When should you see a doctor?
If a child’s Mantoux result does not correspond to the norm, then this is not yet a sign of tuberculosis infection.
But it’s still worth contacting a specialist. Indications for consultation with a phthisiatrician:
- Annual increase in papule size.
- The Mantoux test of other children in the family does not correspond to the norm.
- A sharp increase in infiltration volume compared to last year's results.
- Contact with patients with tuberculosis (especially those with open form).
- Detection of this disease in family members or close relatives.
The phthisiatrician evaluates not only whether the Mantoux size corresponds to the norm, but also the results of additional studies such as chest X-ray and microscopic examination of sputum. In some cases, additional computed tomography is required.
If the doctor suspects tuberculosis of another location (tuberculosis of bones, kidneys, tuberculous meningitis), then examination methods such as bone scintigraphy, ultrasound, spinal puncture, cytological examination, etc. may be prescribed.
Thus, the Mantoux test for tuberculosis is a diagnostic method for examining patients of different ages, so the concept of normal in children may have age-related differences. It has been proven that after the administration of tuberculin, adverse reactions may develop, but there is no risk of infection from the test.
There are clear criteria for assessing the result of a reaction. With the help of simple measurements you can find out whether the size of Mantoux in children corresponds to the norm or not.
Refusal of Mantoux
Often parents refuse to give any vaccinations to their children, everyone has their own reasons for this. Recently, there are more and more such mothers and fathers, but doctors do not have the right to force them to change their decision. Another question is how expedient this is. For example, a disease such as tuberculosis is considered very dangerous. From year to year it only gets younger and progresses even more. If parents categorically do not want their baby to be given Mantoux, they should know the instructions for subsequent actions.
In each medical institution, you can find an example of a sample refusal application on the information stand. Let’s say parents are firmly convinced that their son or daughter will never come into contact with a person with tuberculosis. In such a case, they should write a statement based on the sample and give it to the local pediatrician.
Only parents have the right to decide what is best for their children. In addition, modern medicine is able to diagnose the causative agent of this dangerous disease using other methods. For example, you can take an appropriate blood test or use Diaskintest. Similar methods are practiced in private clinics.
A child without Mantoux has every right to attend kindergarten . If a doctor does not grant admission to a preschool institution, you need to understand that his actions are illegal. However, there are some nuances here. Would a parent want to take their child to a group of 28 people, among whom, most likely, there will be an infected child. Such children do not show signs of the disease, but are its carriers.
What should be the normal Mantoux reaction in children?
After the first tuberculosis vaccination, immunity from this deadly disease does not disappear for 7 years. How long the protection against a dangerous pathology will last can be judged by the size of the rounded scar remaining on the shoulder after vaccination. The larger this size, the longer a person remains vaccinated against tuberculosis.
The reaction to Mantoux appears after the injection the next day. It looks like a small papule at the sample injection site. 3 days after the injection, the immune system reacts to the “invasion” of tuberculin with maximum force.
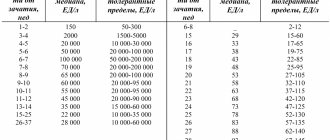
The Mantoux norm varies depending on the age of the baby:
Norm Mantoux, made for the first time at 1 year
For the entire year before the second test, almost all children’s reaction to tuberculin can be called doubtful or positive. For yearlings with a post-vaccination scar, redness is considered normal if its diameter is in the region of 5-11 mm.
The photo shows what the first Mantoux looks like:
Normal for children from 2 to 6 years old
In the 2nd year, anti-tuberculosis immunity is usually strongest. When the size of the post-vaccination scar exceeds 8 mm (that is, what it should be when the baby is 2 years old), then Mantoux can easily reach as much as 16 mm. When a child is over three years old, immunity to tuberculosis begins to weaken. However, in most cases, a positive or questionable reaction to tuberculin persists at 4, 5, and 6 years of age. During this period, the normal size for a papule is a maximum of 10 mm. To accurately determine which parameters are optimal at this age, you should compare it with the post-vaccination tuberculosis trace.
| Post-vaccination scar (mm in width) | Normal papule (in millimeters) |
| Maximum 2.0 | no reaction |
| Within 4.0-6.0 | 5,0-6,0 |
| 6.0 and more | maximum 10.0 |
At 6-7 years old
The reaction to the test performed in the vast majority of cases can be called questionable or negative. This is a sign that immunity to tuberculosis is beginning to disappear. That is why at the age of 7 all children receive a second anti-tuberculosis vaccination.
