Beginning of pregnancy - development of the fertilized egg
A fertilized egg is 1 mm – such a small size, but what a significance this bubble already has! The correct determination of the gestational age in the first weeks, the diagnosis of a frozen pregnancy, and the determination of the state of the embryo in dynamics depend on how many mm the fertilized egg has.
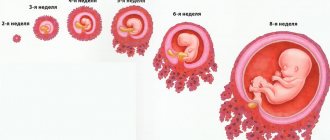
When an expectant mother first comes for an ultrasound, she is usually given a conclusion “early pregnancy” and is recommended to undergo a re-examination in a month. In this case, the conclusion may already include such a parameter as the size of the fertilized egg. It is according to this that the ultrasound doctor is guided when determining the gestational age - after all, obstetricians will count the period from the first day of the last menstruation, and ultrasound sometimes indicates the period from conception (i.e., the age of the fetus). It should be remembered that we are all different, and the development of pregnancy is also different for everyone. Therefore, the article provides average data, which may differ slightly from the real ones. A 1 mm ovum is detected already in the fourth obstetric week of pregnancy - around this time the next menstruation should have occurred. Thus, mommy may not yet suspect the birth of a new life, but it can already be seen on an ultrasound. Usually, if a 1 mm ovum is detected, it is recommended to undergo a re-examination in a couple of weeks - it will be possible to assess the dynamics of its growth, see the heartbeat and determine the exact duration of pregnancy. The fertilized egg is 3 mm - it acquires this size in just a couple of days of development. By this moment, the yolk sac has already begun to form, which is clearly visible on ultrasound - it allows you to differentiate the fertilized egg 3 mm from the fluid bubble in the folds of the uterine mucosa. Thus, a 3 mm fertilized egg in the uterine cavity allows one to accurately determine the presence of pregnancy. If an ultrasound reveals a gestational sac of 3 mm, but the embryo is not visible, there is no need to panic, at this time it simply has not yet had time to develop, and it should not be visible. In just a few days, the fertilized egg will increase in size, and not only the embryo, but also its heartbeat will become noticeable. If pregnancy is diagnosed by ultrasound, a 4 mm ovum will be visible by the end of the fourth obstetric week. The rudiments of the fetal organs - liver, pancreas, lungs - begin to form. The most important organ that is formed at this stage of pregnancy ( fertilized egg 4 mm ) is the heart. In just a couple of days, the heart will begin to beat, and it will be possible to note with relief that the fetus is developing, the pregnancy is progressing! The fertilized egg is 5 mm - it reaches this size by the last day of the fourth week of pregnancy. At this stage, sometimes it is already possible to see the embryo by ultrasound, although its size is no more than a millimeter. A 5 mm fertilized egg is the borderline of the transition from the fourth to the fifth week of pregnancy. The fertilized egg is 6 mm - this is its size that indicates that the fifth week of pregnancy has begun. At this stage, two important events occur - the heart and blood vessels of the embryo are actively forming, and the formation of the nervous system occurs. The embryo reaches a size of 1.5 mm, sometimes at this stage the beating of a tiny heart is already noticeable. Thus, a fertilized egg of 6 mm is a reason to talk about a developing pregnancy. A 7 mm ovum is approximately the middle of the fifth week of pregnancy. The fertilized egg and embryo grow quite quickly, increasing by at least 1 mm every day. A fertilized egg of 7 mm indicates that the embryo is also growing, its organs are forming. If the ultrasound report describes a gestational sac of 7 mm, this usually corresponds to about ten days of delay. However, do not worry if you have a delay of more than two weeks, and the ovum is 7 mm - most likely, ovulation occurred with a delay, and therefore fertilization too. Literally in a day, an 8 mm gestational sac will be visible on an ultrasound scan - this is approximately 5 obstetric weeks and four days. The baby continues to grow along with its shells, and soon it will