skin easily and quickly, which reduces pain, prevents damage and accelerates wound healing. The device is in convenient contact with the puncture site, and the procedure is completely safe for both medical personnel and the patient. In an automatic scarifier, the needle is located inside the device, both before and after use. This eliminates the possibility of harm, accidental use and the risk of medical personnel coming into contact with blood. In addition, all modern lancets are sterilized, which makes their use safe for patients and staff.
The sterile disposable lancet Medlance plus has an ultra-thin needle of different sizes (G25, G21 and 0.8 mm feather) which very easily penetrates the skin, and different depths of puncture of the patient’s skin, since the pressure at the puncture site is strictly calculated. This ensures complete and definitive control of the penetration depth and the availability of a sufficient amount of blood sample.
Medlans Plus Lite (MEDLANCE Plus Lite)
Needle: 25G Puncture depth: 1.5 mm. Recommendations for users: Suitable for all categories, ideal for monitoring blood sugar levels. Blood flow: Low
Medlans Plus Universal (MEDLANCE Plus Universal)
Needle: 21G Puncture depth: 1.8mm Recommendations for users: Suitable for when a large blood sample is needed to measure glucose, hemoglobin, cholesterol, and blood group, coagulation, blood gases, etc. Blood flow : Average
Medlans Plus Extra (MEDLANCE Plus Extra)
Needle: 21 G Puncture depth: 2.4 mm Recommendations for users: Suitable for patients whose skin is too rough or a large blood sample is needed (men and people engaged in manual labor). Blood flow: Medium to high
MEDLANCE Plus Special, blade
Needle: blade - 0.8 mm. Puncture depth: 2.0 mm. Recommendations for users: Suitable for collecting blood from the heel in infants and from the finger in adults. The ultra-thin pen of the Special scarifiers allows you to collect the required volume of blood and promotes rapid healing of the puncture site. Blood flow: Strong
Video instructions for use Packaging: 200 pcs. in original factory box. Shelf life: 5 years Manufacturer: “HTL-Strefa. Inc.”, Poland
Scarifier (lancet) automatic price
| Name | Needle | Puncture depth | Photo | Package | Price per package |
| Medlans Plus Lite (MEDLANCE Plus Lite) | 25G | 1.5 mm | 200 pcs. | RUB 1,400.00 | |
| Medlans Plus Universal (MEDLANCE Plus Universal) | 21G | 1.8 mm | |||
| Medlans Plus Extra (MEDLANCE Plus Extra) | 21G | 2.4 mm | |||
| MEDLANCE Plus Special, blade | blade - 0.8 mm | 2.0 mm |
Drawing blood from a vein or finger
The decision as to where the baby's blood should be taken from is made by the doctor. Capillary blood is usually taken in the following cases:
- during medical examination during a general health check;
- to obtain help;
- if anemia is suspected;
- to assess the condition of the blood after treatment.
Venous blood will be required under the following circumstances:
- if a serious systemic disease is suspected;
- in conjunction with other research;
- to obtain more reliable information after poorly performed capillary blood sampling.
Interesting. Venous blood in newborns is most often taken not from the arm, but from a vein in the head. This is due to the fact that the vessels are much better visible in this place.
In infants, venous blood is taken only in exceptional cases, since the risk of tissue damage and infection in a fragile body is too high. If there are no special indications, doctors limit themselves to analyzing capillary blood taken from a finger or heel.
There are clear rules regarding the collection of hematological material for research in infants. We are talking about the following significant points:
- The baby's last meal should take place several hours before the procedure.
- The limb from which blood will be drawn must be warm (this will speed up blood circulation).
- The surface to be punctured must be thoroughly treated with an antiseptic liquid or alcohol.
- Antiseptic treatment is repeated after completion of the procedure.
- After disinfection, the puncture site is sealed with a bactericidal adhesive plaster.
Important! When taking fluid from a vein on the head, a tourniquet is not applied.
If all the rules for collecting blood from a baby are followed, there is no danger to the child. Even if a nurse accidentally pierces a vein, the hematoma that forms will resolve over time without complications. There will be no risk to health, since no medications are administered during the blood test.
To carry out a general blood test, 1 ml of blood is enough. Typically, the volume of biological material taken from an infant is at least 5 ml. This allows, if a medical error is made, to re-conduct the study or send blood for additional analysis if the general analysis is insufficient for some reason.
Blood collection must be carried out under sterile conditions
Some parents are wary of the procedure of taking blood for analysis from a young child. There are no objective reasons for this. Laboratory assistants wear gloves; modern automatic scarifiers, designed specifically for small children, do not cause much discomfort and cause minimal pain. At the same time, the hematological analysis itself allows you to most accurately determine the general condition of the body, as well as correctly make a diagnosis if the presence of pathology is suspected. As you know, the earlier a disease is detected, the easier it will be to cure it.
Types of lancets and their features
Lancet needles are divided into two main categories; they are automatic and universal. Handles with automatic lancets independently determine the required level of puncture depth and collect blood. The needles in the device are replaceable and cannot be reused.
After the puncture, the lancets are placed in a special compartment. When the lancets run out, the patient replaces the drum with needles. For safety reasons, some piercing pens only work when the needle touches the skin.
Automatic lancets are individually marked and may differ from each other, depending on the patient’s age and skin type. These needles are very convenient to use, so they are in great demand among diabetics.
- Universal lancets are small needles that can be used with almost any lancing device that comes with your meter. If there are any exceptions, the manufacturer usually indicates this information on the packaging of consumables.
- Some models of lancet needles can be used to adjust the puncture depth. For safety reasons, universal lancets are supplied with a protective cap.
- Lancets for children are also sometimes classified as a separate category, but such needles are in low demand. Diabetics usually purchase universal lancets for such purposes, since their price is much lower than for children. Meanwhile, the children's needle is as sharp as possible so that the child does not feel pain during the puncture and the area on the skin does not hurt after the analysis.
To facilitate blood collection, lancet needles most often have the function of adjusting the level of puncture depth on the skin. Thus, the patient can independently choose how deeply to pierce the finger.
As a rule, a diabetic is provided with seven levels, which affect the degree and duration of pain, the depth of entry into the blood vessel, and the accuracy of the obtained indicators. In particular, the results of the analysis may be controversial if the puncture is shallow.
This is due to the fact that the skin contains tissue fluid, which can distort the data. Meanwhile, a minimal puncture is recommended for children or people with poor wound healing.