Normal for 7-14 years old
After revaccination, a new 7-year cycle begins. At the age of 3 to 10 years, the child has good reliable immunity against tuberculosis, and the size of the papule is between 10-17 millimeters.
When the baby becomes more than 10 years old, the immune response to the invasion of tuberculin begins to weaken, and the papule decreases to 5.0-6.0 mm. At 13 years old, the absence of any reaction or the presence of a questionable one is already the norm. The papule during this period is maximum 4 mm. By the age of 14, it often disappears completely.
What can affect the result?
If a person has a tendency to allergic conditions, this may affect the results of the Mantoux test, which is also considered a type of allergy.
When performing a tuberculin test, one should take into account age, the presence of chronic diseases, as well as the fact that any infectious disease has recently been suffered.
Children under 1 year of age, due to the fact that their immunity has not yet been fully formed, will also not be able to adequately respond to the Mantoux reaction.
The following factors are considered important: the presence of helminthiasis, very sensitive skin, malnutrition. They are also, oddly enough, capable of influencing the test results.
Now let's dispel all the myths. After the test, DO NOT:
- Scratch the puncture site.
- Strictly limit exposure to any chemicals in the Mantoux area.
- Bandage, apply an adhesive plaster and generally isolate the area.
If these rules are not followed, your child runs the risk of distorting the results obtained during the reaction, thereby nullifying all the efforts of doctors.
But, oddly enough, you can wet Manta. Probably, this tradition has remained since the times when tuberculin was administered cutaneously, and then staying in the water of the forearm after the start of the test was prohibited. But those days have passed, but the rule remains. Whatever you say, there are useless rudiments in medicine too.
Reasons for distorting the result
A number of different factors can distort the results of an injection (both positively and negatively). The culprits may be:
- chronic functional and organic diseases of internal organs and body systems;
- various infectious pathologies, especially colds with high fever. The Mantoux result can also be distorted in a healthy child who has recently suffered from some infectious disease;
- allergies of various natures. It is especially dangerous to test children who are intolerant to tuberculin;
- dermatitis and other skin diseases;
- liquid entering the place where the Mantoux test was placed. Even a very small amount of water can cause an allergic reaction and distort the result;
- unfavorable environmental situation in the region where the person who received Mantoux lives;
- various diseases whose main symptom is epileptic seizures;
- a period of quarantine due to a pandemic of a virus (for example, a strain of influenza);
- low quality of the drug, use of an expired sample;
- improper storage and transportation of the sample;
- the test was carried out with violations - they used a non-disposable syringe, did not treat the skin where the injection was made with alcohol.
Thus, severe swelling at the site where tuberculin was injected, or, conversely, a complete absence of swelling, is not a guarantee that the child has Koch’s bacillus or not. To find out for sure, more in-depth research and analysis will be required. The Mantoux reaction is just one of the methods by which it is determined whether there is a dangerous pathology in the body.
Complications resulting from diagnosis
The Mantoux test is the most common method of anti-tuberculosis research. This is due to the high efficiency and safety of this examination method. But there are situations when the baby has increased susceptibility to tuberculin.
In this case, the body inadequately perceives the antigens that are present in the drug, as a result of which the necessary reaction of the immune system is absent. Serious consequences are not observed, but in each case, after the Mantoux test, the subject will get sick, sometimes in acute forms for a long period of time.
When properly manufactured and following the necessary storage recommendations, the drug does not pose a danger to the average person. However, among its components there may be factors that can cause allergies in some individuals.
During its development, the subject experiences the following symptoms:
- In case of mild allergic reactions to the constituent substances, the skin at the injection site may turn red, followed by itching.
- Allergies of moderate severity are characterized by inflammation of regional lymph nodes, an increase in body temperature of more than 38 degrees Celsius, general weakness, headaches and dizziness.
