An analysis for dysbiosis allows you to determine whether beneficial and pathogenic bacteria are present in the intestines and to estimate their quantity. Mostly, such a study is indicated for children in the presence of symptoms characteristic of dysbiosis in the form of constipation or diarrhea, abdominal pain, and flatulence. The analysis results may contain various microflora, including clostridia, which have a negative effect on the child’s body.
Why are clostridia dangerous?
They belong to opportunistic microflora, forming one group with staphylococcus, enterococcus and candida. Such microorganisms, when favorable conditions arise, can turn into pathogenic bacteria, causing quite serious disruptions in the functioning of the body. Therefore, if there are suspicions, it is important to do a timely analysis of the intestinal microflora and carry out the correct treatment as quickly as possible, improving the child’s condition.
Clostridia take part in protein processing. During their life processes, by-products are formed in the form of skatole and indole - toxic substances that do not have a negative effect if present in moderate quantities. Normally, skatole and indole activate intestinal motility, promoting better evacuation of feces. If intestinal dysbiosis is diagnosed, there is an increased number of clostridia and an increase in the level of these substances, which can become a trigger for putrefactive dyspepsia - a serious disruption of the functioning of the digestive system.
In addition, clostridia in the presence of dysbiosis provoke the development of the following pathologies:
- Tetanus.
- Botulism.
- Gas gangrene.
- Pseudomembranous colitis.
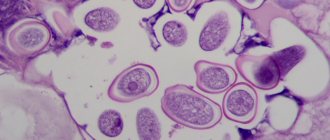
The most common are clostridia of the Difficile type, whose natural habitat is soil. The peculiarity of this species is the ability to form endospores and enclose them in a shell, allowing them to survive an “unfavorable” period. As a result, when released into the external environment, they can live for at least two months even at fairly high temperatures (for example, when boiling). If the problem is associated with an increase in the number of such microorganisms, doctors immediately note the complex treatment of dysbiosis, which is due to the low sensitivity of the Difficile species to antibiotic therapy.
Normally, this type of opportunistic microflora is present in the microbial composition of the gastrointestinal tract, namely in the area of the large intestine. A newborn child is especially susceptible to the negative influence of this type of clostridia and the dysbiosis provoked by them due to the immaturity of the digestive system. As a result of their activity in the gastrointestinal tract, Difficile microorganisms secrete toxins A, B and protein that inhibits peristalsis, inhibiting the digestion of food, triggering fermentation and putrefactive processes, which are a source of inflammation.
Stool analysis can also reveal dysbacteriosis associated with the activity of another species - Perfringens, which is the cause of the development of food toxic infections and necrotic enteritis in children - a disease accompanied by acute abdominal pain, bloody diarrhea, vomiting and peritonitis, the formation of ulcers in the small intestine due to exfoliation mucous membrane and gas stratification of the submucosal layer of the intestine. When a stool test for dysbacteriosis contains a large number of clostridia of this type, it is necessary to immediately limit the intake of protein into the body and decide on drug therapy.
Basic indicators
The normal color of stool is light or dark brown. Changes in color may indicate problems in the body.
- When breastfeeding, the color of stool is greenish. Yellow stool means that the baby is getting enough mature milk.
- Taking certain medications (antibiotics, activated carbon) changes the color of stool. Black inclusions, strings, dots, and sand appear in it.
- Foods affect stool color.
- Reaction to bilirubin. In this case, the stool is yellow or orange. Bilirubin is often detected in the first months. Bilirubin in feces can increase with dysbacteriosis. When bilirubin is elevated, the child looks lethargic, eats poorly, and has yellowing of the skin and whites of the eyes. The intestinal flora is disrupted.
- White stool may indicate an infectious liver disease - hepatitis.
Black specks and sand are often the remains of overcooked food. Black threads appear from eating bananas, black dots - from kiwi, raspberry, and currant seeds. In children who were offered an apple or pear for the first time, black dots, sand and strings can be found in their stool.
If white lumps like sand, as well as mucus and blood appear in the stool, this indicates a bacterial infection. White spots may be the cause of dysbacteriosis. White sand-like grains do not indicate pathology. Parents should be alerted to white streaks that indicate candidiasis.
Watery stools, fever, bright yellow or green color of stool, and its pungent odor should not be ignored.
With constipation, there is no stool for more than two days. The consistency of stool becomes hard and dry. The reasons for the absence of stool for a long time may be the mother’s poor diet, lack of fluid, or taking medications.
The mother should be alarmed by the absence of feces for more than three days. In this case, it is necessary to resort to emergency measures.
White lumps may appear as a result of curdled milk. Perhaps the child is overfed and does not have time to produce enzymes. White lumps like sand require treatment when the child appears lethargic and has a fever.
Streaks of blood may appear as a result of an allergic reaction to cow's milk protein.
