How to help your child with a wet cough
Any expectorant helps remove mucus from the lungs. Due to the liquefying effect, mucus with harmful microbes leaves the body without difficulty. A cough expectorant can be prepared at home. They are suitable for children 2 years and older. Up to 1 year, homemade mixtures and decoctions should be given only after consultation with an experienced doctor.
Expectorants for children are offered in a variety of ways by pharmaceutical companies. Self-medication is not the best choice of therapy for young patients . In 60% of cases, such actions only worsen the child’s condition and lead to chronic diseases.
If the baby is not yet 5 years old, then bronchospasm may indicate bronchitis. This disease is characterized by severe swelling of the mucous membrane of the respiratory organs. Warming up in this case is contraindicated. It is generally advisable to call an ambulance or a local pediatrician, who will select competent therapy.
The use of mucolytic drugs for cough in children
Often, the process of “physiological” cough, which is necessary for the body, is significantly hampered due to the influence of a number of factors. For example, during inflammatory processes in the respiratory tract against the background of respiratory diseases, the formation of bronchial secretions significantly increases. This is accompanied not only by an increase in volume, but also by a significant change in the composition of the secretion due to an increase in the concentration of mucins, which ultimately leads to an increase in the viscosity of sputum. This circumstance causes a decrease in the activity of the cilia of the ciliated epithelium, which promote sputum from the respiratory tract. And finally, inflammation is accompanied by swelling of the mucous membrane of the respiratory tract, which leads to impaired bronchial obstruction. As a result of these numerous changes, conditions are created for the accumulation and stagnation of sputum, which, in turn, becomes favorable soil for the proliferation of pathogenic microorganisms in the respiratory tract [2]. It is important to consider that under conditions of sputum stagnation in bronchial secretions, the content of a number of local immunity factors that have antiviral and antimicrobial activity decreases. Consequently, local immune defense is suppressed. In such circumstances, the insufficiency of mucus evacuation mechanisms must be compensated by increased coughing. However, this is hampered by the increasing viscosity of sputum, the removal of which requires very significant efforts, which results in a prolonged, severe and unproductive cough with a small amount of sputum [3]. Infectious and inflammatory diseases of the respiratory system in children are almost always accompanied by a cough (dry or wet, unproductive or intrusive) with the release of copious, scanty or viscous sputum. In addition, it is necessary to take into account the anatomical and physiological features of the structure of the bronchopulmonary system in children, especially young children, namely: short and wide bronchi, insufficient development of the bronchial tree, richly vascularized mucous membrane, the special state of the lymphoepithelial tissue of the pharyngeal ring, which is involved in the formation of local immunological reactions, etc. A feature of the child’s body of this age is also the insufficient viability of the physiological mechanisms of sanitation of the tracheobronchial tree [2–4]. The complex treatment of patients with respiratory diseases, and especially with chronic and recurrent inflammatory diseases of the respiratory system, along with adequate hydration, includes medications that help reduce the viscosity of sputum and improve its excretion. Table 1 presents the main groups of drugs used in the treatment of cough. It should be noted that many of the drugs listed in the table have a variety of side effects described. For example, when using libexin, nausea, diarrhea, skin rash, and angioedema were noted; sinekoda – dizziness, nausea, diarrhea, skin rash; broncholithin - tachycardia, increased blood pressure, tremor, agitation, drowsiness, nausea, vomiting, constipation, difficulty urinating, rash, increased sweating; tussina plus - nausea, vomiting, diarrhea, drowsiness, etc. [5]. Among modern expectorants, a special place is occupied by drugs with the so-called mucolytic effect. They are able to quickly dilute sputum, restore the mucous membranes of the bronchi and impaired elasticity of the lungs. According to the mechanism of action, mucolytics are not a means of influencing the main pathogenetic link of the disease - the inflammatory reaction, but only affect the symptoms of the disease, i.e. are drugs for symptomatic therapy [3]. Expectorants are most often used orally in the form of drops, tablets, syrups; some medications are available in suppositories, others are intended for inhalation; in severe diseases, intramuscular and intravenous administration is possible. These drugs include numerous drugs: bromhexine, acetylcysteine, carbocysteine, ambroxol (Lazolvan®, etc.) [2,3,6]. One of these drugs, widely used in pediatric practice, is Lazolvan® (ambroxol), which is an active metabolite of bromhexine, a synthetic derivative of the alkaloid vasicine. The developed ambroxol hydrochloride was first registered in Germany in 1978. Currently, various forms of release of this drug are registered in more than 80 countries and are successfully used to treat diseases of the respiratory tract, accompanied by changes in sputum secretion and difficulty in its evacuation. Ambroxol hydrochloride, which is the basis of the drug, thins sputum by stimulating the serous cells of the glands of the bronchial mucosa, normalizing the ratio of mucous and serous components of sputum, stimulates the production of enzymes that break down the bonds between mucopolysaccharides of sputum, stimulates the production of surfactant, which also normalizes the rheological parameters of sputum, reducing it viscosity and adhesive properties. The drug