Why does a child often get colds?
If a child often suffers from colds, this means that the body’s defenses are not yet sufficient to protect against unfavorable environmental conditions.
Coughs, colds, fevers, vomiting and diarrhea - children's immune systems learn to cope on their own.
Illness is a baby's way of strengthening their immune systems for their future health.
When babies are born, they take their immune system strength from their mother. Antibodies are special proteins that fight infection, and children are born with large amounts of them in their blood. These maternal antibodies give a good start in helping to fight infections.
When a baby is breastfed, this effect increases because mother's milk also contains antibodies that reach the baby and help fight the disease.
As the child grows up, the antibodies that the mother gave die, and the child’s body begins to create its own. However, this process takes time. In addition, the child must come into contact with pathogens in order to create protective factors.
More than 200 different viruses and bacteria cause colds, and a child develops immunity to them one at a time. Each time a pathogen appears in the body, the child's immune system increases its ability to recognize the pathogenic organism. However, there are so many pathogens around that when the body overcomes one disease, another infection comes. Sometimes it seems that a child is constantly suffering from the same illness, but usually it is several different pathogens.
Unfortunately, it is normal for a child to be sick. A baby gets sick more often than adults because his immune system is not yet functioning at full capacity. In addition, he does not yet have immunity to the various viruses and bacteria that cause colds.
Being around other children also increases the risk of catching a cold. Carriers of viruses and bacteria also include older brothers and sisters who bring home the infection from school or kindergarten.
Studies have shown that children attending educational institutions have more colds, ear infections, runny noses and other respiratory problems than children at home.
During the cold months, your child often suffers from colds as viruses and bacteria spread throughout the country. This is also the time when the indoor heating turns on, which dries out the nasal passages and allows cold viruses to flourish.
How to boost your immunity
Every person needs a strong immune system, especially children who fall into the “frequently ill” category. Considering that the baby’s immunity is not yet fully formed, parents need to approach strengthening the baby competently, armed with comprehensive measures.
The first question that mommy faces is whether it is worth taking a constantly ill baby to the garden. You cannot find a single mother who would not encounter the problems of frequent illnesses in her child in the first year of going to kindergarten. This is a natural and adequate reaction of the body to changing conditions, communication with new children, separation from mommy.
For a strong immune system, it is vital for the body to recognize viruses and bacteria. And the sooner the baby gets acquainted with childhood diseases, influenza, ARVI, the better for him. Otherwise, you will have to not study at school in the future, but be sick at home - sooner or later, the immune system will take its toll. What advice can I give to mothers of children with disabilities regarding kindergarten:
- Don't rush to give up your preschool education! If the child is constantly sick, write an application to the head of the kindergarten to grant leave to the child while saving his place.
- At this time, take care of strengthening your immune system: vitamins, daily routine, gymnastics, sports and regular walks in the fresh air.
- If there are special kindergartens for children in the city, try to transfer your child there. In such institutions, children receive health activities, hardening, and physical therapy.
- Vaccinate your child against influenza annually. If the baby gets a cold, vaccination will help to cope with it in a mild form.
- Get advice from an immunologist on how best to strengthen your body.
- Listen to the position of child psychologists.
Psychologists are of the opinion about the importance of visiting gardens. This is an opportunity for a little person to get acquainted with the problems of adaptation among peers. In the absence of such experience, there is a high probability of increased conflict situations at school, leading to stress for the little person.
According to pediatricians, it is better for a person to become familiar with childhood diseases at a young age - chickenpox and measles in adults are much more severe and lasting, with complications.
Watch your child - if the breaks between illnesses (when visiting kindergarten) become longer, the body adapts. But when there is no break in illnesses, and the illnesses become more serious, think about a full examination of the baby by doctors. To identify the existing problem and cure the child once and for all.
Sanatoriums
In our country, the “Mother and Child” program exists and successfully operates, allowing hundreds of children from all Russian regions to visit health resorts annually, accompanied by their mothers, on preferential terms. A free voucher is issued under the following conditions:
- Large families.
- Presence of disabled children.
- Children included in the category of private children.
- With the presence of chronic diseases.
- If children are registered at the clinic's dispensary.
Since 2010, the rights to issue free referrals have been vested in regional authorities (each constituent entity of the Russian Federation implements a program with individual nuances). Detailed information should be obtained from the local social security department and children's clinic. The general principles for the implementation of this program include a set of required documents/certificates and conditions for obtaining a voucher.
The referral gives the right to use health-improving services free of charge and undergo full spa treatment in any health resort in Russia for children over 4 years old. But, if a child is diagnosed with a chronic disease, he can go to a sanatorium even at a younger age. To take advantage of this opportunity, a package of documents is required:
- Certificate of birth of the baby.
- Documents of the accompanying parent.
- Honey. child insurance policy (copy).
- Certificate form 070/у-04 (issued at the clinic).
- Completed application (the template is available on the Internet resource of the Ministry of Health).
The clinic submits a package of documents to the Ministry of Health of the Russian Federation for inclusion in the state program. Also, if parents decide to use such services, the child should apply for a sanatorium-resort card. It records the results of the child’s examination: general blood test, ECG, fluorography, expert opinions.