The smell of feces in formula-fed children resembles rot, while in breastfed children the smell is sour. Changes in odor indicate diseases of the internal organs.
A foul odor occurs in diseases of the large intestine and pancreas. A putrid odor is observed in colitis and putrefactive dyspepsia. A sour smell is characteristic of fermentative dyspepsia.
If significant impurities appear in the child’s stool, vomiting, fever, loss of appetite and weight, you should immediately consult a doctor.
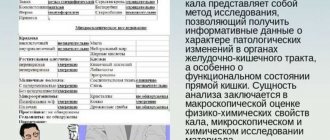
Coprogram: norm and deviations
In some cases, pathological changes in the child’s internal organs may occur.
Blood (erythrocytes) in a child’s stool is detected in the following cases: rectal fissures, atopic dermatitis, intestinal inflammation, changes in the functioning of the digestive organs, polyps.
A reaction to occult blood (red blood cells) in a coprogram indicates bleeding, ulcers, hemorrhoids, polyps or a tumor.
Reaction to clostridia
Clostridia is a complex of bacteria. Clostridia provokes such serious diseases as tetanus, botulism, necrotic enteritis.
Clostridia perform the function of breaking down protein and improving intestinal contractions. An increase in their number leads to serious consequences.
A positive reaction to clostridia can occur when an infection enters a child’s body through dirty dishes, toys, or clothes. Clostridia can be suspected if foam and mucus are found in the stool. Clostridia are detected by bacteriological examination of stool.
If clostridia is detected in a child, treatment will be aimed at restoring the intestinal microflora. Prebiotics, enzymes, and enterosorbents are prescribed.
Detritus
Detritus can indicate good functioning of the digestive organs. In the case when detritus increases, mucus and leukocytes appear, we can talk about colitis or dysbacteriosis.
Detritus is small particles of digested food. In a coprogram it is about (up to 5 characters). Detritus marked with one sign indicates constipation.
Detritus in combination with other signs indicates diseases of the digestive system. If fatty detritus is detected, then it is necessary to examine the liver and pancreas. Loose stools and reduced detritus indicate the occurrence of disorders in the small intestine. Detritus against the background of bacteria and epithelium increase during the inflammatory process in the body.
Reaction to stercobilin
Stercobilin is a bile pigment resulting from the transformations that bilirubin undergoes. Stercobilin appears in the feces of a child aged 5-6 months.
In children under 5 months of age, stool shows a positive reaction only to bilirubin. This is why the stool is green or yellow. From 5 to 8 months, stercobilin and bilirubin are detected in the stool. In the feces of children from 8 to 9 months there is only stercobilin, there is no bilirubin.
Stercobilin decreases with jaundice caused by stones, tumors or cysts, inflammation of the bile ducts, and hepatitis. Stercobilin is completely absent when the biliary tract is blocked. The stool becomes colorless and clayey.
If bilirubin and stercobilin are detected in the stool analysis of a child over 9 months old, this indicates hidden dysbacteriosis.
Stercobilin increases with hemolytic anemia, when red blood cells are destroyed (for various reasons), or with increased outflow of bile.
Neutral fat and fatty acids
When the stool contains fatty components, they speak of a disease such as steatorrhea. The feces leave a greasy mark on the surface.
Fat in stool can appear due to diseases of the pancreas or liver. Perhaps the fat is not completely absorbed and is excreted along with feces.
Fat, soaps, or fatty acids may be found in the stool. There are cases when all three components are detected simultaneously. The color of the stool may not change, the smell becomes pungent. Fat in feces is combined with colic, lethargy, dry cough, and diarrhea.
To reduce fat in stool, treatment should be based on taking drugs with a high lipase content.
Ideally, neutral fat is absent from feces. It must be completely absorbed by the body, as it is a source of cell growth and development. In infants, small amounts of neutral fat may be found in the feces.
Neutral fat is found in pancreatitis, liver and biliary tract diseases.
Fatty acids should also be normally absent. Their appearance is associated with disruption of the digestive system.
Iodophilic flora is a complex of different types of bacteria (cocci, rods). When they come into contact with iodine, they turn black. Normally, iodophilic flora is detected in small quantities or completely absent.
Iodophilic flora increases with dysbacteriosis or inflammatory processes of the digestive organs, gastritis.
Iodophilic flora is not always a sign of disease. The indicator is always evaluated based on other parameters.
If a child is breastfed, then most often iodophilic flora occurs due to dysbacteriosis. Probiotics and bacteriophages are prescribed. If the child is bottle-fed, then you need to choose the right formula.
In cases where iodophilic flora is detected in more serious diseases (pancreatitis, gastritis), the doctor may prescribe additional examination methods.
Enterococci
Enterococci are microorganisms that populate the intestinal flora. They are responsible for immunity. Enterococci begin to multiply rapidly when you have a cold or take antibiotics. The main symptoms of enterococci in a child’s stool are diarrhea, change in stool color (green), and refusal to eat.