directly stimulates the movement of the cilia of the bronchial epithelium and prevents them from sticking together, facilitating the evacuation of sputum. Ambroxol normalizes the functions of altered serous and mucosal glands of the bronchial mucosa, helps to reduce mucosal cysts and activates the production of the serous component [1]. Thus, ambroxol promotes the production of qualitatively changed secretions. Literature data indicate the anti-inflammatory and immunomodulatory effects of ambroxol. The drug enhances local immunity by activating tissue macrophages and increasing the production of secretory IgA. Ambroxol has a suppressive effect on the production of inflammatory mediators (interleukin 1 and tumor necrosis factor) by mononuclear cells, and also enhances the natural defense of the lungs, increasing macrophage activity. It has been proven that ambroxol has anti-edematous and anti-inflammatory effects, effectively helps relieve exacerbations of chronic bronchitis and significantly reduces the risk of developing bleomycin-induced pulmonary fibrosis. Since ambroxol is used in the treatment of patients with obstructive bronchitis, the effect of the drug on the course of broncho-obstructive syndrome is of interest. KJ Weissman et al. showed a statistically significant improvement in indicators of external respiratory function in patients with broncho-obstruction and a decrease in hypoxemia while taking ambroxol [7]. Ambroxol is widely used for respiratory diseases of bacterial etiology. A number of studies have been devoted to studying the effectiveness of the combined use of ambroxol and antibiotics. It has been shown that the combination of the drug with antibiotics has an advantage over the use of a single antibiotic. Ambroxol helps to increase the concentration of the antibiotic in bronchial secretions, which improves the course of the disease in bacterial lung infections. In controlled studies, it was found that the combination of Lazolvan with antibiotics such as amoxicillin, erythromycin, doxycycline and cephalosporins leads to an increase in their concentration in bronchial secretions in patients with chronic obstructive pulmonary diseases. Therefore, the use of the drug is quite justified in inflammatory processes of an infectious nature [1,6]. In patients with bronchial asthma and recurrent bronchitis, improvement in the rheological properties of sputum leads to more pronounced positive dynamics of external respiratory function indicators, which reflects the ability to more actively influence the improvement of external respiratory function indicators in this pathology. The results of clinical observations show that Lazolvan® is an effective drug that has a mucolytic effect, improves sputum expectoration and reduces the intensity of cough. The use of Lazolvan promotes faster elimination of symptoms of exacerbation of the bronchopulmonary process and alleviates the condition of patients. The positive dynamics of clinical symptoms is accompanied by an improvement in respiratory function indicators. These data are confirmed by clinical observations in adult patients. The drug is well tolerated by patients of any age. A feature of the pharmacokinetics of Lazolvan after oral administration is its rapid and almost complete absorption, but up to 20–30% of the drug is metabolized during the initial passage through the liver. After taking 30 mg of the drug, the maximum concentration is observed after 2 hours and reaches 88.8 mcg/ml. The duration of action after taking one dose is 6–12 hours. When administered by inhalation, the therapeutic effect of the drug also develops quickly - after 30 minutes. and lasts for 6–12 hours. The maximum effect is observed already on the 2nd day. Lazolvan® is able to penetrate into the cerebrospinal fluid, through the placenta, and into breast milk. It is important to take into account that the drug has a high level of safety and can be used in pregnant women (in the second and third trimester) and newborns (solution for inhalation and oral administration and syrup 15 mg/5 ml) [6]. Important effects of Lazolvan are relief of chest pain when coughing (due to a decrease in its intensity), acceleration of the penetration of antibiotics into the lung tissue [9], and improvement of local immunity of the respiratory tract. It does not contain sugar or alcohol, therefore, unlike other mucolytic drugs, it can be used in patients with diabetes mellitus or with impaired glucose tolerance. One of the advantages of Lazolvan is that it has no contraindications for use in gastric and duodenal ulcers. The drug has a long shelf life: for tablets, syrup 30 mg/5 ml and solution for oral administration and inhalation - 5 years, syrup 15 mg/5 ml - 3 years. The variety of dosage forms of Lazolvan allows for an optimal course of treatment depending on the patient’s age and individual characteristics, which is very important in pediatric practice. Lazolvan® has four dosage forms: syrup, tablets, solution for inhalation and oral administration, and lozenges [8]. An important condition for treatment with Lazolvan is compliance with the drinking regime: additional amounts of liquid should be used to more effectively dilute sputum. The last dose of the drug should be no later than 6 pm, otherwise the mucolytic effect and drainage activity will occur in the child during sleep. Incorrect administration of ambroxol hydrochloride in the evening is the most common mistake in pediatric practice. A prerequisite for using Lazolvan is the need for breathing exercises and the so-called active “coughing”, which are elements of kinesiotherapy. With the combined use of Lazolvan and kinesitherapy, the mucolytic effect occurs faster, sputum becomes less viscous and is more effectively removed from the respiratory tract, thereby reducing the duration of the disease [6]. The duration of therapy with Lazolvan is selected individually. On average it is 4–5 days. If the clinical picture of the disease shows positive dynamics (cough disappears, the amount of sputum decreases, it becomes less