have limbs. A fertilized egg of 8 mm is an indicator that the sixth week of pregnancy will begin in a few days. A 9 mm gestational sac can be distinguished by ultrasound at 5 weeks and 5 days. Thus, a 9 mm fertilized egg is determined by the end of the fifth week of pregnancy - at this time, the germ cells continue to actively divide, forming the anlage of future organs. A 10 mm ovum is detected at the very end of the fifth week. By this moment, the embryo already has a neural tube with a thickening at its end - this is the future brain. A gestational sac of 10 mm indicates that the formation of the heart and blood vessels is almost complete. A 12 mm ovum is the beginning of the sixth week of pregnancy. At this stage, experienced ultrasound specialists can already determine the fetal heartbeat, although its size is only 2 mm. A gestational sac of 12 mm is an opportunity to catch the pulsation of your baby’s formed heart on an ultrasound. A 13 mm gestational sac is visualized at six weeks and three days. At this point, the baby's heart rate is at least 150 beats per minute. A gestational sac of 13 mm usually allows for good visualization of the embryo. The fertilized egg is 14 mm - it reaches this size by the end of the third day of the sixth week. The baby's arms and legs begin to appear, while still in their infancy. A fertilized egg of 14 mm usually allows you not to worry about the presence of a frozen pregnancy - the embryo is actively developing. A 15 mm gestational sac is visible at 6 weeks and four days. The baby's brain and nerve fibers are formed. If the fertilized egg is 15 mm, a face is already forming, indentations form in place of the eyes, and folds form in the area of the nose and mouth. Fertilized egg 16 mm - corresponds to a period of six weeks and five days. At this point, the digestive system, the rudiments of cartilage and the spleen begin to form. The fertilized egg is 16 mm - at this size, the embryo already has three intestinal loops, the rudiment of the esophagus and stomach. A fertilized egg of 17 mm indicates the close end of the sixth week. If an ultrasound reveals a gestational sac of 17 mm, finger buds begin to form in the embryo. A fertilized egg of 18 mm is determined at the very end of the sixth week. Usually, by the time an 18 mm ovum is formed, muscle tissue has formed in the fetus and it begins to respond to external signals. reaches 19 mm A 19 mm fertilized sac usually contains a fetus measuring at least 5 mm, clearly visible on ultrasound. The fertilized egg is 20 mm – this is the second day of the seventh week. The baby’s brain is actively developing, and a genital tubercle is formed (from which the genital organs will form in the future). The fertilized egg is 20 mm – usually at this moment the mouth and nostrils become visible. The ovum is 21 mm – the fetal face and brain continue to form. A fertilized egg of 21 mm indicates the size of the fetus is at least 8-10 mm. Fertilized egg 22 mm - mid-seventh week of pregnancy. A visible gestational sac of 22 mm allows you to stop calling the baby an embryo - now it is a full-fledged fetus!
WOMEN HEALTH
Tweet
The ovum consists of the fetus, its membranes and amniotic fluid.
FRUIT SHELLS
The aqueous membrane - amnion - is the inner membrane of the fetal sac, directly washed by the amniotic fluid, which is also produced by it. It consists of a thin, vessel-free, transparent membrane, which has two layers: the inner one, facing the fetus, and the outer one, closely adjacent to the chorion.
The amnion has a shiny, smooth appearance. With its outer layer it is fused with the fetal surface of the chorion along its entire length up to the point of attachment of the umbilical cord to the placenta. However, this fusion is only apparent, since it is usually possible to easily separate the transparent translucent thin amnion from the denser, somewhat rougher and less transparent chorion.
The villous membrane, the chorion, is the second membrane of the fertilized egg. The entire chorion is divided into two sections: a branched chorion, consisting of lushly developed villi, and a smooth chorion, completely devoid of villi. In this case, the smooth chorion is the second layer of that part of the fetal sac, which is actually called the membranes of the fetus, while the branched chorion goes to build the placenta.