Enterococci can cause dysbacteriosis, infection of the genitourinary system, and inflammation of the abdominal cavity. Enterococci should be treated with bacteriophages, which normalize the microflora.
Enterococci increase with decreased immunity. Therefore, the mother should harden the baby. If enterococci are below normal, this is considered a physiological norm.
Dangerous types of clostridia and symptoms of the disease
A danger to the child’s health (that is, a possible confirmation of the diagnosis of an infectious disease) is:
- detection of a large number of clostridia in combination with other changes in the microbial composition of feces;
- detection of Cl. botulinum (in a child under 1 year of age);
- detection of Cl.difficile or Cl.perfringeus.
The detection of such pathogenic clostridia as Cl.tetani in feces does not pose any danger to the health and life of the child. The clinical picture of the disease is directly determined by the action of a specific exotoxin. In the human body (including the intestines), Cl.tetani does not have the ability to produce toxin. Therefore, the detection of only the causative agent of tetanus is just an incidental finding.
Diseases caused by various clostridia are treated by an infectious disease specialist, gastroenterologist or family practice doctor. Prevention of all variants of clostridiosis consists of careful compliance with all sanitary and hygienic standards regarding food products offered to the child.
Dysbacteriosis and clostridia
We can talk about dysbiosis of the digestive tract in the case of pronounced changes in the ratio of the microbial composition of the intestine in a child of any age. These include:
- reduction in the content of lacto- and bifidobacteria;
- an increase in the content of clostridia (any saprophytic), certain types of Escherichia coli;
- the appearance of microbial agents (staphylococcus, proteus, streptococcus), which are not representatives of the normal intestinal microflora.
Dysbacteriosis can be either an independent disease or a complication of many infectious processes (shigellosis, salmonellosis), or its development is the result of long-term drug therapy (especially broad-spectrum antibiotics).
The reasons for the formation of dysbiosis are not fully understood, since in different people the action of the same damaging factors (listed above) can cause different changes in the intestines.
Clinical signs of dysbiosis are quite nonspecific and are the same in a child of any age. The most significant include:
- decreased or complete lack of appetite;
- repeated nausea and vomiting;
- bloating and flatulence;
- A very young child experiences unmotivated restlessness, constant crying, and lack of weight gain.
The diagnosis of dysbiosis can only be made based on the results of a specific laboratory test - the so-called stool test for dysbacteriosis. In some cases, an instrumental examination of the intestine will be required: sigmoidoscopy or irrigoscopy.
Treatment of dysbacteriosis is very complex and lengthy, requiring the attention of the parents of a small patient in terms of fulfilling all medical prescriptions. You should absolutely not use the first remedy you come across in a pharmacy or flashed in a television advertisement, since uncontrolled intake of pre- and probiotics can only worsen existing changes in the microbial composition of the intestines.
Botulism
This is one of the most severe infectious diseases of a toxic nature, which without appropriate treatment can be fatal.
The pathogen Cl. botulinum comes from various food products - home-made canned food, sausage and fish (also home-made), honey.
An important point is that only in the body of an infant Cl. botulinum is capable of producing exotoxin, which is the main factor causing clinical symptoms of the disease. Therefore, the detection of Cl. botulinum in the feces of such a baby confirms the diagnosis. An increased risk of developing this form of botulism is observed in young patients who are breastfed (artificial formulas often include honey).
What is clostridia?
Clostridia is a gram-positive bacterium with a spindle-shaped form. This bacterium can be found in the intestines of a child or an adult for natural reasons, participating in the digestion process, or it can cause various diseases depending on the type of bacterium. More than 100 species of clostridia have been discovered and well studied in the world, but only a few of them will provoke the development of pathology in children.
The danger of clostridia lies not in their presence in the human body, but in their ability to secrete a toxin that affects the functioning of the digestive tract and nervous system.
Clostridia are fairly stable bacteria that can live for a long time in soil, food, water, etc., due to being in a spore state. When exposed to favorable conditions (human intestines), clostridia enter the stage of growth and reproduction and begin to depress the state of the body.
Clostridia infection can occur:
- Through the soil (children pull sand and dirt into their mouths).
- By consuming poorly processed fruits and vegetables grown on contaminated soil.
- Contact and household contact through dirty hands, kitchen utensils, toys).
- When consuming foods with a long shelf life (canned food).
If these bacteria enter the body in small quantities, then the immunity of adults and newborns is able to overcome them, but children after a year may not be able to cope with the disease.
In an adult, immunity has already been formed, in a baby it is supported by mother’s milk, but children who eat normal food are in limbo, since the immune defense is trying to form on its own and the body is not yet fully strengthened. But even a strong immune system will not save you if clostridia enter the human intestines in large quantities and begin to lead active life activities. In such a situation, only drug therapy can help the child.
