In children, acute intestinal infections (abbreviated as OKI) are common. This disease can have a different nature - bacterial or viral, therefore, the doctor must decide how to treat a sick child. Parents need to know what to feed their child with an intestinal infection.
A properly formulated diet is one of the main components of successful treatment. After all, with OCI, inflammation and irritation of the mucous membrane of the gastrointestinal tract is observed, so food must be selected so that it does not aggravate the situation.
Signs of infection
The disease can be caused by some viruses and bacteria such as dysentery bacillus, salmonella, childhood staphylococcal infection, typhoid bacillus, and vibrio cholera. Some of them enter the body when drunk with water, with food through vegetables, eggs or dairy products.
After entering the stomach, pathogenic bacteria begin to actively multiply, which leads to disturbances in the digestion process and inflammation of the cells of the mucous membranes of the gastrointestinal tract.
One of the first manifestations of an intestinal infection is loose stools (diarrhea), secondary symptoms include nausea, vomiting, fever, general malaise, and lack of appetite.
Diet after antibiotic treatment
As a rule, treatment of acute intestinal infection is carried out with the use of antibiotics, which interferes with the normal functioning of the gastrointestinal tract. To restore the functioning of the gastrointestinal tract during the treatment period, it is necessary to adhere to the following recommendations: drink plenty of fluids, be sure to follow a diet for intestinal infections in a child, comfortable rest and feeding only as desired. It is necessary to follow the prescribed rules for several weeks after recovery, and then gradually switch to a normal diet.
Basic principles of menu design
As a result of poisoning, the digestive organs and all mucous membranes become inflamed, the normal functioning of the liver and pancreas is complicated, gastric juice ceases to be secreted in the required quantities, and muscle tone weakens.
To promote the speedy restoration of the functions of the gastrointestinal tract, you must adhere to the following rules:
- Grinding to a puree and heating the food is mandatory.
- Minimize the consumption of fats and foods containing fiber.
- Relieve the child's stomach and intestines, feed little by little, every 2-3 hours.
- Do not force him to eat if the baby has no appetite.
- A vitamin and mineral complex will replenish nutrients lost during illness.
- If possible, you should maintain a separate diet, with an emphasis on boiled vegetables.
- Dishes should be varied and tasty, since illness increases the requirements for taste.
- Vegetables and fruits should only be eaten after thorough washing and scalding with boiling water.
- Drink only boiled or bottled water.
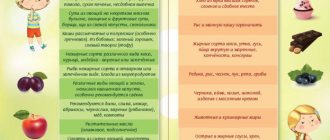
Products that should be included in the daily diet menu for intestinal infections in children: porridge, only boiled vegetables, yesterday's white bread, jelly, compote and broth, dietary meat - chicken, rabbit or turkey, sea fish.
Strictly prohibited
Pork is prohibited after an intestinal infection.
Recovery from an intestinal infection is a little depressing for a child, but there’s nothing you can do – you have to endure it.
And if there are foods that will benefit the baby, there are also those that are strictly forbidden to eat. So, it is prohibited:
- Fatty meats (pork, lamb, chicken wings and legs) and fish (salmon, trout, mackerel). These products are prohibited due to the fact that they are very fatty, and the baby’s body is not able to digest fatty foods due to a decrease in enzyme activity caused by an intestinal infection.
- Brown bread, fresh baked goods, black crackers. This is due to the fact that bread enhances peristalsis, and baking, in turn, provokes the formation of a fermentation process.
- Strong broths. It is forbidden to use strong broths, because The child has an enzyme deficiency.
- Fresh vegetables and fruits. Prohibited because fresh vegetables and act as stimulants of intestinal peristaltic movement.
- Juices, berries, sweets, chocolate, cakes.
This video will tell you about food poisoning:
Desoldering
With an acute intestinal disorder, there is a risk of large loss of fluid - dehydration, which negatively affects the functioning of the entire body, as essential minerals are lost.
With diarrhea and vomiting, the child loses a lot of water, but stopping diarrhea using medications is prohibited. This is a kind of protective reaction that allows the body to get rid of toxins and infections.
At this stage, it is necessary to restore the water-mineral balance using special solutions. For this, both pharmacy powders and a drink prepared with your own hands according to the following recipe are suitable: 8 teaspoons of sugar, 0.5 spoons of baking soda, one spoon of salt are dissolved in a liter jar of boiled, not hot water. Throughout the day, at five-minute intervals, give the child a teaspoon of prepared water. Children over 3 years old can drink several large tablespoons at intervals of 15 minutes.
