Allergic dermatitis in children occurs as a result of exposure to allergens on the skin. Inflammatory processes appear with frequent and prolonged contact with irritating substances - synthetic materials, hygienic cosmetics, plants, etc. The manifestation of an allergic reaction indicates an increase in the body’s sensitivity (sensitization) to allergens. The disease is indicated by papules, swelling, redness, and peeling of the skin in areas that have been in contact with irritating substances.
What is allergic dermatitis
Skin rashes are the body's reaction to a specific irritant (allergen) called allergic dermatitis. The pathology is complicated by a hereditary predisposition to allergies. The mechanism of disease development is based on the penetration of the irritant into the surface layer of the skin (epidermis).
The body produces immune antibodies to the action of the allergen. They form increased sensitivity to this stimulus. The next time you come into contact with it, itchy rashes appear.
The child scratches them, the skin turns red and swells, which leads to inflammation and the development of complications.
Differences between allergic and atopic dermatitis
Without treatment, the allergic form of the pathology transforms into atopic dermatitis in children, which is chronic and difficult to treat. The diseases have a common nature, but differ in the following characteristics:
- The appearance of atopic dermatitis is not always associated with allergens.
- The cause of allergic dermatitis is constant contact with an irritant, while atopic dermatitis is a genetic predisposition.
- Different localization of rashes in infancy with allergic dermatitis.
Clinical manifestations
The main symptoms of allergic dermatitis in children are quite characteristic. They allow the doctor to make the correct diagnosis even without additional diagnostics, based only on a general examination and anamnesis (description of the conditions that preceded the development of the disease). The main clinical manifestations of allergic dermatitis in children are:
- Skin rashes. More often they have a round shape and initially look like slightly swollen and hyperemic areas of the skin. Subsequently, bubbles appear at this place, which, when opened, leave behind weeping erosion.
- Itching in the affected area.
- Increased skin temperature in the area of development of the pathological process.
Lesions in allergic (atopic) dermatitis have a characteristic localization
The severity and impact of these symptoms on the general condition of the child depend on his age. The older the baby, the milder the disease progresses.
Note. Pediatricians, allergists and dermatologists know the symptoms and treatment of allergic dermatitis in children. At the same time, allergists are specialists in the fight against this disease. It is best to contact them when the first symptoms of such a disease develop.
Stages of the disease
Allergic dermatitis in a child occurs in several stages. Stages of the disease:
- Initial – characteristic primary signs of pathology develop within 2-3 days. With timely treatment, the disease recedes; if therapy is not prescribed, it enters the second stage.
- Pronounced – reduction of toxic substances in the body. After 2-3 weeks, the period of exacerbation subsides and is replaced by a chronic form.
- Remission - the child’s condition improves, the skin is cleansed. The duration of the stage depends on the baby’s immunity and the treatment received.
- Stage of clinical recovery - symptoms of dermatitis disappear for an indefinite period.
Mechanism of inflammation development
Allergic dermatitis is a group of diseases accompanied by inflammation of the skin caused by allergic reactions to irritants. Many parents confuse the disease with prickly heat, diathesis and ordinary irritation. In fact, allergic dermatitis in a child has serious differences from these diseases and requires timely treatment.
Insufficient functions of the digestive system, abnormal liver function and immaturity of the immune system are the main causes of the disease. Immediately after birth, the child’s body is attacked by a large number of allergens. The immune system recognizes them as foreign agents and begins to produce antigens to the irritants. When irritating substances re-enter the body, allergic reactions occur.
Very often the disease develops in children who are breastfed. Inappropriate immune responses provoke inflammation, redness and swelling of the skin. Factors that increase the risk of developing the disease include:
- gastritis;
- enterocolitis;
- gastrointestinal diseases;
- helminthic infestations;
- dysbacteriosis;
- epidermal atrophy;
- hyperhidrosis;
- poor nutrition;
- wearing synthetic clothing;
- bacterial infections of the ENT organs;
- chronic inflammation in the skin.
Allergic reactions develop according to a standard pattern. The child is in constant interaction with an irritant that negatively affects the condition of the skin. Gradually, a rash appears on the body, localized in places of direct contact with the allergen. Potential and most likely irritants that provoke allergic reactions include:
- hygienic cosmetics;
- citrus;
- animal hair;
- paint and varnish products;
- medicines;
- synthetic clothing;
- polymer materials;
- houseplants.
The hereditary factor is of no small importance in the development of the disease. If neither parent suffered from dermatitis, the child has only a 10% chance of developing it. But if the mother or father has encountered the disease, the risk of its development in the infant increases to 80%.
Symptoms of an allergic reaction in a child
Signs of allergic dermatitis depend on the form of the disease and the age of the child. Typical (general) symptoms:
- hyperemia, peeling, swelling of the skin;
- burning, itching;
- skin rashes;
- the appearance of crusts;
- damage to the skin of the face, knees, elbows;
- thickening (lichenification) of the skin;
- the appearance of pigmentation.
