The appearance of blood in a child’s stool in most cases causes panic among parents, but, as a rule, in childhood such an abnormal process rarely threatens the baby with a fatal disease. There are quite a large number of different provocateurs, both quite harmless and very dangerous. Therefore, in order not to guess and not miss the chance for a speedy recovery, it is recommended to contact your pediatrician when asking why your child is pooping with blood.
In addition to blood, other impurities such as mucus or foam can be seen in the stool. Additionally, other symptoms may be observed that indicate problems with the baby’s health. When visiting a pediatrician, parents should inform the doctor about all manifestations known to them.
Causes of blood in stool
Blood impurities can turn stool black (if it is bleeding from the esophagus, stomach and duodenum). If there is not enough of it, it may look like blood streaks, strings or droplets on a diaper. Why does an infant have diarrhea with blood or do blood streaks appear in the stool?
The appearance of blood in the stool of a baby has the following reasons:
- Bleeding cracks in mother's nipples. A breastfed baby swallows maternal blood along with milk. For diagnosis, the occult blood test and the Apt-Downer test are used.
- Constant constipation, in which hard feces are formed. Defecation is difficult, the child needs to strain, and as a result, rectal cracks occur. In this case, the blood is not mixed with feces and has a bright color. If constipation occurred 3 months ago or more, it is called chronic.
- An allergic reaction in an infant (when fed with unadapted formulas and cow's milk, which contains foreign protein or when a food allergy occurs).
- Intestinal dysbiosis (often occurs after taking antibiotics). With dysbacteriosis, foamy, sometimes liquid stools streaked with blood are observed.
- Inflammatory diseases of the digestive tract (for example, colitis). Specks and traces of blood do not mix with feces. Mucus often appears in the stool.
- Hemorrhagic disease of newborns. Blood in the stool can be caused in an infant by a deficiency of vitamin K, which affects blood clotting.
- Juvenile intestinal polyps. They rarely form in a one-year-old child, most often appear after 5 years. The main sign is scarlet blood in the stool of a newborn without fever. To confirm the diagnosis, sigmoidoscopy or colonoscopy under anesthesia is performed.
- Intussusception. Often occurs in infants due to the fact that their intestines are relatively longer and more mobile than those of adults. At the site of invagination, an area of venous stasis is formed. As a result, some of the blood leaks into the intestinal lumen. On the baby’s diaper you can see discharge in the form of “raspberry jelly”.
- Acute intestinal infection (shigellosis, salmonellosis, rotavirus gastroenteritis). The temperature rises, vomiting, loss of appetite, and diarrhea occur. In this case, mucus with blood is formed in the baby's liquid stool. Also, green stools often appear.
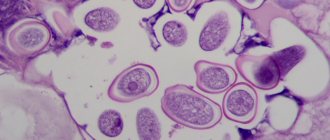
- Helminthic infestations. They often occur with trichuriasis, when helminths attach to the intestinal mucosa and then fall off, which is accompanied by bleeding from their points of attachment. In this case, the child has stool with mucus and blood.
- Lactase deficiency. It occurs when the content of the lactase enzyme is less than normal. In children, foamy diarrhea with streaks of blood and mucus in the stool is observed.
- During teething. The baby tooth erupts with a drop of blood, which can be found in the stool after swallowing.
- When introducing complementary foods before six months of age.
Associated symptoms
It is necessary to immediately show the child to a specialist if the following symptoms are present:
- heat,
- weight loss,
- vomit,
- diarrhea with blood in a baby,
- green chair,
- pale skin (a sign of anemia).
Among the harmless reasons for the appearance of dark stool in a baby are: taking iron supplements, feeding the mother with foods that can color the stool and introducing the first complementary foods. Red fabric strings from diapers can be mistaken for streaks of blood.
What should you do if there are large amounts of blood streaks in the baby’s stool, large clots of coagulated blood are observed, or, conversely, there is a little liquid scarlet blood on the diapers? We urgently need to take the baby to the pediatrician! Blood in dark, runny stool in an infant may indicate internal bleeding, and its scarlet color indicates problems in the lower digestive tract (for example, a bleeding polyp).
Hemorrhagic disease of the newborn
Occurs when there is a deficiency of vitamin K, which promotes the formation of blood clotting factors. It is observed in approximately 2 out of 100 children if vitamin K was not administered in the maternity hospital after birth. The classic form of the disease occurs when the child is breastfed. Symptoms occur between 3 and 5 days of life and include hematemesis, loose, bloody stools (melena), skin hemorrhages, cephalohematoma, and bleeding when the umbilical remnant falls off.
The cause of bloody diarrhea is the formation of small ulcers on the mucous membrane of the stomach and duodenum. The main mechanism of their occurrence is an excess of glucocorticoids (during stress during childbirth), hypoxic damage to the stomach and intestines. Also, blood in the stool and vomiting in an infant can be caused by peptic esophagitis (inflammation of the esophagus) and reflux of stomach contents into the esophagus.
Late hemorrhagic disease occurs before the 10th week of a child’s life. If bleeding occurs later (in a 3-month-old or 4-month-old child), then this disease can be excluded.
What should a newborn's stool look like?
After birth, babies produce their first waste product, meconium. It is a thick dark olive mass that resembles tar. This is the absolute norm. Meconium (or original feces) has no odor, as it is practically devoid of bacteria. It will be released for about 2 days. If meconium is excreted longer, doctors may suspect that the newborn is not receiving enough nutrition.