Weak tea, rosehip decoction and dried fruit compote, but without prunes, are also suitable as a medicinal drink. During the recovery stage, you can cook jelly for the crumbs, since starch, enveloping the mucous membranes, helps them recover.
Symptoms and first aid
The first symptoms that appear in a child are nausea, frequent vomiting, and diarrhea. Children complain of abdominal pain, their temperature rises, and weakness appears.
In this case, first of all, isolate the child from other family members, especially other children, since the disease is contagious. Be sure to give something to drink: just boiled water, mineral water or dried fruit compote. Peppermint tea is good for reducing nausea. You can also use special medicinal solutions to replenish not only fluid in the child’s body, but also minerals that are lost along with vomiting and diarrhea.
Dehydration during illness is especially dangerous for a child’s body, especially for young children.
Drinks should be given little by little, approximately 1–2 tsp. every 5-10 minutes to reduce gagging. For children, it is mandatory to call a pediatrician at home. If you have serious concerns about your baby's health, call an ambulance.
Restrictions on feeding newborns
Treatment of intestinal infection in children involves restrictions on the consumption of carbohydrate foods, milk and milk-based products, since they all contain lactose (milk sugar). This limitation is due to the fact that in acute intestinal disorder, milk sugar begins to ferment in the small intestine, and as a result, excessive gas formation, flatulence and colic occur. That is why formula-fed infants are given formulas with a low lactose content or completely without it during the acute period.
If feeding occurs with breast milk, its dosage should not differ from the diet before the disease by more than 40%, since protective antibodies are present in such milk. It is recommended to increase the number of feedings, but the main guideline should be the child’s appetite.
Initially, the digestive organs of newborns are imperfect, but among the acids and bile it contains taurocholic acid. It is of great importance in the fight against unnecessary bacteria and viruses and has antiseptic properties.
The role of therapeutic nutrition in acute intestinal infections in children
| Summary: Acute intestinal infections (AIE) are the most common cause of diarrhea in childhood. Treatment of acute intestinal infections in children depends on the type of diarrhea, clinical data and pathogen. For watery diarrhea, rehydration plays a major role. Regarding invasive diarrhea, antibacterial treatment is indicated in some cases. It is now believed that early return to a normal diet contributes to shorter disease duration. However, this is not always possible with OKI. In this regard, the issue of nutritious nutrition, which should be easy to digest, becomes of particular importance. Complete balanced formulas intended for children from 1 to 10 years of age that can be used for acute intestinal infections are Peptamen Junior and Clinutren Junior. | Summary: Acute intestinal infections take the second place in the structure of infectious diseases. Therapy of intestinal infections in children depends on type of diarrhea, clinical data, etyology. The rehydration therapy is the first help in watery diarrhea in children. Antibacterial therapy is recommended in some cases of invasive diarrhea.As concerns diet, early return to usual diet reduces the duration of a disease. Usually it is impossible in acute intestinal infections in children. The question is how to restore a child's health after disease and prevent development of a new one. So it is necessary to provide a child with complete and balanced nutrition, which is easy to digest. The best choice is Peptamen Junior and Clinutren junior - therapeutic and preventive nutrition for the children from one to ten years old. |
| Key words: Acute intestinal infections in children, invasive diarrhea, watery diarrhea (secretory or osmotic), rehydration therapy, antibacterial therapy, Peptamen Junior, Clinutren Junior. | Key words: Acute intestinal infections in children, antibacterial therapy, invasive diarrhea, watery diarrhea (secretory or osmotic), rehydration therapy, antibacterial therapy, Peptamen Junior, Clinutren Junior. |
All intestinal infections can be divided into 3 groups1:
- intestinal infections of a bacterial nature (shigellosis, salmonellosis, yersiniosis, cholera, etc.);
- intestinal infections of a viral nature (rotavirus infection caused by adeno-, enteroviruses, Norfolk group viruses, etc.);
- intestinal infections of protozoal etiology (amebic dysentery, etc.).
The summer-autumn period (peak – August–September) is characterized by bacterial acute intestinal infections, and viral acute intestinal infections are more common in the cold season: late autumn, winter and spring.