The sheath that falls off, the decidua, is the maternal tissue. It intimately adjoins the chorion along its entire outer surface. Towards the end of pregnancy it becomes sharply thinner.
The placenta (the old name is the child's place) is formed from the branched chorion. It looks like a thick cake with a diameter of about 18 cm, a thickness of 3 cm and a weight of 500-600 g.
There are two surfaces on the placenta: fetal and maternal.
The fruit surface is covered with amnion. Between the amnion and the underlying chorion, not far from the point of attachment of the umbilical cord, there is a yellowish vesicle, resembling a pea in size and shape. This is a rudiment of the yolk bladder. From it to the umbilical cord there is a whitish thin cord - a rudiment of the vitelline duct. Through the amnion, a well-developed network of blood-filled vessels—arteries and veins—is clearly visible, radiating from the point of attachment of the umbilical cord to the periphery. The caliber of the vessels gradually decreases as they approach the edge of the placenta.
The maternal surface of the born placenta is covered with a matte thin grayish coating, the remnant of the falling membrane. Under the last one you can clearly see 15-20 lobes. The connective tissue of the falling membrane penetrates between the individual lobules and forms partitions between them.
The vascular network of the placenta consists of two systems: uteroplacental and fetal.
The uteroplacental arteries bring blood from the vessels of the uterus to the intervillous spaces of the sheath, from where the blood flows back to the uterus through the uteroplacental veins. In this case, blood circulation occurs slowly, since the uteroplacental vessels are relatively small, and the intervillous spaces are extensive.
Along the edge of the placenta, closed peripheral spaces corresponding to its lobes are often found. They usually contain a small number of atrophied villi. Being part of the intervillous space, they are filled with maternal blood. It was found that these spaces are always separate and never merge with each other along the entire circumference of the placenta, and do not form a continuous channel around the placenta intended for free blood circulation.
In the event of a violation of the integrity of the described formation, blood will flow not only from it, but from the entire intervillous space with which it freely communicates. This can explain the fact known to clinicians that with small sizes of placental abruption (spontaneous placental abruption with normal and marginal attachment, with partial presentation, etc.), heavy bleeding from the uterus is sometimes observed, which in its strength does not correspond to the size of the exposed placental area.
The fetal vessels consist of branches of two umbilical arteries. Each lobule is usually approached by one arterial branch (second-order branch), which, upon entering the lobule, splits into third-order branches. The number of the latter corresponds to the number of villi. The branches of the third order break up into capillaries, the ends of which pass into venous capillaries, which subsequently merge into increasingly larger vessels and, finally, passing into the umbilical vein. Thus, each placental lobule consists of a rich vascular network.
This architectonics of the placental vascular network ensures the isolation of two circulatory systems - mother and fetus. Despite the fact that in this case the blood of the fetus and the mother does not mix anywhere, the exchange of substances between the mother and the fetus occurs quite vigorously through the thinnest membrane of the walls of the capillaries of the villi and their integumentary epithelium.
The functional role of the placenta is very important. Being an organ through which the fetus feeds and breathes, as well as removes its metabolic products, the placenta is also an important endocrine organ. The hormones it secretes, as well as other biologically active substances, play a huge role during pregnancy and childbirth.
The placenta has a relatively small area - about 250 cm2. The entire mass of this organ consists almost entirely of countless individual villi. Therefore, the total functioning surface of the placenta is huge and amounts to 6 m2. This is of great importance (the entire surface of an adult’s body is estimated at 1.4-1.8 m2).
Each placental villi is, in physicochemical terms, a semi-permeable plate through which mutual exchange of substances occurs between mother and fetus due to both the purely physical laws of diffusion and osmosis and complex biological enzymatic processes.
It has been proven that if for some reason half or more than half of the area of the placenta is switched off, the fetus dies from oxygen starvation.
If the circulatory disorder in the placenta is limited to one small area, then a heart attack forms in it. Lime is subsequently deposited in the necrotic tissue and a white infarction is formed. Single small heart attacks do not have a harmful effect on the fetus; with large infarctions, when the respiratory surface of the placenta is significantly reduced, fetal death may occur.
