Diagnostic techniques
Babies whose whites of the eyes are yellow need to undergo special diagnostics.
Such a symptom can be either completely harmless or serve as a sign of a certain pathology. Diagnostics includes:
- general examination by a specialist;
- blood and urine tests;
- studying information about the course of pregnancy.
Based on the studies conducted, a conclusion is made and the general condition of the baby is assessed. If specialists suspect a hemolytic disease, several special blood tests may be required, which will allow them to track the necessary indicators over time.
Why does jaundice appear?
Here, bilirubin is primarily to blame. What is it and where does it come from? It's quite simple. A child who has not yet been born has special blood with special (fetal) hemoglobin. It carries oxygen through the baby's blood vessels. When a baby is born, he begins to breathe through his lungs. And then the composition of the blood changes: “live” hemoglobin appears in it, and fetal hemoglobin is destroyed. This is where bilirubin is formed. The child does not need it, and the little body begins to get rid of it.
This is a very difficult task for a child. You can't just remove bilirubin. First, it enters the liver and is mixed there with special enzymes, then dissolves in urine and is then easily excreted. If the liver cannot cope and there is a lot of bilirubin in the blood, jaundice will begin.
The causes of pathogenic jaundice are completely different. They are most often caused by a violation of the outflow of bile from the body due to the following conditions:
- blood group incompatibility;
- Rhesus conflict;
- viral liver damage;
- genetic metabolic disorders;
- hereditary diseases;
- hormonal disorders;
- mechanical damage to the biliary tract or liver.
VIDEO:
Norm of bilirubin
In the blood of a newborn baby, bilirubin should be from 8.5 to 20.5 µmol/l (micromoles per liter). The unit of measurement is quite complex, but you don’t have to delve into it. If you're really interested, the blood test takes place at the molecular level. If the results of the analysis show that the bilirubin content is slightly higher than normal, the doctor understands: the baby’s body does not have time to cope with the load. True jaundice occurs when the bilirubin level exceeds 35 µmol/l.
And yet she is different...
Why jaundice appears is already clear. Why do you generally have difficulty removing bilirubin? Could this be a sign of pathology? Unfortunately yes. Doctors distinguish two groups of jaundice – physiological and pathological. Let's look at all types of jaundice from the rarest to the most common.
Diseases of the hepatobiliary system and pancreas
In liver diseases, the binding of bilirubin in hepatocytes (liver cells) is disrupted due to damage and destruction of the latter. As a result, an excess of this pigment accumulates in the blood serum, which is externally manifested by jaundice and icterus of the sclera of the eyes.
The following liver pathologies may be the cause:
- toxic, autoimmune, viral and other types of hepatitis;
- fatty liver hepatosis;
- fibrosis and cirrhosis of the organ;
- malignant liver tumors;
- parasitic lesions of the gland (amebiasis, opisthorchiasis, echinococcosis, alveococcosis);
- liver sarcoidosis.
In liver cirrhosis, the cells of the organ are replaced by fibrous connective tissue, as a result of which the gland loses its functions, including the ability to bind bilirubin, which is clinically manifested as jaundice
. Each of these diseases has its own characteristic clinical manifestations, but all of them can be accompanied by yellowness of the proteins eyes and skin.
Yellowing of the sclera in pathologies of the biliary tract is associated with the accumulation in the blood of bilirubin already bound in the liver due to the impossibility of its movement into the intestines for various reasons, for example, blockage of the bile duct with a stone. As a result, the normal outflow of bile, rich in bilirubin, from the liver to the intestine is disrupted, small intrahepatic bile ducts along with blood vessels are ruptured, and the bile is absorbed back into the blood and causes the development of cholestatic jaundice.
Causes:
- primary sclerosing cholangitis;
- benign or malignant formations of the biliary tract and head of the pancreas;
- opisthorchiasis (infection with a parasite from the group of flatworms);
- cholelithiasis.
Cholestatic jaundice has its own characteristics. The mucous membranes and skin are painted an intense yellow color, close to orange. Intense skin itching appears, due to which scratches appear on the skin. The pain syndrome is intense and localized in the right hypochondrium. The feces become discolored (become gray, like clay), and the urine takes on the characteristic shade of beer.