viscous, wheezing in the lungs disappears), then it is advisable to immediately discontinue the drug, because Continuing to take it will stimulate mucus secretion and provoke a cough. For dry paroxysmal cough, which usually accompanies the onset of ARVI, the prescription of Lazolvan is also justified to moisturize the mucous membrane of the respiratory tract. In children with a chronic bronchopulmonary process that develops, for example, against the background of a congenital malformation of the bronchi or a congenital immunodeficiency state, Lazolvan® is used for a long time in courses in age-specific dosages, because in these diseases, mucostasis is constantly present. In cystic fibrosis, when chronic inflammation in the respiratory tract is one of the main manifestations of the disease, in addition to dryness of the mucous membrane of the bronchial tree, there are erosions, as well as a large amount of viscous sputum [1–3]. Another common mistake in the treatment of cough is the simultaneous administration of Lazolvan and centrally acting antitussive drugs that suppress the cough reflex (narcotic and non-narcotic drugs). Under these conditions, on the one hand, active dilution of sputum occurs, and on the other, the cough reflex is eliminated, and removal of sputum from the respiratory tract becomes difficult. Quite quickly, especially in young children, mucostasis begins, which in turn contributes to the development of complications, including pneumonia. The so-called “swamping of the lungs” effect occurs. The drug should be prescribed with caution in patients with impaired motor function of the bronchi (for example, with Sievert-Kartagener syndrome, primary ciliary insufficiency), as well as in patients with copious discharge of viscous sputum, also due to the danger of stagnation of bronchial secretions [6]. There is a special dosage form of Lazolvan for nebulizer therapy, which allows it to be widely used for inhalation both in the hospital and at home, including in young children. It is in this group of children that in a large percentage of cases, infectious diseases of the upper respiratory tract are accompanied by symptoms of broncho-obstructive syndrome, which makes sputum discharge even more difficult. In such situations, it is necessary to combine Lazolvan inhalations with the prescription of bronchodilators, both selective β2-adrenomimetic action and combined ones, combining the action of M-cholinolytics and β2-adrenomimetics (in particular, solutions for inhalation of salbutamol or ipratropium bromide and fenoterol are used) [8]. Thus, Lazolvan® is an effective and safe drug that can be successfully used to treat cough in children of various age groups.
Literature 1. Volkov I.K. Therapeutic effectiveness of Lazolvan (ambroxol) in the treatment of chronic diseases in children // Breast Cancer. 2. Korovina N.A., Zakharova I.N., Zaplatnikov A.L., Ovsyannikova E.M. Cough in children. Antitussive and expectorant drugs in pediatric practice. A manual for doctors. – M.: Posad, 2000. – 53 p. 3. Samsygina G.A. Prolonged cough in children: causes, pathogenesis and principles of therapy // Pediatrics. – 2005. – No. 5. – P. 85–91. 4. Klyuchnikov S.O., Boldyrev V.B., Demin V.F. Broncho-obstructive syndrome in young children. Lectures on pediatrics. T. 2. Pathology of newborns and young children. – M.: RGMU, 2002 – pp. 318–329. 5. Vidal reference book. Medicines in Russia. – M.: Astra-PharmServis, 2003 – S. B 517–518. 6. Simonova O.I. Clinical effects of ambroxol hydrochloride (lazolvan): what does the effectiveness of the drug depend on? // Pediatrics. – 2011. – T. 90, No. 5. –P. 128–133. 7. Weissman K., Niemeyer K. Arzneim. Forsch. //Drug. Res. 1978. Vol. 28(1). Heft 1. P. 5a. 8. Zaitseva O.V. Rational choice of mucolytic therapy in the treatment of respiratory diseases in children // RMZh.. 2009. No. 19. P. 1217–1222. 9. Fraschini F. et al. Effects of a Mucolytic Agent on the Biovailability of Antibiotics in Patients with Chronic Respiratory Diseases. Curr Ther Res. 1988; 43: 734–42.
Expectorants for dry coughs: what are they?
It is difficult for a child who is not yet one year old to cope with the disease on his own. Weak respiratory muscles of the bronchi cannot always push out mucus. Therefore, parents need to understand how to make the spasm productive. A remedy for dry cough is prescribed only if there is no discharge.
Expectorants for children under 5 years of age are presented in the form of syrups. Any baby drinks them easily. Effective medications are often combined with procedures - inhalations, herbal decoctions and rubbing. If the child is already 7 years old, then therapy is carried out with tablets. These can be cheap drugs or more expensive ones, it all depends on the financial capabilities of the parents.
Expectorants for children under 5 years of age are presented in the form of syrups. Any baby drinks them easily. Effective medications are often combined with procedures - inhalations, herbal decoctions and rubbing. If the child is already 7 years old, then therapy is carried out with tablets. These can be cheap drugs or more expensive ones, it all depends on the financial capabilities of the parents.
The use of expectorant drugs for children: features
To choose a good expectorant for children, it is necessary to take into account the individual characteristics of small patients.
Of course, it is better to consult a doctor and find out what exactly is right for your child. But not all parents do exactly this. Many fathers and mothers prefer to follow the advice of experienced acquaintances, the older generation and rely on the knowledge of the pharmacist.
When purchasing medicine for a child, you should consider the following rules:
- the drug must be in liquid form, tablets are prescribed to children aged 6 years or more;
- the composition should not contain substances that can cause allergies in the baby;
- the medication must be on the list of over-the-counter drugs;
- natural does not mean safe, many herbal compounds cause allergies;
- expensive - not necessarily effective.