Prevention
Preventive measures largely consist of maintaining hygiene and sanitary standards for storing and processing products. To avoid infection:
- sick children or adults are isolated;
- promptly treat intestinal dysbiosis;
- properly organize feeding and care of the baby;
- products that are eaten raw are thoroughly washed, the rest must undergo sufficient heat treatment;
- carefully monitor the shelf life of products;
- Sanitation stations are actively identifying carriers of clostridia among specialists in child care institutions and food industry workers.
Long courses of broad-spectrum antibiotics do not work as a treatment, much less as a prophylactic agent. A specialist should prescribe the medicine after identifying the pathogen. The course of antibacterial therapy lasts on average 5-7 days.
To avoid excessive proliferation of bacteria, it is necessary to treat dysbacteriosis in a timely manner, as well as to prevent this condition.
Normal or pathological?
Caring parents quickly become frightened when a child is tested for dysbacteriosis with clostridia, but it is too early to panic. These bacteria are normally found in the intestines and their detection in a child’s stool is quite justified if the amount does not exceed the established limits:
| Age category | Norm (COE/g) |
| Up to 1 year | 10(3) − 10(4) degrees |
| From one year to 18 years | 10(5) - degrees |
| Over 18 years old | 10(6) - degrees |
If the stool analysis shows values higher than those indicated, then you should worry. Another reason to start a comprehensive diagnosis is the presence of clostridia in the feces in the permitted quantity and the presence of accompanying bacteria that are not characteristic of a healthy body. But only a doctor should always make a conclusion based on the patient’s complaints, the clinical picture and the conclusions of diagnostic doctors.
Video
Clostridia in normal stool analysis
Most clostridia found in the stool of a child of any age are not dangerous (pathogenic) for the body. It is these microbial agents, due to their proteolytic properties, that carry out the processes of digestion of protein substances in the distal parts of the digestive tract. Depending on age, the following amounts of clostridia are found in stool:
- in infants and children under 1 year of age - within 103-104 CFU;
- in children of nursery, school and adolescence – 105 CFU;
- in adults over 60 years of age – 106 CFU.
However, an increase in the number of clostridia in stool does not mean an infectious disease. An infectious disease should be considered in the event of a serious imbalance of intestinal microflora (dysbacteriosis) or the appearance of pathogenic species of clostridia.
General symptoms of clostridiosis
Clostridia is an insidious and dangerous disease that affects several systems of the human body. The children's immune system is practically unable to resist these bacteria, and the disease manifests itself with pronounced symptoms. The main thing is to pay attention to the symptoms of the disease in time, since delay in treatment can cost the child’s life (clostridia are so dangerous).
The main symptoms of clostridiosis include:
- Rapid onset of disease development.
- A sharp rise in temperature above 39˚C.
- Manifestation of dyspeptic symptoms (nausea, vomiting, diarrhea).
- Damage to the central nervous system, expressed by disorders of vision, speech, and swallowing.
- Pain in the peritoneum (cramping sensations), with palpation of the intestines the pain intensifies.
- Sudden weight loss and other signs of dehydration.
- Mental disorders may occur if left untreated for a long time.
Depending on the type of clostridia causing the disease in the child, the clinical symptoms will vary slightly, especially in the severity of the disease.
Causes of clostridiosis
Let's consider the main routes of transmission of infections associated with clostridium spp. The carrier can be not only a person, but also an animal. Once the bacteria get into the soil or bodies of water with feces, they can live there for several months. The process of transmission of bacilli depends on the type of clostridia and the symptoms of the disease. The main routes of infection are food and household contact. If we consider the transmission of infection through food, the greatest risk of infection is associated with the consumption of insufficiently thermally processed meat, dairy products, fruits, and vegetables.
Types of clostridioses
There are several pathogenic groups of clostridia that can cause illness in children and can be detected in stool during examination. This:
- Botulinum – causes botulism when it enters the child’s intestines from the outside along with food. But in children under one year of age, this type of clostridia can begin to independently produce exotoxin and infect the body. In older children, Cl. Botulinum does not cause problems if it is present in the stool but does not enter the intestines from the outside.
- tetani - causes tetanus, but only if it enters the human blood through a wound surface. The detection of these clostridia in feces is not a cause for concern, since the bacteria are not capable of producing a toxin in the intestines and cannot cause disease.
- perfringeus – causes gastroenterocolitis in children when ingested through food. Clostridium Perfringens poses the greatest danger when it enters a weakened child’s body.
- difficile – causes pseudomembranous colitis in children while taking antibacterial agents. The main reason for the development is intestinal dysbiosis, since normal microflora is absent and previously existing clostridia of this group begin to operate.
