Galactosemia is a very rare disease, however, it is worth talking about.
In a healthy person, galactose (a component of lactose) is broken down into carbohydrates, including glucose, as it passes through the digestive tract, which is an essential source of energy for humans. In people suffering from galactosemia, galactose is not completely “digested”; an imbalance of carbohydrates in the body occurs; the kidneys, liver, nervous system and almost the entire body are affected.
What is galactosemia
Galactosemia is a congenital anomaly that develops as a result of the transmission of modified genes from the parents to the fetus. The disease is characterized by a violation of metabolic processes in the body, in particular a disorder in the absorption of galactose. Also, the pathology may not have clinical signs and occur in the form of carriage.
Such mutations are rare; the pathology is diagnosed in one out of 70 thousand newborns. For a long time, nothing was known about the disease - it was first described in 1917, and only by 1956 did specialists manage to figure out the mechanism of its development.
Symptoms of galactosemia
So, why and how does this disease occur? What are the signs of galactosemia?
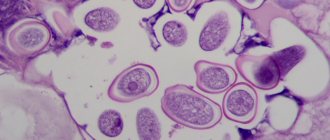
Galactose enters the child's body along with the first food (mother's milk, formula). Due to mutation (damage) of the gene, it is not completely broken down into glucose. Its remnants accumulate in the child’s body - in the tissues, in the kidneys, in the liver. Instant intoxication occurs . The central nervous system and the lens of the eye are also affected, and exhaustion of the body is observed.
In the very first days of the baby's life, obvious jaundice appears, the child refuses food, he constantly vomits, he does not gain weight, and the stool consists of watery diarrhea. The child is also bothered by colic, excessive gas, and becomes lethargic.
In addition, there is involuntary movement of the eyeballs, hypotension, and subsequently mental retardation.
Galactosemia in newborns can manifest itself both very severely and very mildly. In some cases this is only one symptom, in others it is all together.
In severe form, galactosemia in children occurs more often in newborns weighing more than 5 kg. The child spits up after each feeding, has a decrease in blood sugar, watery stools, and bruises appear on the skin.
By two months of life, if galactosemia has not been diagnosed and treatment has not been started, the child develops cataracts in both eyes, severe renal failure, and anorexia.
At three months, the baby develops cirrhosis of the liver, a developmental delay due to damage to the nervous system.
Further, the symptoms include ovarian depletion, mental retardation, alalia, hemorrhage into the vitreous body of the eye, and in very severe cases, sepsis.
Galactosemia, the symptoms of which are severe, can be fatal in the first year of a child’s life.
The average degree of development of galactosemia also contains all of the above symptoms, however, they are not severe and the destruction of the body does not occur so quickly.
A mild form of galactosemia may be almost invisible. There are only symptoms of damage to the nervous system, the child’s refusal to eat and, as a result, exhaustion of the body and digestive problems. You can find out about the presence of this form of the disease if you take a test for galactosemia.
Classification
Galactosemia is divided into several types depending on which enzyme is insufficient for the proper absorption of galactose by the body. The following types are distinguished:
- I – galactose-1-phosphate-uridyltransferase deficiency. It is a classic type of flow. Characterized by the development of jaundice, disruption of the digestive tract and kidneys.
- II – lack of galactokinase. Accompanied by the release of galaxycol, an enzyme that destroys the lens of the eye and leads to the development of cataracts.
- III – insufficient amount of galactose-4-epimerase. With a mild degree of damage, it can be asymptomatic. In more severe cases, it manifests itself as a classic type of galactosemia, accompanied by hearing impairment.
Causes and development of the disease in children
The pathology is transmitted according to an autosomal recessive type, that is, a sick child can only be born if he was conceived by parents who both suffer from galactosemia.
Galactose is an enzyme that must be present in the body to break down food into the state of glucose - a substance that ensures the normal functioning of the kidneys, brain, liver, and cardiovascular system.
After food enters the intestines, the galactose it contains is transported to the liver, where its metabolism must occur. However, against the background of enzyme intolerance, this process is disrupted, and the substance spreads through the bloodstream throughout the body. As a result, there is oxygen starvation of body tissues, dysfunction of the brain, heart, liver, kidneys, eyes, which causes a delay in the psychophysical development of the child.
If a child is a carrier of a mutated gene, then he has no clinical signs.
What is the danger of congenital anomalies - video
Causes
With a disease such as galactosemia, the causes lie in hereditary predisposition. The following factors are also highlighted:
- in normal situations, milk sugar entering the body of a sick baby is broken down into glucose and galactose, and then converted into glucose under the action of an enzyme;
- the cause is gene mutations;
- if there is a lack of the necessary enzyme, metabolic products and galactose itself accumulate in the tissues and blood, producing a toxic effect;
- the liver, organs of vision, and central nervous system are affected.
- metabolic products, such as galaction, cause fluid to accumulate in the eye lens, which causes its clouding and the development of cataracts as a result.