It can now be considered proven that many substances pass unchanged through the placenta to the fetus and back. Thus, oxygen passes from the mother to the fetus, and carbon dioxide passes from the fetus to the mother. Small molecules, such as ammonia, urea and uric acid, can also pass through the placenta.
Glucose, salts, water, some medicinal substances (chloroform, ether, morphine, sulfonamides, antibiotics, bromine, quinine, etc.), as well as hormones and vitamins, also easily pass through the placenta.
A growing fetus has a greater need for proteins. They come to him from the mother's body, having previously passed through the placenta, where they undergo processes of decomposition and partial synthesis. As a result, they reach the fetus mainly in the form of amino acids, which, under the influence of the activity of fetal cells, are combined into protein molecules characteristic of the fetal body. The same processes of dialysis and synthesis are observed during the transition of fats and a number of other substances from mother to fetus.
It goes without saying that waste substances that are no longer needed by the fetus and removed from the woman’s body through excretion enter the mother’s bloodstream through the placenta.
The permeability of the placenta to some microbes, toxins and antibodies found in the mother’s blood deserves attention. However, the transfer of microbes to the fetus becomes possible only after they have previously violated the integrity of the villus. This happens, for example, if a fetus becomes infected from a mother who has malaria, syphilis and other microbial diseases. Viral diseases (measles, influenza, smallpox, etc.) can be transmitted to the fetus even if the villi are intact.
The umbilical cord is an elongated, shiny, smooth, whitish, usually spirally twisted, dense rod that connects the fetus to the baby's place. The length of the umbilical cord is 50-60 cm, diameter - 1 -1.5 cm. Sometimes there are significant deviations from these figures in one direction or another. One end of the umbilical cord is attached to the fetus in the area of the umbilical ring, and the other to the placenta. The attachment of the umbilical cord to the latter can be central, eccentric, marginal or shell; the latter happens in cases where the umbilical cord is attached to the membranes at some distance from the edge of the child's place.
Throughout its entire length, the umbilical cord is replete with bends, bulges and depressions, depending on the characteristics of the development and course of its vessels.
The latter are located in embryonic connective tissue with stellate and spindle cells, called Wharton's jelly. Wharton's jelly forms the basis of the umbilical cord.
In some areas of the umbilical cord there are thickenings formed due to the accumulation of Wharton's jelly in those places where the umbilical cord arteries are sharply twisted (false umbilical cord nodes). Sometimes, as a result of movements inside the fetal sac, the fetus slips through the umbilical cord and forms a true knot.
On a section of the umbilical cord, three vessels are visible: one vein (with a wide lumen, thin-walled) and two arteries. In the center of the umbilical cord there are two thin cords - the remains of the allantois and the vitelline duct. The outside of the umbilical cord is covered with amnion, which, 1 - 0.5 cm short of the navel, passes into the skin of the fetus.
In the umbilical vein you can find doublings of the inner membrane, creating something like valves. Of particular interest are the ring-shaped cushion-shaped protrusions of the muscular and internal layers into the lumen of both arteries, found mainly in the part of the umbilical cord adjacent to the umbilical ring, at a distance of 3-5 cm from each other. Their physiological purpose is that immediately after the birth of a child, when the muscles of the arteries reflexively contract, the ring-shaped protrusions, which are its direct continuation, simultaneously contract and close. In this regard, the vessels close and blood circulation in them stops. This prevents or reduces the risk of blood loss to the newborn if the umbilical cord were left untied for some reason.
The placenta with the umbilical cord and membranes is called the placenta.
You can also read about this topic
Stretch marks in pregnant women. How to warn?
Week Nineteen Tips
Isthmic-cervical insufficiency. ICN
Types of ultrasound. What are SVD and KTR?
To determine the parameters of the ovum, various types of ultrasound are performed:
- Transabdominal - examination occurs through the outer abdominal wall.