Botulism
A child can become infected with botulism by consuming canned foods, meat and fish – home-made or store-bought. The disease is quite dangerous and in 30% of cases leads to death. Symptoms of botulism:
- Double or foggy vision.
- Inability to swallow.
- Difficulty pronouncing words.
- Difficulty breathing.
These symptoms appear in a ladder one after another and correspond to a certain stage of development of the disease. At the last stage it is no longer possible to save the child, but at the penultimate stage it is very difficult.
Gastroenterocolitis
Gastroenterocolitis caused by clostridia occurs in a child in almost the same way as with other causes of the disease. Its symptoms are:
- At first there is a feeling of nausea.
- Vomiting is repeated several times.
- Diffuse pain covers the entire area of the abdomen.
- Impurities of blood, mucus and even pus are found in liquid stool.
With this type of gastroenterocolitis, only antibacterial drugs in combination with medications to maintain the balance of intestinal microflora can help. Treatment must be started immediately, otherwise the child may suffer from rapidly developing dehydration.
Pseudomembranous colitis
The disease develops against the background of intestinal dysbiosis after a long course of treatment with antibiotics.
The child’s weak body is unable to fight the existing clostridia of this genus, which are necessary to maintain the digestion process, and their number in the feces begins to exceed the permitted limit. The symptoms of the disease are standard for ordinary colitis (abdominal pain, dyspepsia, dehydration), and a correct diagnosis can only be made through laboratory tests of stool, as well as taking an anamnesis to understand that the disease developed after taking antibiotics.
What it is
Clostridia are opportunistic microorganisms, just like candida, enterococci and staphylococci. They are shaped like a spindle, hence the corresponding Latin word.
These gram-positive bacteria produce a special enzyme that helps digest protein, converting it into amino acids. But in addition, spindle-shaped rods are capable of producing various toxic substances.
An increased amount is evidence of opportunistic microflora, when the poison of numerous bacteria can poison the body. If conditions favorable for clostridia are created in the intestines, the rods begin to actively multiply and become pathogenic, disrupting the functioning of the circulatory, nervous and digestive systems.
Infection with clostridia leads to acute pathological conditions called clostridiosis.
Pathological processes occur due to two factors:
- bacteria produce strong toxins, which, when released into the blood, depress the nervous system and blood cells, and reduce the vital activity of body cells;
- in addition to toxins, a colony of microorganisms secretes a special group of enzymes, which leads to local tissue damage.
What happens during clostridiosis
Clostridia rods can live in the ground for a long time. They also live in the intestines of animals and humans, and are excreted with feces. Bacterial spores enter the child's body along with contaminated food.
They then multiply in the small intestine, provoking an inflammatory process. Through the intestinal epithelium, clostridia are absorbed into the blood and nearby tissues, producing toxins during their life processes and leading to symptoms such as toxicosis and diarrhea.
Diagnostic measures
In a regular coprogram it will not be possible to see clostridia, so there is no need to test feces for everything.
It is necessary to take a sensible approach to the choice of diagnostic procedures in order to establish not only the presence of clostridia and their quantity, but also to determine the species.
This will help:
- Sowing stool on a nutrient medium.
- Analysis of stool for dysbacteriosis.
- Endoscopic examination of the intestines if necessary.
- Computed tomography as an auxiliary diagnostic method.
Also, contacting a specialist implies the mandatory collection of anamnesis and a visual examination of the child (mucous membranes, skin, etc.), palpation of the abdomen. After receiving the test results, the gastroenterologist (or pediatrician) will be able to prescribe appropriate therapy for the child.
How to treat clostridiosis?
If clostridia detected in a child’s stool is the cause of his poor health, then treatment must be done immediately. Treatment for each type of clostridiosis will be specific and may include taking the following groups of drugs:
- Antibacterial agents to which the detected species of clostridia are sensitive (Metronidazole, Vancomycin).
- Probiotics and prebiotics to restore intestinal microflora (Linex, Bifidumbacterin, Lactofiltrum, Hilak-Forte).
- Enterosorbents as symptomatic treatment (Smecta, Activated carbon, Enterosgel).
- Administration of solutions to eliminate symptoms of dehydration (saline, glucose).
- Vitamin preparations, especially group B.
- Enzyme preparations (Mezim, Creon, Omez).
It is necessary to treat clostrizia in a timely manner, since children are highly susceptible to the influence of toxins released by these bacteria and have a hard time suffering from such diseases.
If clostridia is detected in a child’s stool, you should consult a doctor to understand whether the threat is real. If yes, then you should start treatment after consultation and diagnosis, and if not, then you just need to continue to observe the rules of personal hygiene to avoid infection with pathogenic types of clostridia.
www.lechimzapor.com
Treatment and prevention
The reason for treatment is not the clostridia in the analysis, but the immediate symptoms of a specific clostridiosis. Severe diseases such as botulism, tetanus, gangrene, as well as the most severe forms of diarrhea and colitis require immediate hospitalization to save the patient’s life.