Approximately on the third day, the baby may begin to experience transient stool disorder or physiological dyspepsia. At the same time, the stool becomes more frequent, liquid, almost watery, mixed with greens, mucus and lumps. This phenomenon occurs due to the active colonization of the body by microbes and lasts 3-4 days. Physiological dyspepsia can be expressed by only one of these symptoms. There is no need to worry, this phenomenon goes away on its own and does not require any intervention. If transient stool disorder lasts more than 4 days, then this is a reason to consult a doctor.
Subsequently, the number of beneficial microorganisms stabilizes, the stool becomes yellowish with a sour odor. The acceptable norm is an admixture of mucus, green and white streaks in a small amount. If the child is bottle-fed, then it is necessary to ensure that the feces do not contain undigested pieces of food due to overfeeding.
Normally, a baby’s stool after transitional periods is from golden yellow to light brown in color, with a porridge-like consistency, with a slight sour-milk odor. If the child is bottle-fed or mixed-fed, the stool will be light brown with an admixture of greens, mucus, a thick mushy consistency and an unpleasant odor.
Diagnostics
Coprogram. The main research method that is carried out in all medical institutions. Allows you to determine whether there is mucus, an admixture of red blood cells and particles of undigested food in the feces of a baby, as well as many other indicators. Based on the results of the coprogram, the doctor can make a correct diagnosis.
Coagulogram. Blood from the digestive tract of a baby in the feces sometimes indicates the appearance of congenital disorders of the blood coagulation system. When performing a coagulogram, prothrombin and thrombin times and fibrinogen are determined.
The Apta-Downer test is used to differentiate bleeding in a child under one year old with the syndrome of swallowing maternal blood from cracked nipples. For this purpose, bloody vomit or feces of the baby are taken. They are diluted with water and a solution is obtained that contains hemoglobin. Hemoglobin in a newborn child differs in structure from that of an adult. The resulting mixture is centrifuged and mixed with sodium hydroxide solution. The appearance of a yellow-brown color indicates the presence of hemoglobin A (mother), and the persistence of pink color indicates the presence of hemoglobin of the newborn (alkali-resistant Hb F).
Gregersen test or fecal occult blood test. Used when bleeding from the digestive tract is suspected, when blood is not visually detected in the stool. Meat products are excluded before testing.
A possible range of results are classified according to the amount of hemoglobin in the stool: negative reaction (absence of occult blood in the stool), weakly positive (+), positive (++, +++), strongly positive reaction (++++).
The reaction to Gregersen's blood is widespread only in the CIS countries; in other countries, a stool test is used to determine human hemoglobin using an enzyme-linked immunosorbent assay.
Tests for lactase deficiency. What to do if you suspect this pathology? A quantitative determination of carbohydrates in feces, a breath test (hydrogen content in exhaled air after taking lactose), a D-xylose absorption test and others are carried out.
A stool test for dysbacteriosis, a stool test for helminth eggs, and general blood and urine tests are also performed.
Blood or bloody streaks in the baby's stool require additional diagnostic methods. The need for these examinations is determined after consultation with the following doctors: pediatrician, gastroenterologist, allergist and hematologist.
Laboratory test for occult blood
Blood in stool cannot always be seen with the naked eye. There are several reasons for the penetration of blood into the organs of the digestive tract, but due to its small amount and transformation into iron sulfate after leaving the body, its presence can only be detected with the help of a special laboratory test.
If a test has been prescribed to detect hidden blood in the stool of an infant, parents should not refuse such an examination, even if the test is recommended as a preventive measure and not because of illness.
The presence of hidden blood in stool can be caused by the following reasons:
- liver diseases;
- intestinal tuberculosis;
- the presence of a duodenal or stomach ulcer;
- tumors in the esophagus at the stage of decay;
- stomach cancer.
The above pathologies are most often characteristic of older people, and not children in the first year of life, but the possibility of the presence of one of these diseases cannot be excluded either.
When collecting an occult blood test, parents must adhere to all medical recommendations, since this test is sensitive to even the smallest particles of blood. For example, if a child has a trauma to the oral mucosa or teething, the test for occult blood will be positive.
Treatment
General therapeutic principles for the treatment of diseases that lead to the appearance of blood in the infant’s stool:
- If a formula-fed or bottle-fed baby suffers from constipation, it is necessary to replace the formula or use laxatives in the form of syrup.
- Intestinal obstruction is treated with surgery using manual spreading of the intussusception.
- Acute intestinal infection has two lines of therapy: rehydration and antibacterial.
- If you are allergic to cow's milk protein, such feeding must be replaced with a highly adapted mixture.
- Lactase deficiency is treated with the use of lactose-free mixtures (Nutrilon Lactose-Free, Enfamil Lactofri).
- Hemorrhagic disease of the blood coagulation system in infants is treated with the administration of a synthetic analogue of vitamin K (vicasol).
Blood in the stool of an infant should not cause panic among parents. It is best to consult a pediatrician. If inclusions or blood streaks in the stool recur for a long time, the child does not gain weight or loses appetite, it is necessary to go to the hospital for a wide range of diagnostic or therapeutic procedures.
(
1 ratings, average: 5.00 out of 5)