Symptoms
Signs of the development of pathology begin to appear in children a few days after birth. This is explained by the use of infant formula or breast milk, as they contain galactose. The baby has signs of dysfunction of the gastrointestinal tract, kidneys, liver, anorexia, and damage to the visual organs is also noted.
Symptoms of galactosemia
The above symptoms have varying degrees of manifestation and are determined by the severity of the disease.
Light form
If galactosemia is mild, newborns experience vomiting after drinking milk, and babies refuse to breastfeed. Frequent watery diarrhea and flatulence also develop. A blood test determines hypoglycemia - a lack of glucose.
As it develops, malnutrition and delayed mental and mental development are observed. There are also symptoms of chronic liver pathologies in the form of yellowness of the skin.
Moderate severity
If the pathology has reached a moderate degree of severity, the above clinical symptoms are accompanied by an increase in liver size and more severe jaundice. There is a lag in psychophysical development.
Lack of galactose leads to damage to the lens, which causes the development of cataracts. A blood test shows signs of anemia.
Severe form
Severe galactosemia can be recognized by characteristic signs:
- The child experiences severe vomiting after eating dairy foods, as a result of which children refuse to eat altogether. In newborns, the disease manifests itself as hyperexcitability, watery diarrhea, and loss of reflexes. As a rule, the weight of such children exceeds 5 kg at birth.
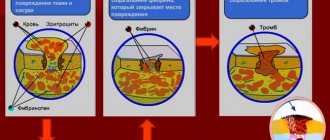
- There is also the development of convulsions, jaundice, and hemorrhages can be found on the skin, which appear due to a deficiency of the factor that ensures normal blood clotting.
- After 1–2 months, kidney failure develops and the lens of the eye is affected. Due to a lack of nutrients, children experience signs of malnutrition.
- Even after a month, the above symptoms are accompanied by signs of liver damage: it increases in size and cirrhosis develops. The functioning of the brain is also disrupted, and ascites may appear.
It is necessary to begin treatment in a timely manner, since severe cases can be fatal due to rapidly progressing failure of vital organs.
Asymptomatic galactosemia
This type of pathology is also called Duarte’s form. It is characterized by the course of the disease without any clinical signs. It is possible to establish the presence of galactosemia only by conducting laboratory tests, as a result of which a deficiency of galactose is detected.
There is another type of pathology - monosymptomatic, when there are only signs of disruption of the digestive organs, brain or the development of cataracts.
Clinical picture
The first symptoms of G. (vomiting, weight loss, jaundice) may appear soon after birth, as soon as the baby begins to receive milk; later, progressive hepatomegaly, ascites, and dyspeptic disorders appear; later, cataracts, areflexia, and delayed psychomotor development appear.
In severe forms of G., death occurs within a few months. In mild forms of the disease, these symptoms are less pronounced, but, as a rule, vomiting, delayed growth and development, hepatomegaly, and cataracts are noted.
The asymptomatic form is accidentally discovered in families in which there are or have been patients with G. Children from these families develop normally; It is typical that they do not like milk and often refuse to breastfeed.
Diagnostics
In order to promptly determine the development of galactosemia in a child, diagnosis can be carried out not only after birth, but also at the stage of intrauterine development. This approach makes it possible to identify pathology in the early stages, prescribe adequate treatment and reduce the risk of complications of the disease.
Prenatal diagnosis consists of conducting studies such as:
- Amniotic fluid analysis. By piercing the woman's anterior abdominal wall, amniotic fluid is collected. They are sent to a laboratory where the level of galactose is determined.
- Chorionic villus biopsy. A small piece of the chorionic membrane of the placenta is collected. Her villi are subsequently examined for the development of galactosemia.
Neonatal screening is carried out after the birth of the fetus in a maternity hospital. Capillary blood is collected, which is applied to filter paper and sent to a genetic laboratory. Such a study is indicated for full-term babies 3–5 days after birth, for premature babies – no earlier than 7–10 days.
If galactosemia is present, the analysis identifies galactose deficiency or low levels of the enzyme that ensures its metabolism.
If the analysis confirms the possible development of galactosemia, it must be repeated. The local pediatrician is notified of the results and will monitor the child’s development. The family should also go to see a geneticist. The doctor conducts a detailed study of the pedigree. If necessary, an examination is carried out to identify the mutated gene.
When the diagnosis is fully confirmed, the specialist prescribes treatment and explains all the nuances of caring for the child and the peculiarities of his nutrition.
Sometimes the following diagnostic methods are used to confirm pathology:
- Urine analysis for the presence of galactose.
- Load tests with the introduction of galactose, glucose.
- General blood and urine analysis.
- Biochemistry of blood. Allows you to identify signs of dysfunction of internal organs.
- Eye microscopy. To determine lens damage.
- Ultrasound examination of the abdominal organs. It is carried out to assess the condition of the liver, kidneys, and intestines.