Cholestatic jaundice requires urgent, usually surgical, care
In diseases of the pancreas (acute pancreatitis, benign and malignant neoplasms), the organ increases in volume, which may be accompanied by compression of the common bile duct and disruption of the outflow of bile. As a result, jaundice and icterus of the sclera occurs according to the same cholestatic mechanism as in pathologies of the biliary tract.
Types of pathology
Yellow pupils in a newborn may be due to exposure to infectious diseases, the development of intrauterine infections, metabolic or endocrine pathology. One of the main causes of yellowing of the skin and mucous membranes is the absence or acquired infection of the biliary tract. With this pathology, bilirubin is not removed from the child’s body at all.
Newborns have the following pathological types of jaundice:
- Conjugative (also called ophthalmic). It appears due to an insufficient amount of enzymes in the liver, as a result of which the bilirubin contained in the cells is poorly bound and processed.
- Hemolytic. Its appearance is provoked by disturbances in the composition of the blood (changes in the structure of red blood cells or hemoglobin).
- Hepatic. Occurs in various liver diseases when liver tissue is affected by bacteria, viruses and toxins. With hepatitis B and C, sepsis, cytomegalovirus, bilirubin accumulates in the blood, causing the skin and mucous membranes to turn green-yellow.
- Mechanical (obstructive). It may occur due to disturbances in the natural outflow of bile. The main cause of the pathology is a decrease in the patency of the bile ducts.
Prevention of yellowness of proteins
Any preventive measures can reduce the risk of morbidity. Taking care of your eyesight is also necessary. To prevent the development of diseases, you need:
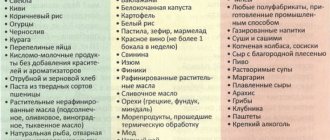
- Proper, and most importantly, balanced nutrition. A person should consume large quantities of vegetables, fruits and protein foods. It is worth giving up smoked, fried, salted, flour and alcohol.
- Long walks, preferably outside the city.
- Full sleep. An adult should rest at least 8 hours a day. If the patient has low blood pressure, then he should devote 9 to 10 hours to sleep.
- If your working day is spent in front of a computer monitor, you should take short breaks.
- It is recommended to take vitamin complexes.
- If the color of the proteins has changed as a result of overwork, then you should use drops and lotions to eliminate the symptoms.
Classification features
Pediatricians distinguish two main types of yellow proteins in a baby: physiological and pathological etiology. The first refers to normative conditions, but it is also monitored by the attending physician. Physiological jaundice has an additional division.
Milk type
Milk or pregnane type - determined by increased levels of estrogen contained in breast milk. Some of its components can interfere with the metabolism of bilirubin, which contributes to disturbances in its synthesis and problems with normal excretion from the body. The result of the anomaly is a yellowish tint of the skin and white membranes of the eyes.
This option appears one to one and a half weeks after birth; in some cases, symptomatic manifestations may occur at a later date. When the child’s body is weakened, milk jaundice forms on the third day of the baby’s life.
When breastfeeding stops, the bilirubin level returns to normal values. This condition is called hyperbilirubinemia. The disease does not require specialized treatment, and clinical signs disappear spontaneously within one to two months.
Continuation of breastfeeding or complete transfer of the baby to artificial nutrition depends on the indicators and general condition of the body. The pediatrician is based on the benefits for the baby, and not on common misconceptions that natural feeding should be continued in any case. The priority is the baby's health.
Neonatal type
Neonatal type - occurs when the child’s body is unable to process both the residual erythrocyte cells of the mother and her own. The deviation provokes a gradual accumulation of bilirubin and yellowing of the sclera of the eyes and dermis of the newborn.
A yellowish tint affects the head area and gradually decreases along the body, moving to the lower limbs. In most cases, jaundice does not progress beyond the umbilical ring. Average neonatal data report:
- In 90% of children, the problem does not require treatment and goes away on its own;
- In 10% of newborns, the anomaly develops into a pathological process.
In the absence of symptoms of a developing disease and the baby’s normal state of health, the color of the skin returns to standard values after a week, the last to normalize the color of the protein membranes of the organs of vision and the skin of the face.