Doctors have differing opinions regarding the use of mucolytic agents. Modern pediatricians believe that it is absolutely forbidden to give them to children under 2 years of age.
Such drugs pose a greater risk of side effects than the expected benefits. In babies of the first year of life, the cough reflex is not yet sufficiently adjusted, so the use of drugs that increase the volume of sputum can be dangerous.
How to choose medications for a baby
Expectorants for wet coughs come in a variety. Most often, the pediatrician prescribes the following drugs that remove mucus from the respiratory tract:
- Marshmallow is a cough syrup for children based on a natural extract. These are expectorant drugs, they reduce spasms and relieve inflammation. If the baby is one year old, the drug is given strictly according to the instructions. Cough remedies for children made from natural ingredients may cause an allergic reaction. In this case, the one-year-old child needs to be shown to a pediatrician and the treatment must be changed abruptly. Side effects of Althea also include nausea and vomiting.
- Licorice root is an expectorant that can be easily found in pharmacies. Decoctions of this remedy quickly remove phlegm, thinning the mucus. Such antitussive drugs should be given carefully to children. If there is no regular intake of fluid into the body, then mucus will accumulate in the lungs, this is a sure path to pneumonia.
- Pertussin is an effective cough suppressant that was used during the Soviet Union. This is an inexpensive medicine available to any family. The syrup promotes expectoration and calms attacks. This is a good remedy; it is included in many modern medicines, the price of which is above 300 rubles per bottle. But even such effective syrups have contraindications - allergies, rashes and nausea.
- Gedelix is an expectorant that thins mucus. For children under one year of age, it is actively prescribed in many clinics across the country. This is an effective expectorant based on plant extracts. Contraindications include diarrhea and allergies.
- Stoptussin-Fito – improves expectoration and relieves inflammation. This cough suppressant is made from plants. Therefore, it is possible that a rash may appear (an allergic reaction to the ingredients).
On this topic:
Effective ways for a child to cough up phlegm
In rare cases, expectorant syrups can cause swelling. In this case, you need to immediately call an ambulance. The doctor will need to tell you which cough expectorant caused this reaction.
Instructions for use of children's antitussive tablets
Tablets are a medicine and therefore must be prescribed by a pediatrician and used in accordance with the instructions.
There are different types of cough: dry, wet, gurgling, barking, hacking. As a rule, different types of cough are caused by different reasons, so different medications need to be selected. For example, there are special tablets for dry coughs for children and special ones for wet coughs. The tablets are packaged in glass vials or blisters, which are placed in cardboard boxes. Instructions for use are always located inside the paper packaging. Parents or caregivers should read it carefully and follow the instructions. This condition does not eliminate the need to coordinate the pill regimen with the treating pediatrician.
How do dry cough medications work?
A dry cough differs from a wet cough by its characteristic sound and the absence of mucus. It occurs at the level of the larynx and, as a rule, does not descend deeply. The symptom is accompanied by soreness and soreness, caused by irritation of the mucous membrane of the larynx. These unpleasant sensations provoke cough attacks, because the inflamed mucous membrane sends impulses along the nerve cells to the cough center located in the brain, in response it generates cough impulses.
Attacks of such cough often follow without interruption, which aggravates the course of the disease. Complications include breathing problems. The sound of a cough is dry, hacking, crackling, often similar to barking. Seizures disturb the child at any time of the day, which greatly exhausts him and does not allow him to regain strength even during sleep.
The cause of swelling and irritation of the larynx is the proliferation of viruses or bacteria on the surface of its mucous membrane. The appearance of a dry cough is characteristic of the first days of a cold (laryngitis, tracheitis, laryngotracheitis, bronchitis) and as a residual phenomenon of the disease.
In light of the above, antitussive drugs are used for the following purposes:
- blocking the cough center;
- effects on peripheral receptors, through which sensitive impulses from irritated mucous membranes are transmitted to the central nervous system (CNS);
Can children use cough suppressants?
Modern cough blockers are highly selective and act only on the cough center without depressing breathing. This quality distinguishes them from previous generation blockers based on narcotic substances, such as codeine, dionine or morphine. They do not form an addictive effect and dependence, do not inhibit gastrointestinal motility, causing constipation. Therefore, the answer to the question “can cough tablets that act as blockers at the central level be given to children” is more likely positive than negative. If the cough is not accompanied by the formation of sputum in the bronchi and lungs, then the blockers will not cause congestion in these organs.
For children, antitussives are prescribed in the form of syrups; the tablet form is suitable for school-age children.
What medications are allowed?
Tablets approved for children that affect the cough center include products containing butamirate citrate. These include tablets such as:
- Panatus (KRKA) - prescribed from 6 years of age daily, 20 mg tablet 2 times;
- Panatus forte (KRKA) - from 12 years old, 50 mg tablet daily 1 to 2 times;
- Omnitus (Serbia, Hemofarm) - children are prescribed a tablet form of 20 mg twice a day per tablet from 6 to 12 years and three times from 12 years.
More often, children are prescribed syrup and drops of Codelac Neo, Omnitus, Sinekod, Panatus.