- Electroencephalography. Allows you to identify and evaluate brain disorders.
- Liver biopsy. It is carried out to exclude the development of cirrhosis.
After diagnosis, the child should undergo regular examinations by a neurologist, geneticist, or ophthalmologist.
Differential diagnosis must also be present if the development of galactosemia is suspected. The disease must be distinguished from insulin-dependent diabetes mellitus, hepatitis, bile duct atresia, cystic fibrosis, hemolytic disease of the newborn, since all these pathologies are accompanied by similar symptoms.
Diagnosis of galactosemia
Since this disease cannot be treated and causes serious harm to the health of the child, it is now customary to do a mandatory test for galactosemia, the so-called screening, even in the maternity hospital . This analysis is carried out during the first week of the baby's life.
An analysis for galactosemia involves taking capillary blood from a newborn, having previously loaded his body with glucose. A positive test shows elevated levels of sugar, particularly galactose, in the blood. The activity of enzymes in erythrocytes is either not detected at all or has a reduced level, and their content can be increased tens of times. If the disease is confirmed after the first test, a repeat test is immediately performed.
Another test for galactosemia involves taking urine and detecting residual glucose in it using chromatography.
Additionally, genetic tests and ultrasound may be prescribed. Genetic analysis allows us to identify the same damaged gene and thus galactosemia is finally confirmed.
Also, modern methods make it possible to diagnose the disease at the stage of prenatal development of the fetus using amniotic fluid analysis. Such an analysis is recommended for women at risk, those who are likely to have a child with galactosemia. Since the disease is hereditary, we are talking about women (and their husbands, partners) in whose families there have already been cases of galactosemia.
In any case, symptoms of galactosemia always occur in the first days after the birth of a child; at the slightest suspicion, the doctor sends the baby for an urgent test.
Treatment
Features of the course of the pathology are determined not only by timely diagnosis, but also by proper treatment. It is based on following a diet that excludes any products that contain galactose, sucrose, lactose, or starch. Children are also prescribed medications.
Medication
Symptomatic medications are prescribed, since it is impossible to influence the very cause of the development of galactosemia. They are used to improve the metabolism and general condition of the child. Typically, the following medications are used:
- multivitamin complexes;
- metabolic process correctors: potassium orotate, Cocarboxylase, ATP (Adenosine triphosphate);
- antioxidants;
- hepatoprotectors;
- calcium preparations;
In severe cases of the disease, intravenous blood transfusion is performed.
It is worth noting that any medications for galactosemia should be prescribed only by a specialist, both for children and adults.
Diet
By following a diet, it is possible to slow down the progression of galactosemia.
First of all, avoid consuming foods containing lactose. Newborns are transferred to artificial feeding and are given special soy-based formulas. As they grow older, they begin to introduce complementary foods according to the following scheme.
Scheme for introducing complementary foods in case of illness - table
| Product | Child's age |
| Fruit juices | 4 months |
| Fruit puree | 4.5 months |
| Dairy-free porridge | About 5–5.5 months |
| Meat | At the age of six months |
| Vegetable oils | 4.5 months |
| Fish | 8 months |
| Cookies, crackers, for the preparation of which milk was not used | 7 months |
| Egg yolk | Not earlier than 1 year |
Products such as:
- milk porridge;
- cottage cheese;
- butter;
- dairy products;
- cookies, crackers, crackers.
Children over one year old should not eat the above foods, as well as:
- sausages;
- legumes;
- spinach;
- offal: liver, kidneys;
- eggs;
- cocoa;
- nuts;
- chocolate;
- soy in its pure form.
Prohibited products in the photo
Chocolate
Nuts
Butter
Spinach
Eggs
Cottage cheese
Legumes
Sausage
This diet should be followed until the age of five. Next, the doctor determines the nature of the disease and draws appropriate conclusions. If the prognosis is favorable and the form is mild, it is recommended to gradually introduce new foods and monitor the body’s reaction. Sometimes, with age, galactose production can increase, resulting in the patient's condition also improving. In severe cases of galactosemia, the diet is followed throughout life.
Forecast
The outcome of galactosemia is determined by the severity of the pathology and timely treatment. If the disease is diagnosed immediately after birth and treatment begins immediately, the prognosis will be quite favorable. This approach helps prevent the development of cataracts, disorders of the brain and liver. In this case, the manifestations of the disease will also be minimal.
If the disease is discovered after it has affected vital organs, the progression of galactosemia can be slowed with medication and diet. Advanced forms of the pathological process in most cases end in death.
Prevention
The development of galactosemia can be prevented only by identifying families that are at risk for developing this disease. The following measures are also used for preventive purposes:
- Screening tests for the development of pathology among all newborns.
- Early detection of galactosemia (prenatal studies).
- If you suspect this disease, you should immediately switch your child to a dairy-free diet.
- Minimizing the consumption of dairy products by women during pregnancy if there is a risk of developing galactosemia.