Be aware that during the peak season, due to the large number of vacationers, there may not be enough places in the health resort. It is better to plan your trip in winter or autumn.
When planning expenses, consider one nuance: the State program does not provide for travel expenses. Such expenses fall on the parents' shoulders. But there are exceptions: if the family’s income is less than the subsistence level, or there is a disabled child in their care, the state pays part of the costs (or the full amount) for the cost of travel to the place of treatment.
Compensation is issued upon return from the sanatorium. Be sure to check this question with the social authorities. protection.
Hardening program
To strengthen the immune system, the baby should be introduced to hardening procedures. Conscious parents understand the importance of hardening, but when approaching the procedures they make serious mistakes:
- Caution is key. Some mothers believe that by rinsing their baby’s heels with cool water after bathing, they have made a breakthrough in working on hardening. In fact, the child’s body does not even notice such “stress”.
- Temper it right away. Another extreme to which young parents throw themselves is too much workload without prior preparation. The movement on the path to hardening should be gradual, and the loads should be progressive and systematically growing.
So how to properly toughen up a child from the CHBD group? Take the “golden mean” and carefully study the basic four rules of hardening:
Gradualism. When bathing your baby, gradually (by 1-2⁰) lower the temperature of the rinsing water. Get your baby used to walking barefoot on a cool floor - you should start with short runs of 4-5 minutes, increasing the time each time.
Don't bundle up. From the very first days of life, dress your baby according to the weather. After all, the child’s body immediately gets used to the conditions that are created for it. If parents try to insulate their baby as best as possible in the first months of life, his body will decide that he lives in a hot climate and will react to a sudden cold snap with a malfunction.
Don't overload. Do not expose your small body to heavy loads. If after a walk your baby has wet feet, do not let him barefoot on the cold floor. This will cause unnecessary, dangerous additional hypothermia.
Only a healthy body can be hardened. You should vaccinate your baby against exposure to cold only if he is not currently sick. The first week after vaccinations you should also not do this. In moments of illness, the young body throws all its strength into fighting the infection, and new difficulties turn out to be beyond their strength.
The list of activities from which an individual hardening plan for children of the CHBD group is drawn up:
- Regular rinsing with cool water after taking a bath.
- Walking barefoot through the forest, grass, sand (in summer), on a cold floor.
- Bathing in a bath with a water temperature below +34⁰ C.
- Including cold foods (ice cream, cool juices) in the children's menu, provided that the throat is not inflamed at this moment. The number of such products should be gradually increased.
- Allow the child to walk without a hat (provided that the air temperature is above +14⁰ C and there is no wind outside). Make sure your baby is actively moving if he is walking without a hat.
- The baby must sleep at night with the window open, regardless of the time of year. If the air outside is too dry in winter, install a humidifier at home to normalize the microclimate.
- Daily walks regardless of the weather. Gradually reduce the amount of clothing so that your baby gets used to the cool air.
Health-improving and hardening procedures do not provide a 100% guarantee that the child will stop getting sick altogether. But a strong, hardened body will become much easier and faster to endure any infections.
Physiotherapy
A simple and affordable way to prevent ARVI in children is simple physical exercises that are interesting for little ones and useful for strengthening the body. Gymnastics should be performed 2-3 hours before a night's rest and no earlier than an hour after eating. The main condition for carrying out the exercises is not difficult breathing.
Before charging, clean your baby’s nose with a cotton swab dipped in warm oil. You should start working out with your baby from 3-5 minutes, gradually increasing the duration of classes to 15-20 minutes. It is better to carry out such gymnastics in a playful way that is interesting for the baby:
- Soldier. Invite your child to play soldier - let him walk in a circle, raising his knees high on his heels and toes (1-2 minutes).
- Watch. Feet at shoulder level, handles on the belt. Tilt your body left and right. So the clock ticks - tick-tock, tick-tock (2-6 times).
- Wind. The baby rises on his toes and stretches up the stick, which he holds with both hands: the wind rises. Then he slowly squats, without bending his back and with his knees spread to the sides, holding the stick straight in front of him and saying the sound “sh-sh-sh”: the wind subsides (4-7 times).
- Woodcutter. Raise your hands up and clasp your fists. The legs stand shoulder width apart. Inhale deeply, as you exhale, bend your body forward and sharply lower your arms, pronouncing the sound: “uh” (3-5 times).
- We run away. The child runs in place, gradually switching to walking (1-2 minutes).
- Cyclist. The baby lies with his back on the floor, arms along his body. You need to lift your legs up and rotate them one by one, as when riding a bicycle (3-5 times).
- Walking. We finish the exercises with calm walking (20-30 seconds).
Gymnastics for a healthy throat. Skiing, skating, running, cycling, and a swimming pool are useful for the strength of the respiratory system of a child. Include in your daily set of exercises and health-improving gymnastics for the throat and lungs:
- Dudochka. The baby is sitting on a chair. Invite him to imagine that he is holding a pipe in his hands and playing it, saying: “pfff” (5 times).
- Cockerel. Stand straight with your legs slightly apart, arms along your body. The baby raises his arms up and to the sides. Then you need to pat your legs with your hands, saying: “crow”. Exhale and repeat (3 times).