Not all children develop additional signs. Associated symptoms:
- dermatitis of the abdomen, feet, hands;
- eczema;
- cracks, pallor, seizures on the lips;
- dryness of the epidermis;
- dark circles under the eyes;
- diathesis;
- cracks behind the ears;
- enlarged lymph nodes;
- weeping ulcers, erosions;
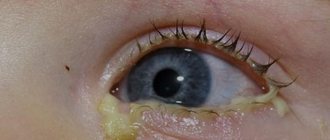
- conjunctivitis;
- nasal congestion, cough;
- restless sleep;
- increase in body temperature.
Article on the topic: Paracetamol for colds - indications for use, dosage for children and adults, list of drugs and prices
What does allergic dermatitis look like?
The external manifestations of the disease and its location depend on the age of the child. There are 3 types of allergic dermatitis:
- Infant (0-2 years). Allergic dermatitis on the face (cheeks), body, elbows and knees, characterized by a weeping rash. The skin remains dry and crusts appear on it. The head is covered with scales - keratinized particles of the epidermis.
- Children (2-12 years old) – the neck, scalp, inguinal folds, wrists and feet are strewn with vesicles. After opening, liquid leaks out of them. Erosion becomes inflamed, heals and thickens.
- Teenage (12-17 years old) – red pimples all over the body (chest, legs, neck), which disappear on their own.
Causes of skin disease development
Pathology occurs when genetic conditioning is combined with negative external factors. Causes of allergic dermatitis:
- bacterial, viral infections;
- irrational nutrition (introduction of allergenic foods, early complementary feeding, intolerance to formula milk);
- children's items made from fabrics with dyes, synthetics;
- diseases of the gastrointestinal tract (gastritis, dysbacteriosis);
- food allergy of a pregnant or lactating woman;
- helminthic infestations;
- incorrect use of medications;
- pet hair, dust, insect bites, pollen;
- nervous overexcitation, stress;
- passive smoking;
- unfavorable ecology (air and water pollution);
- low-quality children's cosmetics with fragrances, laundry detergent;
- seasonal weather changes.
How to treat allergic dermatitis in children
Diagnosis and treatment of the disease is carried out by children's doctors - pediatrician, dermatologist, allergist and immunologist. Treatment of allergic dermatitis in children is complex. It is aimed at identifying and eliminating the allergen. Recommendations:
- Take tests and a patch test for major allergens.
- Eliminate contact with the irritant.
- Make sure that your baby does not scratch the wounds.
- Keep the children's room clean.
- Treat the baby in a hospital.
Treatment tactics for young children
Mild dermatitis can be treated at home. For babies up to one year old, the following are shown:
- Emollients ( Topicrem, Emolium ) - apply to the skin 2-3 times a day to protect, soften and moisturize.
- Antihistamines ( Fenistil, Zodak ) - 3-5 drops orally 3 times a day, to relieve itching and burning.
- Sorbents ( Lactofiltrum, Enterosgel ) - used internally, according to the instructions, to remove toxins from the body.
- Healing creams ( Bepanten, Actovegin ointment ) - apply to the skin 2 times a day for tissue regeneration.
- Antiseptics ( Miramistin, Chlorhexidine ) - treatment of affected areas before applying ointment or to prevent the development of a secondary infection.
For moderate and severe forms of dermatitis, serious medications are required:
- Anti-inflammatory ( Triderm, Tsindol ) - apply to the affected areas 2-3 times a day to reduce swelling and hyperemia.
- Non-hormonal ( Vundehil, Fenistil gel ) – 2 times a day to relieve itching, heal wounds and cracks.
- Immunomodulators ( Viferon, Timalin ) - as prescribed by a doctor to stimulate the immune system during viral infections.
Treatment of allergic dermatitis in children over one year of age
Treatment of the disease in children over one year of age is similar to the regimen for infants; it can be supplemented with stronger drugs:
- Hormonal ( Sinaflan ) – for extensive skin lesions.
- Non-hormonal ( Radevit ) - use local ointments 2 times a day for minor blistering rashes.
- Antibacterial ( Levomekol, Dioxidin ) - to prevent the development of secondary infection.
- Desensitizing ( Cetrin ) - to eliminate itchy manifestations.
- Wound healing ( Solcoseryl ) – for purulent and weeping erosions.
- Glucocorticosteroids ( Prednisone ) - as prescribed by a pediatrician for acute dermatitis.
- Probiotics ( Bifiform ) – to normalize intestinal microflora after taking medications.
- Vitamins ( B6, C, A, D ) – to support the body’s defenses.
- Antipruritic ( Zyrtec, Loratadine ) – to reduce burning and irritation on the skin.