The main mechanism of transmission of intestinal infection is fecal-oral, carried out through food, water and household contact. Moreover, in the case of bacterial infections, the food and water routes are of greater importance, and in the case of viral diarrhea, water and contact routes are of greater importance. In the warm season, potential bacterial pathogens have more opportunities to multiply in food products, and there is a higher likelihood of consuming contaminated fruits, vegetables, herbs, and poor-quality water.
In a situation where etiological diagnosis is difficult, as well as in the first hours of the disease, clinical manifestations can suggest a bacterial or viral etiology of acute intestinal infections, which is important for the correct management of the patient.
Knowing the pathogen is of great importance. Bacterial or viral acute intestinal infection are two different variants of the course of intestinal infection; naturally, the therapy is also different. The pathogenetic mechanisms of development of bacterial and viral infections also differ.
Based on the type of diarrhea, intestinal infections are divided into 3 pathophysiological options:
- osmotic;
- secretory;
- invasive.
Bacterial pathogens usually cause invasive and secretory diarrhea, while viral pathogens usually cause osmotic diarrhea. A mixed version of diarrhea is possible.
Invasive diarrhea is initiated by the introduction and invasion of pathogens into the intestinal wall, which is accompanied by the development of local inflammation and increased permeability of cell membranes. As a rule, the pathological process is localized in the large intestine. Invasive diarrhea is characterized not so much by copious stools, but by various inclusions in the form of pus, blood, mucus, and greens. Stool may be frequent, but not large. Severe intoxication, fever, pain mainly along the colon, and tenesmus are typical.
In contrast to invasive diarrhea, the secretory and osmotic variants are watery diarrhea.
Secretory diarrhea is accompanied by intestinal hypersecretion associated with impaired electrolyte transport in the intestine and caused by bacterial exotoxins. The pathological process is usually localized in the small intestine. Secretory diarrhea is clinically manifested by frequent watery loose stools with undigested food debris, water and electrolyte imbalances, moderate manifestations of intoxication, and a slight increase in temperature.
Osmotic diarrhea, usually viral, is caused by the formation in the intestine of osmotically active substances (disaccharides, including lactose), due to the development of secondary disaccharidase (lactase) deficiency, which retain fluid in the intestinal cavity. This diarrhea is characterized by bloating, a moderate increase in stool volume, and frequent, foamy stools with remnants of undigested food.
The next difference that helps distinguish a bacterial infection from a viral one is the location of the lesion. Viral infections, as a rule, occur in the form of acute gastritis, gastroenteritis (vomiting, watery diarrhea). Bacterial diarrhea (secretory, invasive, mixed) can also occur as gastritis and gastroenteritis, but the lower intestine is often affected, that is, enterocolitis and colitis are more typical for bacterial intestinal infections. Thus, depending on the clinical manifestations, we can assume the localization of the lesion (gastritis, gastroenteritis or, for example, enterocolitis) and the possible pathogen. After this, depending on the severity of the disease, certain therapeutic measures are carried out2.
Acute intestinal infections are often accompanied by the development of secondary digestion and absorption disorders (secondary enzymopathies), which can aggravate the situation and contribute to the development of prolonged diarrhea and exhaustion of the body.
First aid for acute intestinal infections is the fight against dehydration. Watery diarrhea, especially accompanied by high fever, is dangerous due to rapidly developing dehydration. Therefore, rehydration therapy, for which glucose-saline solutions are used, is of paramount importance. If a viral infection is suspected, then antibiotic therapy is not indicated. In the case of a suspected bacterial infection, in some cases, you should consider prescribing an antibacterial drug3,4.
In terms of diet, it is now believed that both infants and older children are advised to stick to their normal diet. If we are talking about infants, then, of course, it is best to drink breast milk; you can temporarily refuse complementary feeding. If we are talking about older children, then frequent meals in small portions are necessary. Avoid coarse fiber, fresh fruits and vegetables, all gas-forming foods, fried and fatty foods. Early return to a normal diet is thought to contribute to a shorter duration of illness. However, this is not always possible with OCI, since intoxication, fever, vomiting, and loose stools reduce appetite. In addition, damage to the gastrointestinal tract does not contribute to the normal digestion of foods. In this regard, the issue of adequate nutrition is of particular importance. In this case, the main condition for impaired functioning of the gastrointestinal tract is the easy digestibility of this food. Complete balanced formulas intended for children from 1 to 10 years old are Peptamen Junior and Clinutren Junior.