Parents should be concerned about the following signs:
- Pallor of the dermis or the appearance of a strange greenish tone;
- Discoloration of stool;
- Dark color of urine, reminiscent of beer;
- Restless behavior of the child;
- Sudden bouts of crying without external stimuli;
- Apathetic state;
- Refusal to eat.
These features indicate the transition of the neonatal form to the pathological one and require professional help.
Pathological type
Pathological type - the syndrome can be registered both from the moment of birth and after a calendar month of the baby’s life. Like the harmless form of jaundice, it is associated with increased concentrations of bilirubin in the bloodstream. The pathology is characterized by maximum rates and a long course of the disease.
Symptomatic manifestations are more pronounced; in addition to yellow proteins and skin, internal systems and organs are involved in the process, which can pose a threat to the life and health of the newborn.
Experts identify several variations in the pathological type of infant jaundice.
Conjugation – formed with insufficient liver development. The problem of yellow eyes is registered in babies within 2-10 days after birth. The pathological deviation does not affect the color parameters of urine and feces.
Definition of symptoms
Most newborns experience neonatal jaundice, a symptom of which is not only yellowing of the skin, but also the eyes. It is not dangerous to the child’s health and goes away in a few days. In some cases, yellow whites of the eyes in a newborn are a sign of pathological diseases.
Symptoms that indicate something is wrong with your baby:
- The baby was born with yellowed skin, or it acquired such a shade in the first days after birth;
- Symptoms intensify on the 3-4th day of life;
- The yellowness of the skin does not go away, even when the baby is 1 month old;
- Symptoms of the disease periodically appear and disappear;
- The child may have white stools and dark urine;
- The baby completely or partially refuses to eat;
- The baby's regurgitation became more frequent or vomiting appeared;
- Unexplained bruises and bruises appeared on the baby’s body;
- When palpating the abdominal cavity, you may notice an enlarged liver or spleen;
- A yellow rash appeared on the child's face and body;
- The newborn looks lethargic and drowsy;
- The baby has an increase in temperature.
The child has yellow pimples on his face
in humans: reasons
Many people, having noticed such changes, do not rush to seek help from highly qualified specialists. After all, most people believe that yellow squirrels are not a cause for concern. In addition, such changes do not cause a feeling of discomfort. A person in this condition may feel good. However, disturbances in the body still occur. Even a spot on the whites may indicate the development of a certain disease.
Yellow eyes in humans are a sign of a serious illness. Typically, this symptom occurs when:
- Liver diseases.
- Various infections.
- Viral hepatitis.
- Conjunctivitis.
- Problems associated with the bile ducts.
- Neoplasms of both benign and malignant types.
Possible complications
Advanced jaundice can subsequently cause the following disorders:
- Neurological abnormalities;
- Malfunction of the brain;
- Poisoning of internal organs with toxins;
- Partial or complete hearing loss;
- The eyes begin to fester;
- Various degrees of paralysis;
- Development of liver cirrhosis;
- Seriously weakened immune system.
If the whites of the baby's eyes turn yellow, this means that there are some disturbances in the functioning of his body. This symptom is temporary and does not pose a threat to health. There are certain cases when changes in eye and skin color are caused by serious pathologies that are life-threatening and require immediate treatment.
Parents must take into account all the doctor’s recommendations, follow the instructions and provide the child with careful care. If these conditions are met, they can be confident of a favorable outcome.
Ophthalmic diseases characterized by yellowing of the sclera
Yellowing of the sclera may occur due to eye lesions. For example, malignant conjunctivitis, various neoplasms, mechanical eye injuries, and contusions may be to blame.
Diseases that cause the whites in the eyes to turn yellow:
- Melanoma is a malignant tumor, mainly localized in the limbus area, and also affecting the bulbar conjunctiva. Its color is dark. As a result, the development of the disease can gradually lead to the onset of a pronounced vascular reaction. Having discovered such a disease, the doctor most often refers the patient to enucleate the eye, and a decision may be made to remove it.
- Wen, or pingvecula. This is a benign formation that has a yellow tint and is located on the conjunctiva of the sclera. Usually occurs in elderly patients. It can form due to problems with lipid metabolism, as well as under the influence of various provoking circumstances. As the tumor develops, a complication may appear, which is the so-called “dry eye syndrome.”