- Locomotive. The baby walks around the room, pretending to be a train, making circular movements with his hands, saying: “chug-chug” (20 seconds).
- Geese. The child walks slowly, while inhaling, raises his arms to the sides, while exhaling, lowers them, says: “ha-ha-ga” (50-60 seconds).
- Crow. The kid portrays a curious crow. He turns his head, looks sideways at the object and croaks loudly (4-5 times). And then the bird became hoarse - the child croaked, but silently, without opening his mouth (5-6 times).
- Horse. Now the baby has turned into a cheerful horse. She runs in circles and clicks (30 seconds).
- Snake. The snake has such a long tongue! Ask your baby to stick out his tongue and try to reach his chin (5 times).
Homeopathy
Homeopathy is an alternative, non-traditional medicine that has been around for over a thousand years. Homeopathic medicines are crushed herbs compressed into tablets. The principle of homeopathy is to treat “like with like”.
Treatment is based on taking microdoses of drugs that cause symptoms similar to those of the disease for which the person is being treated. In the practice of pediatricians, homeopathy takes pride of place, because such drugs:
- Absolutely harmless and effective.
- Increases the body's immune strength.
- They do not cause addiction and allergic manifestations.
- Can be successfully combined with any medical treatment.
- They have a wide range of therapeutic effects.
- They affect all organs of the body, stimulating the activity of the defense forces.
A well-chosen homeopathic course not only regenerates “broken” immunity, but also solves other problems: restores the functioning of the gastrointestinal tract, resuscitates vascular and nervous dysfunction, and eliminates allergies.
Attention! Don't self-medicate! Only a homeopathic doctor can develop a homeopathic course of healing. The specialist, taking into account the baby’s health status, medical history, temperament, habits, reactions to vaccinations, develops an individual plan for taking homeopathic remedies.
What is the normal frequency of colds?
It would seem that the norm should be considered as the absence of a disease, but medical statistics have established that the normal development of a child after birth does not exclude a recurrence of the disease.
If a child under one year old has had a cold at least 4 times, he can already be classified as a frequently ill child. From 1 to 3 years old, these children catch colds 6 times a year. From 3 to 5 years, the frequency of colds decreases to 5 times per year, and then - 4 - 5 acute respiratory diseases every year.
An indication of a weakened immune system is the frequency and duration of illness. If an acute respiratory infection and cold do not disappear after 2 weeks, it means that the child’s immunity is weakened.
What do schoolchildren get sick with most often?
Children at school get sick mainly from those ailments that are easily transmitted from person to person. These are colds, flu, rubella, chickenpox, skin lesions of various natures and even lice. There are plenty of threats. But, oddly enough, younger schoolchildren are beginning to develop diseases that cannot be contracted. For example, scoliosis, gastritis, neurological disorders. It would seem, where is the connection?
Contagious diseases are understandable. But what about the non-infectious ones? Parents usually think that their children get sick because of school. Allegedly, the workload in educational institutions is too heavy, there are no conditions for normal development, and so on. In fact, non-communicable diseases do not appear out of thin air.
Most often , they simply worsen when the child goes to first grade, or returns to school after a long summer vacation. There is additional workload, stress, and you have to put in more physical effort. As you know, “where it’s thin, it breaks.” This is where all the problems pop up that were previously either not noticed by parents or were in their infancy.
Some diseases are purely neurotic in nature. First of all, this applies to headaches and neuroses themselves. But this can also include, for example, a runny nose. Now we see that there are a huge number of diseases to which schoolchildren are exposed. Let's move on to the reasons for their occurrence and methods of struggle.
Causes
A number of conditions undermine the child’s health and immune system:
- premature birth;
- intrauterine infection;
- early interruption of breastfeeding;
- contact with a large number of peers and adults;
- surgical intervention;
- a serious illness that undermines the immune system: pneumonia, sore throat, consequences of severe flu;
- presence of parasites;
- chronic diseases (often chronic tonsillitis, sinusitis, adenoiditis);
- inability to follow the correct daily routine (lack of complete and timely rest, poor nutrition);
- long-term drug therapy with certain drugs (antibiotics, immunosuppressants, steroids).
- complications of a cold.
Frequent colds can lead to quite serious complications in a child. Although these complications are not very common, it is important to be careful and aware of them.
Complications that may occur soon after a child catches a cold:
- There is a risk that babies suffering from the common cold will develop an ear infection. These infections can occur when bacteria or virus travels into the space behind the baby's eardrum;
- a cold can lead to wheezing in the lungs, even when the child does not have asthma or other respiratory diseases;
- colds sometimes lead to sinusitis. Sinus inflammation and infection are common problems;
- Other serious complications caused by the common cold include pneumonia, bronchiolitis, lobar pharyngitis, and streptococcal pharyngitis.
Frequently ill child syndrome
A child who is often sick - what to do? To begin with, understand that this is not a diagnosis at all. This is a clinical observation group. It includes children who often suffer from respiratory infections, and this is not associated with obvious congenital and hereditary pathologies. Formally, the group of “frequently ill people” is defined as follows:
- if a child is aged 3 to 4 years, he gets sick more than 6 times a year;
- if a child is aged 4 to 5 years, he gets sick more than 5 times a year; - if the child is over 5 years old, he gets sick more than 4 times a year.