During outpatient treatment, antibiotics that act on bacteria and a special diet are prescribed. Prevention comes down to careful adherence to the rules of personal hygiene, good heat treatment of potentially dangerous products, as well as vaccination against tetanus.
How dangerous is the pathogen?
Clostridia develops seasonally, mainly in the summer-autumn period. Since the main method of transmission is through household contact, children are most susceptible to infection. This is due to the fact that children try to taste everything.
Clostridiosis manifests itself in the form of acute gastroenteritis, accompanied by vomiting, diarrhea, and cramping abdominal pain. In parallel, the toxin causes necrotic changes in the intestinal wall, with the development of necrotizing ulcerative colitis. The main complications that a child may have:
- Acute dehydration. It is the result of developed gastroenteritis, accompanied by uncontrollable vomiting and diarrhea. At the same time, the child loses a lot of fluid, and since the child’s body consists of moisture in percentage terms to a greater extent than an adult, dehydration develops quickly. Blood pressure drops, the pulse becomes thread-like and superficial. The child loses consciousness. Intensive therapy is required in the form of volumetric infusions to correct the water balance, otherwise the condition can be fatal.
- Sepsis. Intestinal inflammation leads to increased permeability of the vascular wall and penetration of the infectious agent into the bloodstream. This allows the bacteria to spread throughout the child's body. Due to the massive release of toxin into the blood, a bacterial-toxic shock develops, which cannot be stopped even in an intensive care unit. The death of a child can develop instantly.
- Fecal peritonitis. It is a consequence of erosive ulcerative colitis, as a result of which the bacterium attacks the intestinal mucosa, corroding it. As a result, the wall becomes thinner and it may rupture with the release of intestinal contents into the abdominal cavity with the development of fecal peritonitis.
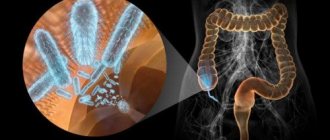
What affects the composition of the intestinal microflora?
The intestinal microflora of a child consists of beneficial (bifidobacteria and lactobacilli), neutral (enterococci) and conditionally pathogenic bacteria (clostridium, fungi, staphylococcus, proteus and klebsiella).
In a healthy intestine, these microorganisms coexist in certain proportions. The quantitative balance should contain 97% beneficial microorganisms and no more than 3% opportunistic microorganisms.
This ratio is supported both by the composition of healthy foods and by external factors.
When the number of obligate (beneficial) bacteria decreases, and the number of pathogenic ones, on the contrary, begins to grow rapidly, this condition in the intestines is usually called dysbiosis. What causes it:
- artificial or mixed feeding (the child stops receiving the necessary lactose and lysozyme);
- amount of food taken;
- congenital pathologies of the large intestine;
- systematic constipation;
- gastroduodenitis;
- inflammatory bowel infections;
- malfunctions of the pancreas, liver or gallbladder;
- stressful situations for the child.
But regarding the objectivity of dysbiosis as a diagnosis, the debate does not stop. Many pediatricians suggest that both the diagnosis itself and the problem are far-fetched. There are versions that treating dysbiosis is a completely pointless exercise, because any change in the bacterial composition will be leveled out by the child’s body on its own. Especially when we are talking about a child under 3 months of age, and at this stage the microflora is actively forming. And only when test results show a significant increase in Proteus bacilli, Klebsiella and Staphylococcus aureus, can corrective drug therapy be intervened.
Attention. In babies born by cesarean section, the formation of microflora occurs more slowly and longer due to the lack of contact with the mucous membrane of the mother's birth canal. At the same time, there is a high probability of colonization of the intestines primarily by pathogenic microorganisms.
Pathways of transmission and growth of bacteria
The microorganism is an anaerobic, that is, it is able to exist and actively reproduce in an oxygen-free environment. These thickenings contain endospores, which are difficult to reach with antibacterial therapy.
Microorganisms are transmitted by spores through the fecal-oral route. Thanks to spore formation, they are resistant to antibiotics and any disinfectants. A child becomes infected when a spore enters the gastrointestinal tract through the mouth. Young children are most often affected. Infection occurs through dirty hands, contaminated household items (cutlery, dirty clothes, a pacifier that has fallen to the ground), while playing in the sandbox with animals, toys in kindergarten. Infection can also occur with food. The pathogen can be found in products with low oxygen content: canned food, pickles, smoked meats.
Factors contributing to the development of dysbiosis and activation of clostridia reproduction in children are:
- long-term antibacterial therapy;
- decreased immunity due to somatic and infectious pathologies;
- prematurity;
- insufficient intake of nutrients into the body (violation of the diet if the child spends little time in the fresh air);
- stressful situations;
- environmentally unfavorable situation.