- Pterygium. Significant growth of the conjunctiva is common for this disease. In some cases, pterygium can occur due to drafts, ultraviolet radiation, and chronic conjunctivitis. The course of the disease is generally favorable. But in complicated situations, when the pterygium begins to creep onto the optical part of the cornea, vision can noticeably deteriorate. In this case, immediate medical attention may be required.
- Subconjunctival hemorrhages. The reason for their appearance is the use of anticoagulants, frequent lifting of unbearable weights, and very physically demanding activities. Also, provoking factors can be laughter, coughing or vomiting, operations performed, and infectious diseases. Such hemorrhages can resolve after a few weeks with almost no residue. But the sclera remains yellow-gray for the next three to four months.
Treatment
In the event that a mild form is observed and the child has “safe” jaundice, medical intervention is not required
You just need to provide your baby with maximum support and attention.
In the case of a pathological disease, a treatment process is necessary, and the mother and child are admitted to the hospital until complete recovery. In a hospital setting, as a rule, different groups of therapeutic treatment are prescribed, this is determined by the main causes of the disease.
Drug therapy
Among the side effects, no pronounced ones were found; they were mostly transient and mild in nature.
Consider a few specific points:
When the cause of the disease is incompatibility or conflict between the blood of mother and child, a blood transfusion is usually used. It can be prescribed more than once, since the main goal is to replace old blood with new one. Already at the first transfusion, replacement can be up to 70 percent of the amount that is in the child’s body. This process is complex and requires additional measures, taking antibiotics or physiotherapy. In the case of mechanical jaundice, surgical intervention is required. Here, all responsibility falls on the shoulders of the medical commission that examined the child and made such a difficult decision. A course of physical therapy, with a total duration of up to 96 hours, is also often prescribed for vitamin D deficiency
A special lamp in its action, reminiscent of the sun, activates the production of an important vitamin, and it in due time helps to remove bilirubin. The child is blindfolded and placed for “tanning” in a special room. For severe illness, glucose and activated charcoal may be prescribed.
Glucose stimulates the liver to work actively, and charcoal absorbs toxins, including bilirubin, and they are excreted along with the feces.
Folk remedies
Among the folk methods there are also many that deserve attention, but you need to understand that all of them should be used only in conjunction with medicinal methods. You should not take homemade remedies without your doctor's permission.
- Rowan or fresh juice from its berries, no more than 100 g at a time.
- One teaspoon of rosehip syrup or a drink made from the berries of this plant.
- 30 drops of barberry tincture.
- Beetroot juice no more than 100 g.
- A teaspoon of aloe juice.
Among the infusions, wormwood with honey or St. John's wort infusion are very effective. It is better to use a thermos for infusion.
Jaundice in newborns
Yellow whites of the eyes are observed in almost every newborn soon after birth. This is due to the insufficient maturity of the baby’s liver enzyme systems. In a newborn, the yellow whites of the eyes go away on their own, without medical intervention.
Physiological jaundice in a newborn is not a pathology. This is the baby’s body’s reaction to adapt to environmental conditions. Appears in every second newborn.
During the prenatal period, the child's body receives a large number of red blood cells from the mother. When born, the formed elements of the blood disintegrate massively, resulting in the release of bilirubin.
The liver enzymes of a newborn are not able to bind bilirubin with proteins in order to remove it from the body due to their immaturity. The baby's sterile intestines are also not a contributing factor for the excretion of pigment in feces.
Physiological jaundice disappears during the first 10 days of life. If yellowing of the skin and whites of the eyes persists for a longer period, the baby should be taken to a pediatrician to assess the condition and prescribe therapy.
However, there is a second reason for yellowing of the skin and mucous membranes in a baby - hemolytic disease of newborns. It develops in the event of an immunological conflict due to incompatibility of the Rh factor or blood group. This is a very serious condition that threatens the child’s life and requires emergency care.
Hemorrhages due to rupture of a vessel and spot
If your newborn's eyes are red, your baby probably has subconjunctival hemorrhage. Typically, hemorrhage in the eye of a newborn occurs as a result of minor trauma to the child's eye during childbirth. Hemorrhage is red-blue or red-black, red spots on the eyes of a newborn, it is caused by a rupture of a vessel under the thin membrane covering the eyeball. After a few days, the spot on a newborn's eye usually goes away, as do any bruises.