Butamirate citrate is also part of a complex drug such as Stoptussin, in which it is combined with the substance guaifenesin, which thins mucus in the bronchi. For children over 12 years of age, it is prescribed to be swallowed after meals in a dose calculated by weight (up to 50 kg, half a tablet four times a day).
Important! Exceeding the dosage of cough blocker tablets may be accompanied by vomiting, nausea, stool upset, abdominal pain, dizziness, and loss of coordination. If these symptoms appear, you should take activated charcoal or rinse your stomach
Children's peripheral cough tablets are marketed under the trade name Libexin and contain prenoxdiazine. The substance relieves irritation of peripheral receptors due to a local analgesic effect, and also has a bronchodilator effect. The tablets slightly suppress respiratory class=”aligncenter” width=”800″ height=”600″|fcw3qayjh5a| src=”https://tbdoc.ru/wp-content/uploads/8/f/7/8f7adb89d13d15d00bedde8b0d4d385b.jpg” class=”aligncenter” width=”660″ height=”479″|fcw3qayjh5a| src=»https://tbdoc.ru/wp-content/uploads/f/7/6/f762bb219ed2a2130a9798bf5f6ed34a.jpg» class=»aligncenter» width=»600″ height=»359″|fcw3qayjh5a| src=”https://tbdoc.ru/wp-content/uploads/b/7/c/b7cc73b2316f9c99701bb5937221d933.jpeg” class=”aligncenter” width=”600″ height=”450″|fcw3qayjh5a| src=»https://tbdoc.ru/wp-content/uploads/9/e/e/9eeb14456393b027baae056f5fb1257e.jpg» class=»aligncenter» width=»600″ height=»800″|fcw3qayjh5a| src=»https://tbdoc.ru/wp-content/uploads/7/b/b/7bbd46867c851f4312f4d68bdecf7301.jpg» class=»aligncenter» width=»1708″ height=»712″|fcw3qayjh5a| src=”https://tbdoc.ru/wp-content/uploads/1/c/8/1c8dbfdc8c4a86d7fef878dae88daab1.jpeg” class=”aligncenter” width=”600″ height=”800″|fcw3qayjh5a| src=”https://tbdoc.ru/wp-content/uploads/3/c/2/3c265accae10048b34b1fdf4d8df3f8d.jpeg” class=”aligncenter” width=”600″ height=”800″|fcw3qayjh5a| src=”https://tbdoc.ru/wp-content/uploads/0/9/d/09d9322d8e91d83e76bd0c1b8f78433c.jpg” class=”aligncenter” width=”1024″ height=”768″|fcw3qayjh5a| src=»https://tbdoc.ru/wp-content/uploads/f/f/3/ff34855293009d96a3386dd7a1a25b0c.jpg» class=»aligncenter» width=»938″ height=»612″[/img]
Prescribed to children with caution. Age restrictions are not indicated in the instructions for the drug (Hungary, JSC "Hinoin")
The dose for a child depends on age and weight, is 1/4-1/2 tablets of 100 mg three times/four times a day.
Doctors' warnings
For coughs, a more extensive list of medications is offered for children over 1 year of age. Folk remedies are also acceptable for bronchospasms, but it should be understood that young patients are sensitive to products such as honey, raspberries and other allergens.
Until the age of two, the baby’s respiratory system is not fully developed. Any sputum expectorant in the wrong dosage can worsen the condition. This must be taken into account and never experiment with medications from the pharmacy. Cough medicine for children who are 0-24 months old is prescribed only by a pediatrician.
It is important to know that in 2010, health care in France and Italy banned cough expectorants from being prescribed to patients under two years of age. This is due to the fact that the respiratory system does not remove mucus to a large extent, but distributes it throughout the body. In this case, a common cold develops into a dangerous disease.
It is important to know that in 2010, health care in France and Italy banned cough expectorants from being prescribed to patients under two years of age. This is due to the fact that the respiratory system does not remove mucus to a large extent, but distributes it throughout the body. In this case, a common cold develops into a dangerous disease.
In this case, children need to be given more drinks for cough. These can be decoctions of chamomile and other medicinal herbs. The best remedy is walking in the fresh air, regular ventilation of the room and wet cleaning.
Recommendations and precautions
Any expectorants for children over 2 years of age or younger children should be given with plenty of liquid. The more the child drinks, the more effective the medicine will be.
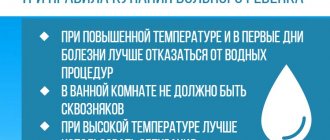
A coughing baby needs to be provided with optimal living conditions, which will also bring the moment of recovery closer. Moist cool air, regular ventilation of the room, loose, breathable underwear and walks (in the absence of elevated temperature) are what doctors recommend.
Expectorant drugs must be given in an age-specific dosage and not deviate from the instructions, unless otherwise indicated by the doctor. Children should not be offered medications at bedtime as most medications act immediately. As a result, the child will not be able to rest due to coughing.
Often moms and dads expect medications to eliminate the symptom right away. However, treatment with expectorants does not imply cough suppression. On the contrary, it becomes more moist, productive and lighter. Parents should understand this when using these medications.
Treatment of cough with expectorants (part 2)
List of products for children over 2 years old
Cough medicine for children over 1 should also be used after seeing a doctor. At this age, the drugs listed above also help. A folk remedy for cough using honey and chamomile decoction will also be effective. These ingredients are simply mixed and given to your baby as a daily drink.