Thanks to the enzymes that the microorganism secretes, when it enters the small and large intestines, the mucous membrane is corroded and cellular structures are damaged. Erosive surfaces and ulcerations form. The microorganism begins to multiply, and the resulting spores enter the outside world with feces.
General characteristics of the genus
Clostridia are anaerobic rod-shaped (with the exception of the species C. coccoides) gram-positive microorganisms. These spore-forming anaerobes are capable of producing various enzymes, depending on the specific species. In spores, clostridia can easily survive high temperatures and most antibacterial drugs. Some of these bacteria, for example, clostridium difficile, are saprophytes; they are present in the healthy microflora of various systems of the human body, including the gastrointestinal tract. They live mainly in various intestinal sections.
Most common types
In nature, especially in soil, many varieties of these bacteria live everywhere. There are about 30 of them in the human intestinal flora. Some microbes are completely harmless to health, while others can cause fatal diseases. Let us give as an example the most famous types of clostridia:
- Clostridium botulinum – capable of producing botulinum toxin and causing the development of botulism.
- Clostridium tetani is the causative agent of such a severe neuroinfection as tetanus.
- Clostridium perfringens is a sulfite-reducing clostridia that affects the meat of domestic animals and poultry, and can reproduce in legumes. Consumption of such products causes toxic food infection. Costridium perfringens, as well as clostridium novyi, clostridium septicum, clostridium sordellii and a species such as clostridium oedematiens, can cause anaerobic wound infection (gas gangrene).
- Clostridium difficile, although it belongs to the normal intestinal microflora, under certain circumstances acts as a causative agent of diarrhea, and can also cause plaque colitis.
- Clostridium ramosum is a fairly common species in nature; the proliferation of these bacteria in the intestines is considered one of the factors of obesity.
- Clostridium tyrobutyricum is cultivated for industrial purposes for the synthesis of butyric acid (C3H7COOH), which is used in the production of plastics, varnishes, pharmaceuticals, etc.
- Clostridium histolyticum and clostridium sporogenes belong to the group of proteolytic bacteria; they are capable of fermenting proteins into amino acids. Clostridium histolyticum produces 5 types of toxins, some of which have strong necrotic properties.
- Clostridium pasteurianum is a free-living, non-pathogenic microorganism that reproduces by fermenting sugars.
Norms for content in feces
When stool is cultured for dysbiosis, clostridia are detected in 100% of cases. Their normal content in the feces of a child over 1 year old is up to 105 CFU/g. An indicator of up to 106 is a sign of dysbiosis, in the presence of clinical manifestations and carrier status when the child is in normal health.
Exceeding 106 indicates clostridiosis and requires consultation and treatment with an infectious disease specialist. In this case, a bacterial culture of stool is required with a test for sensitivity to antimicrobial therapy.
Symptoms
- pain in the abdomen, in the early stages in the epigastric region, then along the intestines;
- nausea;
- profuse vomiting;
- flatulence;
- fever accompanied by chills: the child often has vasospasm, characterized by coldness of the extremities against the background of hectic fever (temperature above 39-40˚C);
- loose stools with bloody foam and putrefactive odor;
- manifestations of dehydration: facial features become sharper, the skin loses its elasticity, the tongue is thickly covered with a white coating, the amount of urine decreases, the pulse quickens and blood pressure decreases;
- intoxication in the form of weakness, lethargy, drowsiness, apathy.
In childhood, most often, clostridiosis occurs as necrotic-ulcerative enteritis; due to the fact that the body is weaker than in an adult, signs of dysbiosis appear more often. Antibiotic-associated clostridiosis does not develop in breastfed children in the first year of life, since the baby receives the antibodies and protective factors it needs through mother’s milk.
Treatment
Treatment begins when signs of intestinal infection appear. In case of dysbiosis with a slight increase in the clostridia index, volume therapy is not required; correction of the microflora with the help of pro- and prebiotics is sufficient. Therapy for clostridiosis includes the following measures:
- Diet. The child is on a water-tea break, which helps replenish the water balance and relieves the intestines. Over the course of a day or two, the mother feeds the baby a tablespoon every 10 minutes. This allows you to restore fluid levels in the child's body.
- Infusion therapy. Necessary in severe cases. Used as detoxification and correction of dehydration. Large volumes of liquid are administered, preferably saline solutions (Ringer's, disol, acesol), glucose, Reosorbilact.
- Antibacterial therapy. It is carried out in accordance with the results of culture for sensitivity. Macrolides, protected penicillins or 3-4 generation cephalosporins are preferred as a starting drug.
- Microflora correction. They use pro- and prebiotics (Acipol, Bifiform, Enterol and others);
- Sorbents. They allow you to reduce the intoxication of the body by removing toxins naturally, and also help to consolidate the stool (Smecta, Atoxil, Activated carbon and so on);
- Hemostatics. If there is blood in the stool or bloody foam. Vikasol, Dicynon, Etamzilat are used.