But if the whites of your baby's eyes remain red and irritated, he may have allergies or conjunctivitis, a contagious eye infection. The affected eye or eyes stick together in the morning, and a crust forms on the eyelashes. Even if conjunctivitis appears in one eye, most likely it will spread to the other. The disease must be treated as soon as possible.
Yellow eyes are a sign of jaundice
Yes, yellow eyes in a newborn can be a telltale sign of jaundice, which is common in babies. More than half of babies are born with physiological jaundice, which causes their skin to appear yellow.
Typically, yellow whites of the eyes in newborns are a temporary condition, do not have serious consequences and are in no way associated with diseases of the liver or other organs. Jaundice develops due to an increase in the amount of bilirubin, a yellow-orange substance produced when red blood cells (red blood cells) break down. Because a newborn baby's liver is not yet able to remove bilirubin quickly enough, many children's eyes and skin turn yellow. In most cases, newborn jaundice goes away on its own within the first week of life.
But if the yellowness of the whites of the eyes and skin in newborns does not go away within a week after birth, it is likely that the baby has developed breast milk jaundice, a generally harmless condition in which certain components of the mother's milk mix with the breakdown products of bilirubin. This jaundice can last up to six weeks or more and is usually hereditary. Although in most cases there is nothing to worry about. A baby with jaundice from breast milk should be examined by a doctor and his bilirubin level should be measured.
Sometimes babies develop jaundice from insufficient feeding (it should not be confused with harmless jaundice from breast milk). With jaundice from insufficient feeding, a significant excess of bilirubin levels can cause liver destruction and other serious consequences. The most common treatments are phototherapy (light therapy) and more frequent breastfeeding. In particularly difficult cases, additional nutrition with a special formula is prescribed.
In some babies, jaundice is a sign of infection or pathology of the thyroid gland - in both cases, treatment is necessary. Jaundice occurs when the Rh factor does not match, a potentially dangerous condition for both the mother and the infant. In most cases, hospitals take preventive measures before and after birth to eliminate Rhesus conflict. Without proper treatment, babies born with hemolytic disease of the newborn can suffer from numerous complications, leading to various forms of anemia and jaundice, destruction of brain cells and heart failure.
Regardless of the cause of jaundice, if your baby's eyes and skin remain yellow for several weeks after birth, your baby's bilirubin level should be measured. With increased levels of bilirubin in the body, urgent measures are required to prevent serious liver diseases, deafness, cerebral palsy and brain damage. Treatment includes phototherapy, but in rare cases a blood transfusion may be needed.
Pupils of different sizes - anisocoria
Pupils of different sizes - anisocoria - is most often a painless, harmless phenomenon that is inherited. One in five people has one pupil larger than the other, and most of these people were born that way.
If your baby was born with different-sized pupils, there is nothing to worry about, especially if you haven't noticed any other unusual signs. Anisocoria can develop some time after birth, but in this case it may be the result of injury or infection, so the child must be seen by a doctor to rule out serious illnesses.
Pupils of unequal size combined with different colored irises and/or drooping eyelids may be signs of congenital Horner's syndrome, which is generally not dangerous to health. But Horner syndrome affects people of any age; it is preceded by injuries to the neck, eyes, and facial nerves; spinal cord or brain.
If anisocoria occurs unexpectedly, it may be a sign of the development of a dangerous disease - for example, cerebral hemorrhage, aneurysm, brain tumor, meningitis or encephalitis.
Causes of yellow whites of the eyes
The main causes of yellow sclera of the eyes:
- Diseases of the liver and biliary tract - the whites of the eyes are colored with a yellow pigment, which is formed due to the breakdown of a large number of red blood cells. This pigment is bilirubin, which for some reason (hepatitis, cholelithiasis) is not excreted from the body;
- Helminth infections - parasitism of helminths (opisthorchis, echinococcus) in the liver can cause closure of the lumen of the bile ducts, which provokes obstructive jaundice;
- Physiological jaundice of a newborn - after birth, the baby’s red blood cells actively disintegrate, and liver enzymes are not yet mature enough to cope with the resulting bilirubin;
- Melanomas and conjunctivitis of a malignant nature are pathologies of the visual analyzer;
- Bad habits, including alcohol abuse, smoking, consumption of large amounts of spices, fatty, smoked foods;
- Overstrain and fatigue.