When this happens, parents often blame the “bad doctors” and begin to torture their children with new and new medications on their own - which can only worsen the problem. If a child is often sick, this means that he is constantly exposed to sources of infection. They can be inside the body itself or in the external environment - for example, with a large number of contacts with people. It is no coincidence that many parents associate the surge in diseases with the child’s beginning to attend kindergarten. But the reasons can also be at home, in the family.
External factors of frequent child morbidity:
- lack of sanitary culture in the family, defects in care, for example, poor nutrition, not taking the child for walks or doing physical exercise;
- material disadvantage, poor sanitary and living conditions, and in quite prosperous families, on the contrary, overprotection of the child;
- uncontrolled use of antibiotics, antipyretics, which disrupt the functioning of the child’s body’s protective factors;
- the presence of chronic diseases of the ENT organs in parents and other family members who live with the child; using shared utensils, etc.;
- vaccinations before visiting a child care facility. Many parents often delay vaccination until they enter kindergarten, and vaccines weaken the functioning of the immune system - as a result, the child gets sick a few days after the start of adaptation to the conditions of the kindergarten;
- parents did not take preventive measures before starting kindergarten, as a result the child’s body cannot cope with overwork and overexcitation of the nervous system;
- the child starts attending kindergarten (especially under the age of 3). At this age, children are very susceptible to respiratory diseases.
- a large number of contacts in places with large numbers of people: transport, supermarkets, etc.
The ENT doctor for my two children, Svetlana Danilova, usually categorically tells parents whose children suffer from sinusitis, otitis, and adenoiditis that they urgently need to take their children home from the institution for at least a couple of months. “If it were my will, I would close all the kindergartens,” Svetlana Vladimirovna categorically states.
But parents often do not have the opportunity to leave their child at home: either there is no one with them, or the financial situation does not allow only the father or mother to work.
Internal factors of frequent child morbidity:
- Pre- and postnatal unfavorable scenarios for the development of the child, for example, malnutrition, rickets, anemia, prematurity, hypoxia during childbirth, encephalopathy;
- early artificial feeding affects the maturation of the immune system;
- allergies, especially those that are inherited;
- the child has foci of chronic infection in the oro- and nasopharynx;
- there may be viruses and pathogenic flora on the mucous membrane of the child’s nasopharynx;
- “local” immunity of the mucous membrane of the respiratory tract does not work well;
- the child’s processes of thermoregulation and thermal adaptation are disrupted;
- disruption of the intestinal microflora.
Ivan Leskov , otolaryngologist, comments
“The real problem begins when the child has to be sent to kindergarten, where there are 20-25 people in the group. Of these, three or four are always in the prodromal period of infection, or come to kindergarten after sick leave - not fully treated. And although a 3-4 year old child can already develop antibodies to infection, the main link of immunity - the T-system - is not yet working (it is formed by the age of 5-6 years). This means that from 3 to 6 years of age there is a danger of the child developing chronic bacterial foci of infection (tonsillitis, adenoiditis), or persistent (Latin for “permanently resident”) chronic viruses, which, in particular, include the Epstein-Barr virus, adenovirus and cytomegalovirus. If a child is often sick, simply stimulating his immunity will not give the desired results.”
What to do?
Three competent steps will allow you to break the vicious circle: 1. Identify and sanitize chronic foci of infection;
- Get tested for antibodies to viruses;
- After completing the first two points, begin the rehabilitation of the child’s immune system
It is necessary to show the child not only to the pediatrician, but also to the otolaryngologist. It is the ENT doctor who can assess the condition of the tonsils, adenoids, paranasal cavities and eardrum. It is diseases of the ENT organs that cause frequent illnesses in children.
The ENT doctor should give a referral for analysis - culture from the mucous membrane of the pharynx and nose to assess the microbial condition. In the nasopharyngeal mucosa of frequently ill children, fungi of the genus Candida, staphylococci, Haemophilus influenzae (by the way, since last year children at risk have been vaccinated against Haemophilus influenzae infection free of charge), and enterobacteria often “live” peacefully. They are the source of the inflammatory process.
As a result of the evaluation of the tests, adequate treatment is prescribed. And only after the child has fully recovered can we begin to rehabilitate the immune system.
How to rehabilitate a child’s immune system?
herbal and homeopathic preparations in their practice . Most of us are familiar with adaptagen plants. To stimulate the immune system, eleutherococcus, echinacea, liceweed, levkoy, Schisandra chinensis, Rhodiola rosea, and Aralia Manchurian are used. Pharmacies sell extracts and tinctures of these plants. In practice, the following dosage is usually used: 1 drop of tincture for 1 year of life. During the epidemic period, immunomodulators are given to the child during the week - excluding weekends - for a month.
Experts in bee products claim that immunity can be boosted with royal jelly, bee jelly, and propolis.
Of the medications, derinat has recently been much advertised; it activates cellular and humoral immunity. Less known are sodium nucleonate, potassium orotate, and safinor.