- Glucocorticosteroids. They are used in severe cases to lower blood pressure and prevent shock.
- Antipyretic. As a symptomatic treatment for fever.
Therapy is complicated by the fact that virtually no antibiotic has any effect on the spores. They can remain in an inactive state for a long time and resume growth under favorable conditions – signs of dysbiosis.
In case of long-term clinical course of the disease, bacteriophages can be effective. The duration of therapy depends on the results of bacteriological culture. Sometimes it is enough to achieve clinical remission, but the child is not allowed into the children's group until the microflora is normalized in the laboratory.
Diagnosis and treatment
If suspicious symptoms appear, you need to have your child's stool tested. The conclusion indicates the specific type of pathogen and the toxin it produces. If the clinical picture is pronounced or there is a risk of dehydration, then the child is hospitalized in a hospital, since this is a life-threatening condition and he must be under constant medical supervision. Treatment includes the following:
- salt drinking solutions - to prevent dehydration and replenish the volume of useful electrolytes; indicated for profuse vomiting and diarrhea;
- probiotics – to restore normal intestinal microflora; prescribed when the activation of clostridia was provoked by antibiotic therapy;
- antibiotics and metronidazole - prescribed if a pathogenic bacterium enters the body with food;
- auxiliary agents that normalize the functioning of the gastrointestinal tract: enzyme preparations, choleretic drugs.
With timely treatment, it is possible to quickly reduce the concentration of pathogens. The child will begin to rapidly proliferate and repair tissue, and the symptoms of the disease will disappear. Regardless of the treatment regimen, it is always supplemented by a special diet. All harmful foods, sausages, sour fruits, and foods with laxative properties are excluded. Enveloping and strengthening foods will be useful: rice, bananas, potatoes. Lactic acid bacteria from kefir and natural yogurt will help quickly restore the balance of microflora.
Clostridia in a child's stool is not dangerous if an increase in their level was detected in time and adequate measures were taken. Antibacterial drugs and replenishing fluid in the body will help prevent dangerous consequences and quickly return the baby to good health. If not treated in a timely manner, severe dehydration and intoxication with substances produced by clostridia are possible; such conditions pose a serious danger.
Normally, the human intestine is home to many bacteria. The body of a newborn is populated by microorganisms in the first weeks of life through contact with the outside world. The community of such bacteria constitutes a unique intestinal microflora, and disturbances of bacterial balance in the intestine are called dysbiosis.
Clostridia bacteria are one of these intestinal inhabitants. They do not cause any harm as long as their quantity is within certain limits. But what will happen to children's health if these spore-bearing microorganisms begin to multiply excessively?
Is it necessary to do something if clostridia in a baby’s stool is elevated, and how dangerous is it for the baby’s health?
Forecast
The prognosis of the pathology depends on the severity of the disease. With a mild degree, minor clinical manifestations and a low degree of insemination of the pathogen in the feces, the symptom is favorable.
In more severe cases, the prognosis is less favorable, since the disease is difficult to respond to antibiotic therapy due to clostridia spores. The child has been registered with an infectious disease specialist for a long time and is admitted to the children's group only under the condition of complete clinical and laboratory remission and normalization of stool microflora.
Severe pathology with severe ulceration of the intestinal wall, septic manifestations or peritonitis can result in death in childhood. The higher the degree of dehydration, the higher the risk of developing serious complications.
Therapy should be carried out as soon as possible. Children are treated in infectious diseases hospitals, and in severe cases in the intensive care unit.
prokishechnik.info
Diagnostics
If symptoms of an intestinal infection appear, the pathogen is determined using laboratory tests. After specific toxins are identified in the stool and the specific source of the disease is determined, a treatment regimen is drawn up and medications are selected.
The perfringens form is diagnosed comprehensively: based on symptoms and laboratory data. For this disease, it is necessary to have an acute onset, rapid development and the same rapid disappearance of clinical manifestations: vomiting, fever, diarrhea, intoxication. Symptoms are pronounced on the first or second day of illness, and then quickly fade away.
Using an express laboratory method, toxins can be detected in a child’s stool - waste products of clostridia: enterotoxin, neurotoxin or cytotoxin. A blood test shows moderate leukocytosis.
If it is not possible to immediately submit feces to the laboratory, it is placed in a special container and stored in the refrigerator at a temperature of 2 to 8 degrees. Then the laboratory result will be reliable within three days.
To identify intestinal Clostridium difficile, information about a history of recent antibiotic therapy is needed. In feces, studies reveal entero- and cytotoxins, as well as the pathogenic bacteria themselves.
It is impossible to prove the form of clostridiosis difficile only using laboratory data. After all, both the Clostridium difficile bacterium itself and its toxins can be present in the biomaterial of healthy children, especially in babies under six months of age.