- Transvaginal – examination is carried out through the vagina.
With a TA examination, a clear identification of the formation is possible starting from the 5th obstetric week. At this time, the fertilized egg is 5-8 mm in size. Using the second research method, you can determine the size of the fertilized egg on the 3-6th day of missed menstruation, which is 4-5 weeks of gestation. The embryo is visualized starting from the 5th week of pregnancy during a TV examination, and during TA - from the 6th week in the form of a linear formation.
To assess the size and growth of the formation and embryo, the following indicators are used:
- SVD is the average internal diameter of the fertilized egg.
- KTP – coccygeal-parietal size of the embryo/fetus.
SVD shows the size of the fertilized egg by week and is measured in millimeters. Thus, the indicator of the size of the fertilized egg constantly varies over the weeks of pregnancy; the CTE indicator is more accurate for determining the reliable gestation period. In this study, the error may be three days up or down. Basically, the study is carried out up to 12 weeks of gestation.
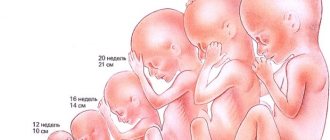
The size of the fertilized egg helps to quickly determine how far along the pregnancy is and how the fetus develops in the womb. The first three months of development are the most important, because it is during this time that all the organs and systems of the future baby are actively developing. Accordingly, it is important to undergo a scheduled ultrasound on time, which helps to identify possible deviations and carry out optimal correction of the current situation.
Author: Lyudmila Morozova,
What are the signs of fertilized egg implantation?
Most women do not feel this process. Some note that during implantation of the fertilized egg:
- Mild aching pain in the lower abdomen appears, reminiscent of menstrual pain.
- There is scanty bleeding, similar to menstruation.
- There may be headaches, nausea, and intestinal upset.
Indeed, at the moment of implantation of the fertilized egg, hormonal changes occur and the body reacts differently to the increase in progesterone in the blood.
On what day of the cycle is the fertilized egg implanted?
The journey of the fertilized egg to the uterus ranges from 2-3 to 6 days. It is not immediately attached to the uterine cavity. After it enters the uterus, it still floats freely for several days. A woman’s body is designed in such a way that after fertilization, real magic happens - her whole body “works” to make pregnancy happen.
To do this, the uterus itself seems to shrink, there is less space in it so that the fertilized egg attaches to the wall as productively as possible. In the wall of the uterus itself, protrusions temporarily form into which the villi of the fertilized egg grow. This occurs approximately on day 19-20 of the standard monthly cycle of 28 calendar days.
Features of the growth and structure of the fertilized egg
The amniotic egg is formed at the moment of fusion of the sperm and the egg; it initially consists of an embryo and a membrane; as the fetus grows, the structure of formation becomes more complex and the volume increases.
The main tasks are to provide the embryo with nutrients, support blood circulation at the initial stage of development, create the basis for the formation of the placenta, secure the fetus in the uterine cavity, and synthesize the hormone hCG.
Stages of formation:
- 7 days after conception, the chorion is formed - the outer dense shell of the embryo, through which oxygen and all useful substances are supplied to the embryo, protecting against infection. As pregnancy progresses, the chorion transforms into the placenta.
- There are many villi located on the surface of the chorion; they help the fertilized egg to gain a foothold in the uterus.
- Gradually, the hairs fall off, remaining only at the site of attachment of the egg to the uterus, the rest of the surface of the chorion becomes smooth.
- On the 20th day after menstruation, the yolk sac is formed - it performs the functions of the liver, kidneys, spleen, the first germ cells, blood cells, and blood vessels are formed in it. The absence of such a sac is a sign of pregnancy pathology.
- Inside the membrane that surrounds the embryo is the amnion, which produces amniotic fluid.
A small round or oval area is the fertilized egg.