If a child constantly suffers from runny noses and otitis media, it is necessary to stimulate his local immunity. It is necessary to use drugs (on the recommendation of an ENT doctor and after tests) that normalize immunity in the mucous membrane of the upper respiratory tract. These medications contain lysates of bacteria. They help prevent infections in the nasopharynx. Ribosomal immunomodulators, bacterial lysates and membrane fractions and their synthetic analogues are known. I don’t specifically name the drugs themselves; they should only be prescribed by a doctor, preferably a good immunologist .
Fedor Lapiy , infectious disease immunologist, comments
“Before prescribing a drug, it is necessary to assess the child’s health condition. To begin with, a general blood test is looked at to see if the content of lymphocyte cells is normal. Their number indicates whether the child has a severe disorder of the immune system (the norm for children aged 4 years and older is 6.1 - 11.4x109/l). It is determined whether the child has suffered from pneumonia, purulent otitis media, meningitis and other serious illnesses. After this, other studies may be required - immunograms. They are different. Sometimes, in order to correctly assess what is happening with the child and prescribe adequate, effective treatment, an immunologist can prescribe a very narrowly targeted test. In this case, the immunogram itself will show the norm. But this will not mean that the problem has been resolved.”
It is good to carry out interferon prophylaxis . Even for newborns, pediatricians prescribe native leukocyte alpha-interferon (in ampoules) during seasonal morbidity. There are recombinant types of interferon - influferon and viferon (suppositories), anaferon and aflubin. Arbidol is an interferon inducer; in addition, it is also an antiviral drug. Don't forget oxolinic ointment. In the morning and evening, after you have cleared the child’s nose of mucus and just crusts, carefully lubricate the mucous membrane with a cotton swab with ointment applied to it.
There are also physical therapy options for restoring immunity. Many pulmonology departments and children's health centers have so-called gala chambers ; they simulate the basic parameters of salt caves. Highly recommended for children with bronchopulmonary diseases, allergy sufferers, and simply children who are often ill. Being in the halochamber activates T cells, the synthesis of endogenous interferon and the level of immunoglobulins increases. Usually two courses are conducted per year. For example, in autumn and spring.
Aromatherapy is a physiotherapeutic procedure using volatile biologically active substances. Depending on the use of the essential oil of a particular plant, there will be a corresponding effect. The anti-inflammatory and antibacterial properties of pine needles, lavender, laurel, fennel and basil oils are widely known. In aromatherapy, a strictly individual selection of essential oil is required.
A little forgotten UFO - ultraviolet irradiation . Physiotherapeutic rooms in children's clinics are usually equipped with these devices. As a result of exposure to ultraviolet rays, not only does the bactericidal activity of the blood increase, phagocytic activity also increases, and antimicrobial antibodies grow.
At the same time, we must not forget to perform other “non-drug” health measures. Everyone knows about them, or has at least heard of them, but following these absolutely competent instructions requires pedantic consistency from adults. Rules must become the norm of life.
- Properly organize the child's daily routine. He should take a walk, play, and go to bed on time.
- Avoid stress. Extinguish all conflict situations in the family. As psychologists correctly note: very often a child gets sick in families where there are unresolved situations between parents. The baby thus attracts the attention of the opposing parties to himself. In another option, the child’s immunity decreases due to constant stress due to the situation in the family.
- to rinse your nose several times a day with a solution of table salt (0.9%) or saline solution (costs a penny). Many parents buy sprays, for example, Aqua-Maris. To save money, after the solution in the purchased product runs out, you can carefully remove the cap with pliers and pour saline solution into the bottle. Cheap and cheerful. Other spray systems do not allow for reuse.
- Rinse your throat with infusions of herbs, for example, chamomile.
— Gradually introduce hardening procedures. Training the vascular response to cooling - ensures good blood supply. As a result, the number of killer cells (phagocytes) grows on the child’s skin and mucous membranes; they destroy foreign microorganisms.
- Go for walks often. Only high fever and other borderline situations can force you to stay home. Try not to go with your child to stores and other crowded places. Dress your offspring appropriately for the weather and physical activity.
- Feed varied and prudently . Supplement fresh vegetables, fruits and berries with vitamin and mineral complexes (3-4 times a year).
- Use adaptogens. They will help the child restore immunity.
— Provide access to clean air. Ventilate more often, at least before going to bed, wet clean the floor in the child’s room. If possible, remove dust-collecting carpets. Or clean them often and very thoroughly.
- to take your child to the sea at least once a year , preferably for two weeks (no less). If this is not possible, go to the village, now open the fashionable summer season. The child should be given the opportunity to clear the bronchi from city air and indoor allergens. Summer is the most favorable time to start hardening procedures. What could be better - pour cold water on the baby’s feet on the grass or run with him along the river bank, and then take a swim in the sun’s spray...
— Make a schedule for visiting specialists. For a frequently ill child, such pedantry is very important. The main ones are pediatrician, otolaryngologist, dentist, physiotherapist. For additional indications: exercise therapy doctor, allergist, immunologist, neurologist.
How to help a child?
It is known that the health of the child will depend on the behavior of the mother during pregnancy and its planning. Timely detection and treatment of existing infections and proper nutrition, good health and successful childbirth have a beneficial effect on the health of the child. This is also important during infancy.