On this topic:
How to treat a persistent cough in a child
There are other antitussives that can be used by children over one year of age:
- Mucaltin are tablets that are best prescribed by doctor's prescription.
- Dry cough syrup for children over 2 years of age – the powder is diluted with warm water according to the instructions. The product must be used after meals, after 15-20 minutes. The dosage is also prescribed in the instructions.
- Linkas syrup is the best expectorant, according to many parents. It is made on the basis of natural ingredients - violet, marshmallow and hyssop. This cough remedy for 1-year-old children is well tolerated and has minimal side effects.
- Syrup "Dr. Theiss" is prescribed to thin sputum. Made from plantain leaves.
It is also permissible to use folk remedies. These are various decoctions and mixtures. The best remedy that has come from ancient times is boiled milk with the addition of a spoon of honey. The drink is not suitable for children suffering from allergies to these products.
Children from 3 years of age are recommended to rinse the nasal passages and do inhalations. You should talk about some procedures with your doctor so as not to harm the young body.
The best expectorants for children
Below is a detailed overview of drugs used to treat productive cough in children of different ages.
Medicines based on marshmallow root (from 30 to 130 rubles per package)
Marshmallow root extract contains a large amount of mucus, pectin, starch and tannins, therefore it helps to effectively fight cough due to its mild stimulating effect on the glands of the bronchial tree and bronchioles. Preparations from marshmallow have a pronounced anti-inflammatory effect, reduce pain when coughing and thin out viscous and thick sputum.
The only contraindication for the use of this group of drugs is peptic ulcer of the duodenum and stomach. The use of products in the form of syrup is contraindicated in case of intolerance to fruit sugar (due to the large amount of sucrose in the composition) and diabetes mellitus.
The most popular medicines based on marshmallow root:
- Alteyka syrup (children under 12 years old take 1 teaspoon 4 times a day, for teenagers the dose is doubled);
- “Mukaltin” tablets (take 1 tablet 3 times a day before meals, after dissolving the medicine in water);
- marshmallow syrup (dosage is 1.25-2.5 ml 3-4 times a day).
Before use, the syrup must be mixed with 50-100 ml of boiled water. The duration of treatment with marshmallow preparations is from 10 to 15 days. In exceptional cases, the patient may be prescribed long-term therapy (up to 2 months).
Stoptussin syrup (120-140 rubles)
"Stoptussin" is a natural herbal preparation with anti-inflammatory and expectorant effects. The syrup contains the most effective medicinal herbs and plants that have a pronounced expectorant effect: extracts of plantain, thyme and thyme.
Despite its natural composition, not everyone can use the syrup. Contraindications for treatment with Stoptussin are:
- allergies to medicinal plants and auxiliary components of the syrup;
- pregnancy and breastfeeding;
- epilepsy;
- brain injuries;
- pathologies of the kidneys and liver.
The drug is not prescribed to children under 1 year of age due to the increased risk of intolerance reactions and the possible development of hypersalivation.
The regimen of administration and dosage depends on the age of the child and is as follows:
- from 1 to 5 years – 5 ml 3 times a day;
- from 5 to 10 years – 5-10 ml 3 times a day;
- from 10 to 15 years – 10-15 ml 3 times a day;
- adolescents over 15 years old - 12.5 ml 3-5 times a day.
The medicine should be taken immediately after meals. The maximum duration of therapy is 7 days.
"Fluditek" (450-500 rubles)
Fluditec is a modern expectorant mucolytic drug with proven effectiveness. The main active ingredient is carbocisteine. “Fluditek” is produced in the form of a caramel-colored syrup with the smell of chewing gum (added “tutti-frutti” flavoring), it has a pleasant taste and aroma, so children willingly drink it, and parents do not have problems with treatment.
The syrup causes practically no side effects, is well tolerated and helps to cope with cough in a short time. The standard dosage of syrup for children is 5 ml 3 times a day, but the amount of the drug may vary depending on the age of the child.
The only disadvantage of Fluditek is its price. If necessary, the doctor can select analogs of the syrup with the same active ingredient. These include:
- "Libexin Muco";
- "Fluifort";
- "Carbocysteine";
- "Bronchobos."
Preparations based on carbocisteine should not be taken for cystitis, chronic glomerulonephritis, or peptic ulcers. Pregnant women and children under 2 years of age are also not prescribed products with carbocysteine.
Medicines for wet coughs for children from five years old
Children from 5 years old can boast of better health. But this does not stop parents from thinking about which remedy to choose to overcome a cough. Children from 4-5 years old can be prescribed tablets. While it is difficult to get 3-year-old children to use them, older children can easily eat such drugs.
When coughing up sputum is difficult, you need to choose the following medications:
- Thermopsol - prescribed from 5 years of age, these are tablets. The course of treatment is 5-7 days, as prescribed by the pediatrician. The drug is also suitable for adults.
- Codelac Broncho with thyme - this remedy can be used if the child is over 10 years old. You need to take one pill a day, the course of therapy should not exceed four days. From the age of 5, the drug is prohibited, as severe complications may occur - suffocation, allergies or diarrhea, causing dehydration.