- Signs of severe manifestations of allergic processes include nausea, vomiting, a significant increase in temperature, disturbances of consciousness, difficulty breathing, and the development of kidney and heart failure.
The Mantoux test is one of the most reliable diagnostic methods that can be used to detect tuberculosis in the early stages of its development.
You should not refuse to conduct a tuberculin test without absolute contraindications. This will help prevent the spread of the disease and the development of severe complications in infected children.
Mantoux in children aged 4 years: norm and possible deviations
At four years old, the child undergoes the fourth Mantoux test. After vaccination, immunity accumulates significant strength by the age of one year, reaches its maximum value at the age of two, and begins to decline from the age of three.
A negative reaction to Mantoux is possible if the vaccination in the maternity hospital was not effective enough. If the scar on the forearm is small, about 2-3 mm, there is no significant strain on the immune system, protection ends by three to four years.
A negative (or questionable) reaction to the Mantoux test at four years of age is observed when the post-vaccination scar is up to five millimeters in size.
If the scar on the forearm is larger than 5-6 mm, protection against infection is more reliable. By the age of four, children show a weakly positive (papule 5-7 mm) or positive (papule 8-10 mm) Mantoux reaction.
Important! The diameter of the “button”, starting from the age of three, decreases by several millimeters at each check until the age of seven (normal). If at three years a papule measuring 10 mm was observed, at four years an infiltrate of about 8 mm would be normal.
If the swelling is still about a centimeter, the doctor will make a decision based on the child's overall health. If, when checked at age five, the papule remains the same size, the child will need to be monitored by a TB specialist. Most four-year-old children show an average result when tested - a papule of 5-7 mm. 10 mm is the maximum permissible value; with a diameter greater than this figure, it is recommended to conduct additional examinations
If at three years a papule measuring 10 mm was observed, at four years an infiltrate of about 8 mm would be normal. If the swelling is still about a centimeter, the doctor will make a decision based on the child's overall health. If, when checked at age five, the papule remains the same size, the child will need to be monitored by a TB specialist. Most four-year-old children show an average result when tested - a papule of 5-7 mm. 10 mm is the maximum permissible value; with a diameter greater than this figure, it is recommended to conduct additional examinations.
“Turn” is the main diagnostic principle that is used to assess the likelihood of infection at this age. If, compared to the result of the previous check, the papule does not decrease, but increases, then additional examination is necessary. If the “button” has increased by more than 6 millimeters over the course of a year, the child is diagnosed with “tuberculin test deviation”; observation by a phthisiatrician is mandatory.
Example. At the age of three, the diameter of the child’s papule was 5 mm (the size of the post-vaccination scar was 6 mm). The fourth check showed the size of the papule to be 15 mm. Over the course of a year, the reaction has increased by 10 mm, the likelihood of infection is high. Examination and treatment are necessary.
A hyperergic Mantoux reaction (17 mm or more) at four years of age also becomes a fairly accurate sign of possible infection. In addition to infection, a large “button” at this age occurs in the event of a severe allergic reaction of the body to chemicals, foods or medications. Infection with another, non-tuberculous mycobacterium is possible.
When assessing a sample from a four-year-old child, experts take into account not only the size of the infiltrate, but also additional signs of infection. The papule in an infected child usually festers, has a characteristic bright red color, and sometimes resembles an open wound.
When infected, the infiltrate has clear boundaries; after a week the tumor does not disappear, it becomes pigmented and turns brown. Sores and blisters appear around the injection site, and a bright red trail runs from it towards the elbow.
If the “button” is too large, but there are no additional signs, there is no need to worry in advance. A “false-positive” reaction caused by allergies or mechanical irritation is possible.
Classification
Mantu is performed starting from the age of one year, and is done annually until the age of fourteen. But cases cannot be ruled out when it becomes necessary to carry out the test twice a year and start doing this as early as six months.
Such factors include;
- HIV infection;
- absence of BCG in the maternity hospital;
- diabetes;
- long-term use of hormonal drugs;
- Chronical bronchitis.
Manta is distinguished:
- individual - carried out exclusively according to indications;
- mass - carried out immediately for a group of people. This type of manta is carried out in places with a high increase in incidence, in order to timely detect infected children.