For example, not all parents understand that not only the mother’s smoking is dangerous for the child, but also volatile substances from tobacco products carried by family members on their hair and clothes. But these measures are ideal as preventive measures.
What to do if your child often gets colds:
- Proper nutrition. It is necessary to teach your child to eat healthy foods, because a proper diet allows you to get the required vitamins and minerals. Various snacks are not only harmful in their composition, but also suppress the natural feeling of hunger, forcing the child to give up wholesome and healthy food.
- Organization of living space. A common mistake mothers make is organizing complete hygienic sterility, which could compete with operating room conditions. But to maintain the child’s health, wet cleaning, ventilation, and removal of dust collectors are sufficient.
- Hygiene rules. Developing the habit of washing your children’s hands after going outside, using the toilet and before eating is the most important rule. The sooner hygiene skills are instilled in a child, the more likely it is that he will begin to observe them without being under the control of his parents.
- The hardening that a healthy child receives naturally is light drafts, walking barefoot, ice cream and drinks from the refrigerator. But this is a prohibition for a constantly ill child. However, in order to accustom him to natural conditions, it is necessary to spend holidays at sea or in the countryside, and a morning rubdown with cold water does not look so scary.
Recommendations for adults
Sometimes parents do not understand why their child is constantly sick. Look deep into your own family, what kind of psychological climate reigns at home? Doctors claim that the answer to CBD lies in the unresolved problems of adults. The body is inextricably linked with the psyche - if a person has psychological problems, the body becomes ill.
Statistics have proven that the percentage of NBI is 2-3 times higher in disharmonious families.
The relationship between dad and mom plays a big role. It has been noticed that a child, seeing his parents quarreling, gets sick, unconsciously trying to “hold together” a falling apart family. And the illness will become protracted, since the little one is subconsciously afraid that as soon as he recovers, the quarrels will resume.
Differences between parents in their views on raising a child play an important role. The contradictions of adults cause stress in the little one - the child does not understand whom to listen to. And where there is unrest, there is illness. What about personality traits? After all, the baby copies the habits of adults. If a wife knows how and is used to manipulating her husband by pretending to be sick, expect the same behavior from the child.
The baby gets sick if he does not feel cared for by his parents. After all, a sick child receives a lot of attention - he is given treats, they take care of him and ask him how he is doing.
Moms and dads, remember a simple truth - the main reason for the baby’s constant illnesses lies in the lack of love for him. Do not forget to take an interest in the life of a little person, learn to understand his emotions and moods. And then most diseases will fade into the background.
The child is often sick in kindergarten
Almost everyone has this problem. When the baby sits at home, he almost never gets sick, and as soon as the child goes to kindergarten, the diagnosis of acute respiratory infection (ARI) is made every 2 weeks.
And this phenomenon depends on a number of reasons:
- adaptation stage. In many cases, a child often gets sick in kindergarten during the first year of attendance, regardless of the child’s age. For most parents, the hope is that the adjustment period will pass, the stress will decrease, and the constant sick leave will stop;
- infection acquired from other children. Not wanting to go on sick leave (or not having the opportunity), many parents bring children with primary cold symptoms to the group, when the temperature has not yet risen. A runny nose and a slight cough are faithful companions for those attending an educational institution. Children easily infect each other and get sick more often;
- inappropriate clothing and footwear. Children go to kindergarten every day, except on especially cold days and weekends.
Make sure your child's clothes and shoes are always appropriate for the weather and comfortable for him. Shoes and outerwear should be waterproof and warm, but not hot.
If a child gets sick very often in kindergarten, the only way is to try to strengthen his immunity. Start gradual hardening, ventilate the rooms, enroll your child in the swimming section, follow the principles of healthy nutrition and give vitamins. Regarding the latter, consult your pediatrician first.
The ideal way to properly adapt to kindergarten is gradual habituation. In the first 2 - 3 months, it is better for a mother or grandmother to take a vacation or work part-time so as not to leave the child in the group for a long time. Increase the time gradually to reduce your stress levels.
And when a child gets sick, do not rush to go to work and return the child to the group. It is important to wait for complete recovery so that there are no relapses or complications.
How to strengthen children's immunity
Strengthening the immune system is a system of measures aimed at healing the body and restoring its defenses.
How to strengthen a child's immunity? It's not too difficult. But the whole family may have to change their usual lifestyle a little. You can achieve what you want using the following actions:
- regular and nutritious meals,
- sufficient sleep duration,
- walking,
- feasible physical activity,
- vitaminization,
- hardening.
Remember that everything is good in moderation. You shouldn’t get too carried away with any of the above. Regularity and common sense are the path to health.
Why does a child often get a sore throat?
The common cold is, in fact, a big threat.
Lack of proper therapy and refusal of bed rest are fraught with complications.
The most common type of complication of respiratory disease is sore throat, or, medically speaking, tonsillitis.
Tonsillitis is an inflammation of the tonsil tissue due to infection of bacterial and viral origin.