- The herb wild rosemary is a folk remedy that has been known since ancient times. The mixture should be brewed and drunk 3 times every day, there should be about 100 ml in a glass.
- Bronchicum S syrup - it can be drunk by children up to 2 years old, but it is better to start from the age of 3 years. The drug is considered powerful, especially when the recommendations of the treating pediatrician are followed.
- Bromhexine – has a mucolytic property and is an excellent sputum thinner. The drug should be given taking into account the patient's age.
On this topic:
Causes and treatment of cough in a two-year-old child
It is best to start giving tablets and syrups from the age of three. First of all, any sick child needs to be provided with plenty of fluids. Recipes for softening drinks should be in every family where children's health is given special attention. For adults, such decoctions and juices will also be useful.
Treatment of newborns
You should not give expectorant medications to a newborn baby on your own. In the first months of life, babies develop a physiological runny nose that does not require treatment.
Due to the accumulation of mucus in the nasopharynx, the baby may sometimes cough. These symptoms are not a signal to start treatment. If parents are not sure about the health of the baby, then they should show him to the pediatrician.
If necessary, the doctor will prescribe Gedelix herbal syrup. Its main plant is ivy. The syrup has an expectorant, antispasmodic and anti-inflammatory effect. Until 12 months of age, the baby should be given 2.5 ml of suspension once a day. The duration of use of the medicine should be at least a week. After the disappearance of disturbing symptoms, the suspension must be taken for another 2-3 days.
For severe diseases of the lower respiratory system (bronchitis, pneumonia), the doctor prescribes Ambrobene or its analogues (Lazolvan, Halixol). These drugs have an expectorant and mucolytic effect at the same time. During the treatment period, the child is under medical supervision. It is preferable to use medications in inhalation form. During one procedure, 1 ml of solution is administered to the child.
If the use of expectorants for newborns is accompanied by difficult discharge of liquefied sputum, then the accumulated mucus is removed in the hospital using special equipment.
The best drinks for coughing children
Medicines have side effects. Of course, manufacturers prefer to omit this information so as not to cause panic among parents. Moms and dads regularly ask what is the most effective remedy for bronchospasms with mucus. For a common cold, a competent pediatrician will not rush to prescribe medications. He will give the following advice:
- ventilate the room and carry out wet cleaning;
- go for a walk every day if there is no fever;
- make compresses from mustard plasters for children over 4 years old who do not have pathologies or heart disease;
- drink a lot.
The last tip involves more than just using water and tea. It is best to prepare medicinal drinks that will help remove phlegm from the respiratory tract:
- decoctions of rosehip, raspberry or chamomile leaves - these plants have a special effect on the body. Drinks will not only remove mucus, but also strengthen the immune system. They need to be consumed 5-7 times every day;
- tea with lemon is a classic drink that is ideal for preventing colds. With the onset of winter, every kitchen should have this citrus. It can be cut into circles and put in a jar, covered with sugar. Every time you pour tea, you need to take out this delicacy and throw it into the drink or eat it like candy;
- dried fruit compotes - children of any age love them. For a more pleasant taste, you can add a little sugar or a few circles of lemon;
- jelly - starch coats the walls of the throat, facilitating the process of spasms. Children from 7 years old enjoy drinking such drinks. There is a huge selection of flavors on the shelves in the store;
- freshly squeezed juices - it is best to choose citrus fruits, carrots and beets. To prevent vegetables from seeming disgusting, you need to mix them with oranges, apples or other juicy fruits.
The mucus that accumulates in the lungs must come out. Special medications help facilitate this process. If you do not take any measures, you may encounter serious complications. Of course, it is easier to prevent bronchospasms by consuming vitamins, fruits, vegetables and decoctions of medicinal herbs.
How to choose a drug by age
What syrup should I give to a baby with a dry cough, and which one is suitable for older children? Antitussive medications have age restrictions. This should be taken into account when choosing a medicine.
The following is a list of dry cough syrups for children in tabular form by age category.