Two types of tuberculin can be used:
- alttuberculin or also called Koch tuberculin, which consists of mycobacteria neutralized by heating, the problem is that it may contain impurities, which often leads to a false positive result;
- purified tuberculin - this type completely eliminates all kinds of impurities.
Preparation for the event
No special preparation is required for the test. It is advisable to come to the clinic in loose clothing that does not rub the injection site. You should first undergo an examination by a pediatrician. Urine and blood tests are prescribed if the doctor doubts the state of the immune system. If there is an allergy, the child is first given antihistamines. 1 week before the expected date, it is not recommended to introduce new foods into the children's diet.
How the sample is made
The child's mantoux is placed in the front of the forearm. 0.1 ml of tuberculin is injected intradermally with a disposable syringe. It is advisable to dress the child in clothes with short sleeves so that she cannot rub the papule. Do not cover the injection site with a plaster or bandage it. Such actions can lead to skin injury. The survey results will be distorted.
It is not recommended to lubricate the papule with brilliant green, iodine, hydrogen peroxide and other antiseptics. After checking the indicators, if the area is inflamed or festered, it can be treated using any means.
Complications and adverse reactions with the Mantoux test
Usually doctors do not like to talk about this out loud, so as not to disrupt the planned tuberculin diagnosis, but complications and side effects after the Mantoux reaction do exist.
The most common side effects include fever (body temperature rises to 400 C), headaches, vomiting, dizziness, itching in the papule area, and allergic conditions.
Also dangerous are lymphangitis and lymphadenitis, which are not uncommon in people with hypersensitivity to the injected substance.
You can find out where to go with your child in St. Petersburg from our article. You can find out how to explain to your child what sex is here.
How to treat diarrhea in a child, you can find out here
How and why Mantoux is made
After the BCG vaccination, the process of developing immunity begins in the baby’s body. In the first year of life, he will actually have to suffer from a local cutaneous form of the disease. Attenuated mycobacteria of bovine tuberculosis enter the body. After a month and a half, an infiltrate forms, which festers for six months, then a scar appears - evidence of the development of immunity.
It is the BCG vaccination that is a serious burden for the body, but no one would think of refusing vaccination: it provides immunity during primary infection and protects against severe forms of the disease (including meningitis).
Mantoux is a simple diagnostic procedure that forms a single diagnostic complex with BCG. The amount of the administered substance is minimal, the immune system does not receive any additional stress, and the state of health does not deteriorate.
Tuberculin does not contain living bacteria. Fragments of pathogen tissue have been repeatedly processed (both thermally and chemically) and do not pose any health hazard.
An aqueous solution of the drug is injected under the upper layer of the skin of the forearm in an amount of 0.1 mg.
Phenol, used as a preservative, is contained in each individual sample in an amount several times less than that which is released by the body itself daily during its life processes.
The reaction to tuberculin appears on the first day after the procedure. It is expressed by redness (hyperemia) and the appearance of a tumor. A compaction, an infiltrate that rises above the skin, is called a papule. It is the diameter of the papule that is the main indicator of the test result. The papule is created by active T-lymphocytes, which are concentrated at the site of infection from the nearest lymphatic ducts. If their number is large, the immune system is seriously strained.
Attention! The maximum tension of immunity in a child’s body after the first BCG vaccination is achieved by two to three years. The response to the Mantoux test at this age is most pronounced
Reaction results: photo
The results of the Mantoux test are assessed 72 hours after the injection.
Photo 1. Positive result of the reaction. At two years old this is the norm: the child has developed immunity.
Photo 2. Hyperergic reaction: the child is most likely infected or already sick with tuberculosis.
Using a special ruler, holding it perpendicular to the shoulder line, the doctor measures the diameter of the skin lump.
- If there are no traces of an injection, with slight redness without a tumor (or with a tumor of about a millimeter), the doctor states a “negative reaction” to the Mantoux test.
- A small infiltrate (from two to four millimeters), regardless of the size of the reddened area, is a “doubtful reaction” to a tuberculin test.
- A papule measuring half a centimeter or more is a positive result, a “positive reaction” to the Mantoux test.