The tonsils are part of the lymphatic system and form the body's first line of defense. They are present on the left and right sides inside the throat and appear as two pink structures at the back of the mouth. The tonsils protect the upper respiratory system from pathogens that enter the body through the nose or mouth. However, this makes them vulnerable to infections, leading to tonsillitis.
Once the tonsils become affected and inflamed, they become large, reddish, and covered with a whitish or yellowish coating.
There are two types of tonsillitis:
- chronic (lasts more than three months);
- recurrent (frequent disease, many times a year).
Causes of tonsillitis in children
As mentioned earlier, the predominant cause of tonsillitis is an infection of viral or bacterial origin.
1. Viruses that usually lead to sore throat in children:
- enteroviruses;
- influenza virus;
- adenoviruses;
- parainfluenza viruses;
- herpes simplex virus;
- Epstein-Barr virus.
2. Bacterial infection is the cause of 30% of tonsillitis cases. The main cause is group A streptococci.
Some other bacteria that can cause tonsillitis are chlamydia pneumoniae, streptococcus pneumoniae, staphylococcus aureus and mycoplasma pneumoniae.
In rare cases, tonsillitis is caused by fusobacteria, the causative agents of whooping cough, syphilis and gonorrhea.
Tonsillitis is quite contagious and easily spreads from an infected child to other children through airborne droplets and household contact. This infection mainly spreads among young children in schools and among family members at home.
Reasons for recurrent infection include a child's weakened immune system, resistant bacteria, or a family member who is a carrier of streptococcus.
One study showed a genetic predisposition to developing recurrent tonsillitis.
3. Dental caries and inflamed gums cause the accumulation of bacteria in the mouth and larynx, which also causes a sore throat.
4. An infected state of the sinus, maxillary, and frontal sinuses quickly provoke inflammation of the tonsils.
5. Due to fungal diseases, bacteria accumulate in the body that are difficult to treat, which reduces resistance and causes frequent relapse of tonsillitis.
6. Less commonly, inflammation can be caused by injury. For example, chemical irritation from severe acid reflux.
When a child has frequent sore throat, you must understand that every time he suffers great damage. The tonsils are so weakened that they cannot resist germs and protect against infection. As a result, pathogens begin to cling to one another.
A child who often suffers from sore throat may experience many complications.
Tonsillitis can lead to the following consequences:
- adenoid infection. Adenoids are part of lymphatic tissue, just like tonsils. They are located at the back of the nasal cavity. Acute infection of the tonsils can infect the adenoids, causing them to swell, leading to obstructive sleep apnea;
- peritonsillar abscess. When the infection spreads from the tonsils to the surrounding tissue, it results in the formation of a pus-filled pocket. If the infection subsequently spreads to the gums, it can cause problems during teething;
- otitis. The pathogen can quickly find its way to the ear from the throat through the eustachian tube. Here it can affect the eardrum and middle ear, causing a whole new set of complications;
- rheumatic fever. If group A streptococci causes tonsillitis and the condition is ignored for a very long time, it can cause rheumatic fever, which is severe inflammation of various organs of the body;
- poststreptococcal glomerulonephritis. Streptococcus bacteria can find their way to various internal organs of the body. If the infection enters the kidneys, it causes post-streptococcal glomerulonephritis. The blood vessels in the kidneys become inflamed, making the organ ineffective at filtering blood and producing urine.
What to do if a child often gets a sore throat?
Persistent sore throat can affect diet, lifestyle, and even the education and development of a child. Therefore, it is common practice to remove the tonsils if tonsil inflammation is a recurring problem.
However, tonsillectomy (surgical removal of the tonsils) is not the preferred treatment option. If your child has frequent tonsillitis, there are some ways to prevent it.
How to prevent recurring sore throat?
1. Frequent hand washing.
Many of the germs that cause tonsillitis are highly contagious. A child can easily pick them up from the air he breathes, and this is often inevitable. However, transmission of germs through hands is another common route and can be prevented. The key to prevention is good hygiene.
Teach your child to wash their hands frequently with soap and water. Use antibacterial soap whenever possible. Antibacterial hand sanitizers are great when you're on the go. Teach your child to always wash their hands after using the toilet, before eating, and after sneezing or coughing.
2. Avoid sharing food and drinks.
Saliva contains germs that can cause infection. By sharing food and drinks with an infected person, a child inevitably allows germs to enter his body. Sometimes these germs are airborne and can inevitably land on food and drinks. But the exchange of food and drinks must be excluded. Teach your child not to share food and drinks to avoid cross-contamination. It is better to separate or cut the food, pour the drink into glasses, but avoid sharing.
3. Minimizing contact with others.
You should try to prevent your baby from getting an infection that will lead to tonsillitis. When a child has tonsillitis, you should minimize his contact with others. This applies to any infection, especially if you know it is highly contagious. Let the child not attend school or kindergarten during illness, and do not come too close to other family members at home who may become infected. Even a trip to the mall or other outings means that a child can infect others. Let the child rest during this time and reduce contact with people to a minimum.
4. Removal of tonsils.
Tonsillectomy is a very effective way to stop frequent recurrences of tonsillitis. This does not mean that the child will never have a sore throat again. But it will give him a better quality of life. There are some myths and misconceptions about tonsillectomy, but it is a very safe procedure and complications are rare. Surgery is especially necessary if tonsillitis does not respond to antibiotics or serious complications develop (for example, tonsillar abscess).