Dimensions of the fertilized egg - norms by week
The size of the fertilized egg depends on the gestational age. In the absence of pathological processes, the diameter of the egg increases every day up to 15-16 obstetric weeks by 1 mm, and then by 2-2.5 mm daily. There are certain norms of indicators that allow one to judge the nature of the course of pregnancy; during an ultrasound, the thickness of the chorion is also determined.
Table of the size of the fertilized egg and the thickness of the chorion
| Gestation period (week) | Diameter of embryonic egg (mm) | Chorion thickness (mm) |
| 5 | 5 | — |
| 6 | 10,9–18,1 | — |
| 7-8 | 20,1–25,1 | 7–14 |
| 8–9 | 27,9–33,2 | 8–15 |
| 9–10 | 34,1–42,2 | 8,5-9,5–16,5–1,5 |
| 11 | 50 | 10–18,5 |
| 12 | 56-62 | 11,5-19 |
| 13 | 62–67 | 12,5–20 |
Reasons for deviations
A long-awaited pregnancy is a condition in which women are very suspicious; they can be upset and alarmed by anything. Especially - incomprehensible and complex terms that a doctor can use when determining the size of the ovum. For example, the concept of “deformed” can be confusing. There is nothing to worry about - in 90% of cases the egg is deformed due to increased tone of the uterine muscles.
At 10-14 weeks of pregnancy, a woman undergoes an ultrasound examination, which allows the doctor to take measurements of the ovum to determine the exact gestational age. Sometimes during the examination a deformed fertilized egg is discovered. The main cause of this pathology is considered to be an increase in uterine tone.
Why does the uterus become toned? Doctors identify several reasons:
- Psychological. The nervous situation in the family and at work, personal fears associated with the course of pregnancy cause stress in a woman. There is general tension in the body, which also affects the condition of the uterus.
- Infectious. Diseases of an infectious nature provoke an inflammatory process that negatively affects the muscle tissue of the uterus and leads to an increase in its tone.
- Intimate life. Violent sexual intercourse during pregnancy actively affects the reproductive organ, causing it to overstrain.
- Hormonal imbalance. Improper hormone production can lead to endometrial growth. Filling the uterine cavity, it negatively affects the surrounding structures, which is how an irregularly shaped fertilized egg is formed.
- Physical activity. Passion for physical exercise provokes tension in the muscle tissue of the uterus and tones it.
During pregnancy, the uterus has heightened sensitivity to any irritants. Even a simple palpation of the abdomen or a short jog can tone it down. However, these are temporary phenomena and are not considered serious disorders. A cause for concern is the frequent manifestation of increased uterine tone and an elongated outline of the egg. With such signs, the doctor is forced to constantly monitor the condition of the organ and the course of pregnancy.
Ultrasound can recognize the fertilized egg in the third week after conception. On the sixth day, the basis of the embryo is clearly visible and the heartbeat of the unborn baby can be heard. Initially, the fertilized egg looks like a small transparent ball. By the 5th week of its development, the so-called gall sac is already present, which supplies the fetus with nutrition. The size of the fertilized egg during this period is already more than 2 mm. It can be seen as a black spot on the ultrasonic screen.
If the pregnancy test result is positive, the fertilized egg may be absent from the uterus for various reasons:
- False test results.
- Ectopic pregnancy.
- The ultrasound is performed too early and the fertilized egg has not yet implanted in the uterus.
In this case, additional tests, such as a blood test for hCG, are needed to understand what is happening.
Deviations from parameters
The growth and size of the fertilized egg and embryo must correspond to the duration of pregnancy. If the fetus is less than 2 mm in size at 5 weeks, a developmental disorder can be stated. Fetal size less than 4 mm at seven weeks so
also indicates a violation. With these parameters, you need to make sure that the set deadline is correct.
A large fertilized egg with a small embryo often indicates a frozen pregnancy. But re-examination is necessary to confirm. A frozen pregnancy can also be indicated by a too small fertilized egg. However, again we need to observe the dynamics of development.