- The size of a papule in children is 17 mm or more - an indicator of a “hyperergic reaction”, a sign of infection and disease.
Photo 3. An example of a dubious Mantoux test: the size of the papule does not exceed half a centimeter.
Nature and process of grafting
The test is administered by injecting a disposable syringe shallowly under the skin from the palm to the elbow from the inside on the surface of the child’s arm. Typically, such an injection is not too painful, so you need to talk to a child of a conscious age in advance so that he does not feel afraid of the vaccination.
After some time, a papule forms at the puncture site. After 72 hours, its diameter is measured with a ruler, and the obtained figures are used to determine the state of immunity and the activity of Koch’s bacillus in the body.
In order for the doctor to make a correct diagnosis, it is necessary to take certain precautions after the injection.
The injection site must be protected so that the size of the mantoux is true. Under no circumstances should it be wet. Therefore, showers and baths are canceled while waiting for the Mantoux reaction in a one-year-old child. You can wash your face, wash your legs and other parts of the body, but you need to be careful not to let water get into the grafting site.
You also need to avoid dirt and dust, so vigorous games in the sandbox are canceled for three days.
You should not scratch the papule or the area around it; you should avoid playing with pets so that their claws, tongue and fur do not get dirt into the skin puncture site. During these three days, until the doctor measures the red spot that represents the reaction, you need to take care of the child.
You should also not eat red vegetables and fruits, so as not to cause excessive redness, but you should not change your diet too much, so that this does not become a shock to the body and cause an unusual reaction to the vaccine.
Somewhere during the month when the vaccination should occur, there is no need to change the baby’s usual menu much. You just have to limit meat and dairy products a little. The rest of the menu should be in its normal state without sudden changes. Also, you should not put a band-aid on the injection site or apply anything on it.
If water accidentally gets on the papule, you need to honestly tell the doctor about it. If the red spot is large enough, the doctor may send you to a tuberculosis clinic for additional tests. To prevent this from happening, you must warn the doctor that it was not possible to protect the injection site. And then he will calculate the body’s reaction based on the diameter of the spot, taking into account the ingress of water.
After the doctor has examined, measured the spot and made conclusions, you can lubricate the hole from the injection with brilliant green, wait a little until it heals and then continue to lead a normal life for the baby. The Mantoux vaccination will not seriously affect his health.
The essence of the examination, interpretation of the result
Results are provided only 72 hours after the injection. Based on the size of the formation, the doctor makes a conclusion about the presence of the causative agent of the disease in the child’s body. At the same time, he necessarily takes into account the individual nuances of the response to the introduction of tuberculin.
Children are considered more susceptible to tuberculosis than adults. For this reason, their examination is very significant. The first vaccination is given to children aged 1 year. It is not advisable to use the Mantoux test before this age, since the hypersensitivity of the baby’s skin does not guarantee the accuracy of this type of examination.
The assessment of diagnostic results is directly determined by the size of the papule.
Measurements are carried out 72 years after the injection of tuberculin.
The answer could be:
- Negative. During this, specific compactions and hyperemia are not observed at the injection site, which indicates the absence of contact with disease antigens. It is possible that it could have taken place in the past with further suppression of the activity of the pathogen and its effect on the child’s body.
- Positive. In this case, the formed papule is the result of contact of the body with the causative agent of tuberculosis, during which specific lymphocytes accumulate in it to combat the pathology.
- Doubtful. The size of the compaction does not exceed 4 mm and slight hyperemia of the skin at the injection site is observed. In this case, it is recommended to repeat the test after a month. It is also worth taking an x-ray, where the doctor will be able to examine the condition of the child’s lungs using the resulting photo.
The following types of reaction are distinguished:
- mild form (5-9 mm);
- medium shape (10-14 mm);
- pronounced shape (15-16 mm);
- excessive development (17mm).
Deviations
If you are interested in what Mantoux looks like for tuberculosis, you need to understand that the body’s reaction to the introduction of tuberculin can be weakly positive, moderately or strongly expressed, and doubtful.
What do you think are the most important factors when choosing a medical facility? Poll Options are limited because JavaScript is disabled in your browser.