5. Rinse with salt water.
This is one of the simple solutions, but also very effective. 1 teaspoon of regular table salt in a 200 ml glass of water makes this method quick and inexpensive.
It should only be used by children who are of an age where rinsing is safe. Remember that while rinsing may be helpful, it is not a substitute for medications prescribed by your doctor. Gargling with salt water soothes the throat and may give your child short-term relief from tonsillitis symptoms, but prescription medications such as antibiotics will kill the bacteria that is causing the problem.
6. Keep the air clean and humid.
Airborne irritants such as cigarette smoke are known to increase a child's chances of developing tonsillitis.
Cigarette smoking should definitely be eliminated from the home, but you should also be careful with cleaning products and other strong chemicals, the vapor of which can also be an airborne irritant. Even dry air that doesn't contain harsh chemical fumes can be irritating. A humidifier increases the moisture content in the air and helps with tonsillitis if you live in a dry climate.
7. Rest and drink plenty of fluids.
Providing adequate rest for a child with a sore throat can affect the duration and severity of his condition. It is necessary not only to stay away from school or kindergarten and sleep all day.
It is equally important to maintain vocal calm. Try to keep your child's conversation to a minimum while his throat heals.
Give your child plenty of fluids. Liquid foods are better tolerated compared to solid foods, which will rub the tonsils and irritate them further. Maintain good nutrition to support the immune system, which helps fight illness along with any medications your child takes.
8. Be aware of acid reflux.
Acid reflux is a common digestive disorder. Acidic stomach contents rise up into the esophagus and can reach the throat and nose. Therefore, the acid will irritate the tonsils and even damage them, increasing the likelihood of infection. Heartburn is a typical symptom of acid reflux, but sometimes it doesn't occur.
Always keep an eye on your child. And if he has acid reflux, change his diet and lifestyle.
What advice can you give to parents?
It is better to start taking care of your baby’s health before he is born. The expectant mother, if possible, should move from environmentally unfavorable areas. Some time before a planned pregnancy, it is worth parting with work involving heavy metals, especially lead, paints or solvents, as well as devices that emit strong electromagnetic fields.
Besides:
- Before planning a child, it is advisable for a married couple to be examined by an andrologist and gynecologist.
- When planning a pregnancy, the expectant mother must treat all her chronic diseases, including having her teeth sanitized.
- During pregnancy, you should protect yourself from stress and also avoid contact with people suffering from colds.
- After the birth of your baby, try to breastfeed him for as long as possible; do not switch your baby to artificial formula without special reasons. Transferring a child to artificial feeding before he is four months old deprives the baby of the mother's immunoglobulins - protective substances produced by her immune system. Therefore, do not forget: a child who is weaned too early is a direct candidate for the group of frequently ill children.
- If your child is often sick, get examined by a pediatrician, endocrinologist, or immunologist. Try not to “trigger” illnesses in your baby, don’t give up treatment halfway, don’t use untested treatment methods or advice from friends, contact specialists.
- Regularly give your child vitamins, strengthen him, and teach him a healthy lifestyle.
Based on materials from the magazine “Family Doctor” No. 10, 1999.
Why does a child often suffer from bronchitis?
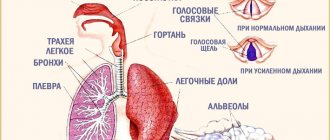
Bronchitis is an inflammation of the walls of the bronchi - the airways connecting the trachea to the lungs. The wall of the bronchi is thin and produces mucus. It is responsible for protecting the respiratory system.
Bronchitis refers to diseases of the upper respiratory tract. This especially often affects children from 3 to 8 years old due to immature immunity and structural features of the upper respiratory tract.
Causes of frequent bronchitis
The main cause leading to the development of bronchitis is a viral infection. The pathogen enters the upper respiratory tract and then attacks. This causes inflammation of the mucous membrane of the respiratory tract.
Other causes of frequent bronchitis:
- bacteria. The child often puts toys and other objects in his mouth. Together with these objects, bacteria that cause this disease enter the body;
- allergic reactions to dandruff, mold, dust, food. When such reactions happen frequently, it causes constant inflammation, which eventually causes chronic bronchitis;
- inhalation of vapors of various chemicals. A major role in the development of the disease is played by dust, impurities in the air of any toxic substances, gases, cigarette smoke;
- incompletely treated viral infections or colds;
- the presence of a large number of parasites in the body. They are able to penetrate the lungs and settle in them, constantly irritating and causing inflammatory reactions in the bronchi;
- congenital defects in the structure of the upper respiratory tract.
The first signs of ARVI
Adult schoolchildren usually do not attach much importance to cold and flu symptoms. A cough and runny nose are not a reason for them to refuse to go to the cinema or to a concert of their favorite band with friends. In order to start treatment on time, caring parents must closely monitor the well-being of their children. The warning signs are:
- redness of the eyes,
- nasal congestion,
- sore throat,
- sneezing,
- increase in body temperature,
- weakness,
- drowsiness,
- decreased appetite.