Article on the topic: Everything about modern antidepressants: list of the 30 best drugs at the end of 2021
Health Hazard
Acute dermatitis in infants and older children can become chronic and cause serious complications. Inflammatory processes in the skin disrupt its barrier function, which creates favorable conditions for the development of secondary infections. When the vesicles are opened, the risk of tissue infection by pathogenic bacteria and the development of streptoderma increases.
Children with severe forms of toxic-allergic dermatitis may experience disturbances in the functioning of the kidneys, heart, liver and lungs.
Abscesses and erosive formations that appear on the skin can leave scars. Therefore, rashes on the face must be treated with antiseptics that prevent infectious agents from entering the body. In patients with severe toxicoderma, the functioning of the lungs, kidneys, heart and liver is often impaired.
Hypoallergenic diet for dermatitis in children
Diet is an important factor in the successful treatment of allergic dermatitis. A bottle-fed child who is intolerant to cow protein is transferred to hypoallergenic formula. If your baby is breastfed, follow these nutritional rules:
- Avoid chocolate, citrus fruits, and honey.
- Eliminate fried, spicy foods, fast food, sweet soda, and baked goods from your diet.
- Avoid products with gluten, preservatives, dyes, and harmful additives.
For children over 6 months of age, the diet consists of the following products:
- green fruits and vegetables (zucchini, apples, cauliflower, pears);
- lean meat, river fish (turkey, veal, perch);
- fermented milk products (kefir, yogurt, cheese, cottage cheese);
- cereals (buckwheat, millet, lentils, rice).
Recommendations for nutrition for babies up to one year:
- Start complementary feeding no earlier than 6 months.
- Let's start with dairy-free porridge.
- Introduce new foods if remission is stable.
- Give complementary foods at the end of the main feeding.
- Keep a food diary of your child's reactions to new foods.
A child over one year old needs a balanced diet with all the necessary substances. Recommendations:
- Small meals - 5 times a day.
- Do not force your child to eat (the baby’s body itself knows how much food it needs).
- Let's have porridge for breakfast.
- Ensure drinking regime - at least 800 ml of clean water per day.
- Make a lunch of boiled or steamed food.
- Use vitamin and mineral complexes to eliminate the deficiency of essential substances.
- Make small portions.
How to prevent the rash from recurring
To prevent relapses of the disease, it is necessary to monitor the condition of the skin, diet and immune status of the child’s body. Compliance with preventive measures reduces the risk of re-formation of a rash on the body:
- Do not smoke in a room where children are present;
- in the apartment and children's room you need to do wet cleaning at least once every 2-3 days;
- it is necessary to remove all soft toys and things that accumulate allergenic dust;
- When washing children's clothes, it is advisable to use only hypoallergenic washing powders.
To restore the functions of the immune and digestive systems, children are prescribed vitamins and special dietary supplements. For a month after relief of the main symptoms of the disease, it is recommended to follow a hypoallergenic diet. When introducing complementary foods, foods with high allergenicity (oranges, milk, red apples, carrots, tomatoes, mushroom broths) are avoided.
The likelihood of allergic dermatitis largely depends on the condition of the gastrointestinal tract and skin. Timely treatment of gastroenterological and dermatological diseases reduces the risk of allergic inflammation by 2-3 times.
Physiotherapy for skin diseases
At the stage of remission of the disease, physiotherapy is prescribed:
- Laser (from 1 month) – exposure of lesions to low-intensity radiation.
- Phototherapy (from 1 year) – irradiation with ultraviolet light rays.
- Electrosleep (from 3 years of age) – pulsed currents reduce disorders of the autonomic system.
- Mud therapy (from 6 months) – application of therapeutic mud to the skin in order to restore it.
- Electrophoresis (from birth) – percutaneous administration of medications under the influence of constant electrical impulses.
Prognosis and prevention
Episodes of allergic dermatitis decrease as the child gets older. In the absence of a chronic course and secondary infections, the outcome of the disease is favorable. If there are factors that aggravate the nature of dermatitis, complications are possible:
- pyoderma (purulent infection);
- atrophic ulcers;
- bronchial asthma;
- eye diseases;
- anaphylactic shock.
Methods for preventing skin disease:
- long-term breastfeeding;
- following a hypoallergenic diet;
- use of safe children's cosmetics;
- maintaining the child’s personal hygiene;
- selection of clothing made from natural fabrics;
- daily moisturizing of baby's skin;
- strengthening the immune system (walking in the air, hardening).
Treatment Basics
Treatment of allergic dermatitis in children is a protracted undertaking that involves the use of a whole range of medications. The list of drugs used includes drugs from the following groups:
- antihistamines;
- corticosteroids;
- antiseptics;
- prebiotics;
- antibiotics.
Topical treatment is preferred in children
There are other methods to treat allergic dermatitis in a child. We are talking about non-drug methods. The main ones are:
- physiotherapy;
- diet therapy.
About