Positive reaction
If a person is sick with tuberculosis, after the injection a papule is formed, the diameter of which is more than 5 mm. There is thickening, redness and swelling of the skin, itching may be present, and allergies may develop.
With a sharply positive reaction, the size of the plaque exceeds 15 mm, severe swelling appears at the injection site, the lymph nodes become enlarged, foci of inflammation and purulent formations around the papule are observed.
A questionable Mantoux reaction is characterized by the presence of a neoplasm, the size of which does not exceed 4 mm, slight redness of the skin and the absence of compaction.
False positive result
A false positive result of tuberculin diagnostics is observed after the administration of tuberculin in the presence of contraindications to the test.
These include:
- skin pathologies;
- allergies of various origins;
- exacerbation of an infectious or bacterial disease at the time of the test;
- recently completed preventive vaccinations against tuberculosis and polio;
- epilepsy;
- taking certain medications.
A false positive reaction is characterized by the appearance of large papules, severe swelling and redness of the skin. Most often it occurs as a result of improper care of the injection site: scratching, contact with water, treating the skin with medications, or applying an adhesive plaster.
In cases where the allergy test has deviations from the norm, or the reaction raises doubts among the therapist, additional studies are prescribed, and the patient is referred to a specialist doctor.
Correctness of assessment
Parents are often interested in what size Mantoux is considered normal for children. When measuring a sample at home, they may make some mistakes and get some scary results. The medical specialist uses a tuberculin ruler, which is completely transparent. It is applied to the arm along the line where the puncture site is located. Sometimes you can evaluate the result visually. We are talking about cases when it is already obvious that the “button” is tiny.
If there is still a need to use a special ruler, the doctor measures only the location of the lump, without touching the reddened area. Unfortunately, there are now frequent cases where false positive results are observed. The most common mistake is not taking into account the baby’s age. The younger the child, the larger the diameter the lump can reach after the injection
It is important that as you grow older, the size of the papule decreases
If you see a large compaction after Mantoux, you should not panic. It is possible that this is an allergic reaction to tuberculin. If the diameter is really large, then most likely you will have to undergo repeated tests. Final conclusions are made only after several samples.
There may be many reasons for Mantoux’s positive reaction. One of them is poor ecology. Toxic emissions from enterprises poison the body, which provokes local inflammation. It is they who can cause a pronounced positive reaction and frighten parents.
Wanting to understand how many millimeters is the Mantoux norm for 1 year, adults should ask their doctor about this or look at a special table. You should not worry too much about large sizes until repeated studies have been completed.
First try
Many people wonder when they give the first Mantoux test to a one-year-old child? If a newborn is vaccinated with BCG within a week after birth, Mantoux should be mandatory when he turns one year old. This first test is also important in that it enhances the development of immunity to the causative agent of tuberculosis pathology.
But the main goal of Mantoux for a child’s year is to control the BCG vaccination. If for any reason the vaccine was not administered after birth, Mantoux is given once every 6 months. Their frequency increases if among those who come into contact with the little one there are those who suffer from tuberculosis.
The Mantoux test is characterized by the introduction of a solution with neutralized fragments of the causative agent of Koch's disease subcutaneously in a small dose. The place where the Mantoux test is injected with a special syringe is the inner side of the forearm. A swelling forms around the injected dose of tuberculin - a painless, button-like, compacted papule. For one-year-old children, the optimal size of the Mantoux reaction papule is 10 mm. This size of the Mantoux reaction is considered normal after BCG vaccination and confirms that there has already been contact with mycobacteria and the body has responded to their appearance.
We recommend reading! Follow the link: Normal sizes for children result on Mantoux
Assessing the dynamics of results
Thanks to statistics, we can safely say that during the first testing, more than half of children have a positive Mantoux test result. The rest of the contingent is registered as doubtful or negative. It is believed that at three years of age children experience the greatest positive effect from tuberculin testing, and can reach 15 mm.
However, after 4 years, the immunity formed by the BCG vaccination gradually fades, and a papule measuring > 13 mm may indicate the presence of the disease.
When children reach the age of seven, a significant number of them will subsequently have doubtful or negative results of the Mantoux test.