| Dry cough syrups for children / age category | Drug name |
| Up to 1 year | Lazolvan, licorice root syrup, Bronchicum, Prospan, Herbion ivy, syrups with ambroxol. From 3 months - Bronchipret, from six months - Linkas |
| From 1 year | Alteika, Gelisal |
| From 2 years | Erispolom, ACC, Herbion |
| From 3 years. | Rengalin, Pertussin, Omnitus, Doctor MOM |
List of effective syrups for dry cough for children, available in domestic pharmacy chains:
| Name | Compound | Therapeutic effect | Application | Price |
| BRONCHOLITIN | Glaucine hydrobromide, ephedrine hydrochloride | Antitussive, bronchodilator | 1 teaspoon 3 rubles per day (from 3 years) | From 100 rub. |
| DOCTOR MOM | Elecampane, aloe, ginger, nightshade, cubeba pepper, wasaka, licorice | Bronchodilator, mucolytic, anti-inflammatory, mucokinetic | ½ tsp 3 r. per day (from 3 years). The therapeutic course lasts 14 days | From 175 rub. |
| KODELAK NEO | Butamirate citrate | Expectorant, eliminates unproductive paroxysmal cough, anti-inflammatory | 1 teaspoon 3 rubles per day (from 36 months) | From 139 rub. |
| GERBION primrose syrup | Plant herbs | Expectorant | ½ tsp 3 r. per day for 2-3 weeks (from 24 months) | From 230 rub. |
| SINECODE | Butamirate citrate | Bronchodilator, makes breathing easier | 3 r. per day for 7 days (from 3 years old) | From 260 rub. |
| GEDELIX | ivy leaves | Facilitating expectoration of sputum, anti-inflammatory, wound healing, antioxidant, antibacterial, antimicrobial, antispasmodic, mucolytic | ½ tsp 3 r. per day (up to 12 months). From a year - 1 teaspoon 4 rubles. in a day | From 350 rub. Good dry cough syrup for children |
| PROSPAN | ivy leaves | Mucolytic, expectorant, antimicrobial, antispasmodic, antitussive | 1 teaspoon 3 rubles per day (from 1 year). After consumption, side effects may occur in the form of skin rashes, since many children develop an allergy to ivy | From 400 rub. |
| EUCABALUS | Thyme and plantain, ethanol | Expectorant, mucolytic, anti-inflammatory | 1 tsp 2 r. per day (up to 1 year) | From 200 rub. |
| TUSSAMAG | Thymol and carvacrol | Expectorant, antiseptic | 1 teaspoon 2-3 r. per day (from a year) | From 239 rub. |
| TRAVISIL | Fennel, pepper, licorice, ginger, emblica, turmeric, terminalia | Local irritant, distracting, antiseptic, anti-inflammatory | 1 measuring spoon 3 rubles. per day (from 12 months) | From 96 rub. |
| LINCAS | Extracts of hyssop, marshmallow, violet | Emollient, bactericidal, antibacterial, expectorant, mucolytic | ½ tsp 3 r. per day (from 6 months). Course of therapy – from 7 to 10 days | From 135 rub. |
| BRONCHICUM | Thyme, alcohol | Expectorant, anti-inflammatory | 1 teaspoon 3 rubles per day (from 2 years). Duration of treatment is 2 weeks | From 199 rub. |
| PERTUSSIN | Thyme | Expectorant, mucolytic | 3 r. 1 measuring spoon per day, which comes with the kit (from 3 years old) | From 30 rub. This is the most inexpensive cough syrup for children |
| DOCTOR THEISS | Mint, plantain, beetroot | Improves the removal of mucus from the lungs and upper respiratory tract | ½ tsp 4 rubles per day, washing down the solution with water (from 1 year) | From 270 rub. |
| LAZOLVAN | Ambroxol | Mucolytic, expectorant | 2-3 r. in a day | From 190 rub. |
| Licorice root syrup | Herbal Ingredients | Expectorant, enveloping, antimicrobial, restorative | No more than 2-3 drops three times a day (from 1 year). From 2 years – from 2 to 10 drops three times a day. Before use, dilute the medicine in tbsp. l. boiled water at room temperature | From 50 rub. |
| ASKORIL EXPERTOR | Guaifenesin | Bronchodilator, mucolytic, expectorant | 1 teaspoon 3 rubles per day (up to 6 years) | From 228 rub. |
| AMBROBENE | Ambroxol | Mucolytic, expectorant | ½ teaspoon 2-3 r. per day 7 days (from 1 year). | From 104 rub. |
Medicines depending on the nature of the symptoms
Medicines should be selected depending on the nature of the clinical picture. This applies to cheap and expensive tablets.
Dry cough
This type of cough, caused by exacerbation of chronic pathologies of the respiratory system, is treated with medications that have a local (most preferable) or systemic effect. The first group (Libexin, Prenoxdiazine) prevents bronchospasm, and the second (Bromhexine, Solvin) is prescribed for acute pathologies. If the phenomenon in question does not stop, narcotic drugs are used (Terkodin, Codelac). At the initial stage of development of a cold, mucolytic medications are recommended.
Wet cough
If the patient coughs up mucus, then it is necessary to use:
- Mucolytic tablets - "ACC", "Fluimucil".
- Combined medications that have a mucolytic and expectorant effect - “Ascoril”, “Bromhexine”, “Ambroxol”.
If a sufficient amount of sputum is produced when coughing, expectorant medications are recommended:
- "Dr. MOM." The drug is based on herbal components that suppress the inflammatory process and soften the throat tissue.
- "Mukaltin." The drug is based on marshmallow extract, which stimulates the contractile function of the bronchi and the functioning of the glands.
- "Thermopsis". This Soviet drug enhances sputum secretion due to the combined action of the Tremopsis plant and sodium bicarbonate.
Some expectorant tablets cause unpleasant consequences in the form of intestinal upset.
Allergic reaction
The symptom occurs in the form of a reflex reaction of the body to the action of the pathogen. To relieve allergy symptoms, cadeine-based medications are prescribed:
- "Quintalgin";
- "Codelac";
- "Terkodin";
- "Tedeen."
Local antitussives can be an analogue of these medications. If you have an allergic reaction, you must take an antihistamine.
Treatment methods for bronchitis
For chronic bronchitis, topical antitussive drugs or mucolytic agents are prescribed. In case of exacerbation of the pathology, the latter must be supplemented with expectorants. You should take medications until the disturbing symptom disappears.