These mixtures can be used as a sole source of nutrition or as a supplement to regular food in children with various gastrointestinal problems. The protein component of the Peptamen Junior mixture is represented by peptides, which are obtained as a result of the hydrolysis of whey proteins, which eliminates the development of allergic reactions in children. Such protein is easier to digest and absorb, promotes rapid gastric emptying, which reduces the risk of vomiting. Due to the high level of cysteine, it provides an anti-inflammatory effect. Peptamen Junior contains fats (medium chain triglycerides), which do not require digestive enzymes for their absorption, but are a good source of energy for the body. The mixture contains an optimal ratio of omega 6: omega 3 (7:1) fatty acids, which helps the child’s body fight inflammation. The “sweet part” of the mixture is represented by broken down starch (maltodextrin), which any child can digest, even with damaged intestines. This mixture is preferably used during the acute period of the disease (ACI) not only as a nutritional, but also a therapeutic component, since it helps normalize water balance, helps restore the integrity of the intestinal mucosa, replenishes the lack of energy and vitamins necessary for the body, and reduces the severity of vomiting and diarrhea5.
In the end of the disease, after the acute symptoms have stopped, but weakness and asthenia remain, it is recommended to switch to Clinutren Junior for a quick recovery. The Clinutren Junior mixture contains easily digestible whole milk proteins (a mixture of caseins and 50% whey proteins), which are easily broken down and absorbed in the gastrointestinal tract, helping to strengthen the immune system. The “sweet part” is also represented by maltodextrin. Just like Peptamen, but in smaller quantities, Clinutren Junior contains medium-chain triglycerides - fats that are broken down and absorbed without the participation of pancreatic enzymes, while providing the body with “fast” energy. Both mixtures contain vitamins and microelements necessary for the child’s body. The most important role in maintaining immunity is played by vitamins A, C, E and the trace elements selenium and zinc. Clinutren Junior contains two probiotics (Lactobacillus paracasei, Bifidobacterium longum) and prebiotics (dietary fiber), which help increase the number of “good” bacteria in the child’s intestines, which also activates the immune system and improves the functioning of the gastrointestinal tract. It should be noted that both mixtures do not contain gluten and are low-lactose (contain minimal, clinically insignificant amounts of lactose), which is important for the development of secondary enzymopathies.
Equally important, especially in pediatric practice, are good tolerability and good organoleptic properties of these food products. Therapeutic mixtures Peptamen Junior and Clinutren Junior have physiological osmolarity. The vanilla flavor of the mixtures is of particular importance for children.
Thus, the use of these mixtures for acute intestinal infections promotes rapid recovery and restoration of the child’s body after an illness.
Bibliography:
- Uchaikin V.F., Novokshenov A.A., Sokolova N.V. Etiopathogenetic therapy of acute intestinal infections in children at the present stage. Attending Physician 2010;1:7-13.
- Practice parameter: the management of acute gastroenteritis in young children. American Academy of Pediatrics, Provisional Committee on Quality Improvement, Subcommittee on Acute Gastroenteritis. Mar 1996;97(3):424-35.
- World Health Organization. The treatment of diarrhoea: a manual for physicians and other senior health workers - 4th revision.
- Guarino A., Albano F., Ashkenasi S. et al. ESPGHAN/ESPID Evidence-based Guidelines for the Management of acute gastroenteritis in children in Europe. J Pediatric Gastroenter Nutr 2008;46(2):81-184.
- Flack S., Lawson M., Milla P. (2003) Experience with a new hydrolysed feed in a pediatric gastroenterology clinic. J Hum Nutr Diet. 16:365-70.
Nutrition for a child over one year old
Children after one year are recommended to adhere to diet therapy during the acute stage of the disease and two to three weeks after it. At this time, the intestines are restored after an attack by an infectious agent.
Dietary recommendations:
- The breaks between meals are reduced, as is the portion size.
- It must be remembered that the digestion process in the intestines will not be stopped even with the most severe inflammation, so the amount of food eaten is reduced only in severe cases of the disease by no more than 50%.
- You need to cook in a double boiler or by boiling food; it is best to give food to your child in puree form, since this is the easiest form for the intestines.
- Be sure to have sufficient protein in the menu.
- It is necessary to exclude all foods that cause gas formation and fermentation, as well as whole milk.
- Fermented milk products will bring the greatest benefit, as they contain amino acids and vitamins (B and C), which are necessary for the formation of new intestinal epithelial cells.