Overvoltage
Prolonged stress on the visual analyzer can be a provoking factor for yellowing of the sclera. Occurs in the following cases:
- Prolonged work on a personal computer;
- Chronic lack of sleep;
- Long reading in a supine position;
- Working with small details in low light.
In such situations, yellowness of the eyes is accompanied by pain, a feeling of dryness and pain, and “the presence of sand.” A person cannot concentrate his gaze on a specific object and complains of headaches and dizziness.
Bad habits
Tobacco smoking is perhaps one of the most harmless reasons why the whites of the eyes may turn yellow.
As you know, tobacco smoke contains a large amount of toxic substances. When in contact with the eye, smoke has a harmful effect on the tear film and conjunctiva, as a result of which they can become cloudy or even yellow. However, it must be said that this does not happen to every smoker.
Infectious eye diseases
The whites of the eyes may turn yellow if a person has recently had infectious keratitis or severe conjunctivitis. The fact is that during the course of the disease, microscopic defects appear on the surface of the conjunctiva and cornea, after healing of which yellowish scars remain.
It should be noted that this phenomenon can remain for life or disappear without a trace when using keratoprotectors - drugs that accelerate the regeneration (restoration) of the cornea.
Liver diseases
Sometimes yellowed whites of the eyes are the first symptom of hepatitis and other liver diseases.
The coloring of proteins is caused by the breakdown products of bilirubin, an enzyme that is produced by the liver for the normal functioning of the hepatic system. In this case, the skin and visible mucous membranes will turn yellow.
A similar picture will be observed in all viral hepatitis, Gilbert's syndrome (hereditary increase in the concentration of bilirubin in the blood), malignant neoplasms of the liver
Diseases of the biliary tract
Prevention of myopiaWarming up for the eyes when working at the computerTreatment of dry eye syndrome
As a result, bile accumulates in the cavity of the gallbladder, and its breakdown products penetrate into the blood and give the skin and mucous membranes a specific yellow-lemon coloration.
Parasitic diseases
This refers to opisthorchiasis and echinococcosis.
The favorite location of these parasites is the liver. Together with the blood flow, the parasite larvae penetrate the hepatic ducts. Once there, they tightly attach to the wall of the ducts and form cysts in which further development of the parasite occurs.
Over time, the cyst grows, compresses the hepatic ducts and causes an attack of hepatic colic, one of the symptoms of which is yellowing of the sclera (the whites of the eyes).
Now you know why the whites of the eyes turn yellow in adults, but why does scleral jaundice occur in children?
Types of vascular defects and symptoms
Skin problems of this kind on the baby’s thighs are visually noticeable. Defects are reddish or bluish in color. In rare cases, a harbinger of their occurrence is:
- dry skin;
- muscle weakness;
- burning;
- aching pain when pressing on the damaged area.
When the defect is already noticeable, the baby may complain of pain or heaviness in the limbs, spasms and cramps, and headaches.
Spider veins can have different sizes and be tree-like, linear or spider-like in shape. They form where the capillaries on the thighs expand and burst. In the latter case, they may resemble bluish spots with branches, similar in appearance to small blots. Sometimes defects appear in areas of expansion of a vein or artery, where such vessels are located near the skin.
Diagnostics
Diagnosis is quite difficult, since there are a large number of factors that can cause such causes. Initially, the doctor conducts a visual examination of the patient and studies the medical history. By palpation you can determine that the liver is enlarged. In order to determine the presence of pathological changes, laboratory tests and ultrasound diagnostics are prescribed.
If there is fever, tachycardia and signs of intoxication, hospitalization will be required. The examination continues at the hospital. In addition to changes in the color of the sclera, the shade of the skin and urine may change. A general analysis of blood, urine and feces is required.
Bacteriological and biochemical studies are also carried out. Additionally, the following diagnostics are carried out:
- MRI;
- CT;
- Ultrasound;
- X-ray;
- cardiogram.
Diagnosis depends on suspicion of the presence of a specific disease
It is important to take into account the indicators of red blood cells and bilirubin in the blood. Hemoglobin levels are also monitored
Taking into account the results of the examinations, the doctor can determine the diagnosis and prescribe treatment.