For a month, it is necessary to eat food with a liquid and creamy consistency, then it smoothly turns into a mushy consistency; food is served only warm, so as not to provoke irritation of the mucous membranes of the gastrointestinal tract. It is advisable to completely exclude the following dishes from the menu: saturated and fatty broths, pickled and pickled vegetables, rye bread, raw vegetables and fruits, legumes, any juices and sauces, sweets (sweets, ice cream, cakes) and carbonated drinks.
Nutrition during recovery
When the acute period of the disease is over, intoxication has disappeared, vomiting and diarrhea have passed, the infection has been eliminated, recovery from an intestinal infection occurs, and the little one is recovering, it is allowed to gradually add new products to the menu, increase the amount of food, but subject to a number of conditions.
Such as:
- A week after the main symptoms disappear, you can add applesauce or bananas to your diet.
- Whole milk is excluded for the entire recovery period (for a month).
- Pasta can be given twice a week.
- Include some sweets - marmalade, marshmallows or marshmallows.
- Fermented milk products are offered with higher fat content.
- Boiled yolk or steamed omelet is allowed no more than twice a week.
The introduction of new products is in its own way similar to the introduction of complementary foods to infants: it starts with one spoon, and the next day the dose is given twice as much. In this case, you need to pay attention to the consistency of the stool and the general well-being of the child: if the tummy does not hurt, the stool is normal, you can safely add the product to the menu.
In a diet after an intestinal infection in a child, the addition of vegetables and fruits is left for last, with mandatory heat treatment, pureed. First add those that have the best digestibility: zucchini, pumpkin, broccoli, cauliflower, carrots and broccoli.
You can add crackers or dry unsweetened cookies, crackers from white or gray bread. It is imperative to observe consistency and gradualism, since the appearance of a new product on the menu in large quantities at once can provoke attacks of vomiting or diarrhea.
Basic nutritional requirements in the acute period
Previously, it was believed that in case of ACI it was necessary to take “hunger breaks” or, in extreme cases, give the child only tea and crackers. Modern pediatricians abandon this principle, believing that fasting is not beneficial for a one-year-old child and even for a 3-4 year old child. At this age, fasting greatly weakens the body and slows down the recovery of damaged mucous membranes.
Of course, there is no need to force feed a child during an intestinal infection. But if the baby has an appetite, then you should definitely give him something to eat, but you just need to select the food correctly.
For example, Dr. Komarovsky recommends using the following diet principles:
- food should be gentle, both chemically and mechanically. That is, you need to choose easily digestible foods that do not irritate the gastrointestinal mucosa, and give them in the form of purees;
- products must be boiled or steamed;
- limit the amount of fat, table salt, and carbohydrates in the diet;
- meals should be small, but frequent. So for a child aged 2 years, the size of a single serving should not exceed 50 grams, but the number of feedings should be increased to 8 times;
- food should have a temperature between 33-37 degrees, that is, not cold or hot;
- It is useful to include lactose-free or low-lactose fermented milk products enriched with bifidobacteria in the diet.
It is necessary to completely exclude from the diet all foods that stimulate intestinal motility or enhance fermentation processes.
Prevention
The root cause of intestinal infection is recognized to be failure to follow basic rules: untimely washing, not washing hands thoroughly or not at all, improper way of storing food, etc. At home, first and second courses and open dairy products can be stored outside the refrigerator, turning into a breeding ground for bacteria.
Fruits and vegetables are simply rinsed under running water and do not have time to be properly washed. Often mothers and grandmothers offer the baby to eat outside, at best, wiping the hands with a damp napkin.
Prevention of intestinal infection is very simple: hand washing, heat treatment, compliance with the terms and rules of food storage (in clean containers with a lid). If you follow all these rules, you can not be afraid of intestinal infections and feed your child plenty of fresh fruits and vegetables.
What products are prohibited
All fried, salty, spicy foods, any smoked foods, sausages and preserves should be excluded from the child’s menu. Among vegetables and fruits, in case of intestinal infection, it is forbidden to eat fresh greens, all legumes, fresh fruits and vegetables - beets, carrots, cucumbers, tomatoes. It is worth giving up mushrooms and nuts. You should avoid sour berries and fruits.
As for flour products, you should not give fresh bread, as well as bread made from rye flour, all baked goods, cakes and pastries. Sweets should be sharply limited: exclude sweets, chocolate, sweet cookies. And you should also not offer your child packaged juices from the store or coffee. Fatty meat and strong meat broth are not the best option for a diet with an intestinal infection. As for dairy products, you should absolutely not consume milk and kefir.