Abdominal pain (in the abdomen) is quite common in both adults and children. Many people try to associate them with some food or drink consumed the day before. This reason for the development of events also occurs, but not always.
Abdominal pain can also be caused by more serious factors. One of them is that the lymph nodes in the abdominal cavity are enlarged. In children and adults, the symptoms of this pathology are approximately the same. The difference is that a small patient sometimes cannot explain clearly enough what is wrong with him. Concerned parents may attribute his complaints of abdominal pain to a dozen reasons that have no place in this case. Some even begin to self-medicate, thereby aggravating the baby’s condition.
The article answers questions about why a child may have enlarged lymph nodes in the abdominal cavity, how to differentiate this pathology from other problems with the gastrointestinal tract, and what treatment is required.
Lymph nodes
First, let's take a brief overview of these small but very important organs. The lymph node is a natural filter that helps get rid of all kinds of pathogenic agents that have entered the body.
Its structure is quite complex. In general terms, a lymph node is a small (up to 50 mm maximum) round, bean-shaped or oval-shaped sac, to which lymph vessels (several incoming and one outgoing) are suitable. The outside of the “bag” is covered with a membrane consisting of connective tissue. Inside it is filled with the so-called stroma, made up of reticular fibers. A large number of lymphocytes of various types are concentrated in the space between them.
Lymph, slowly seeping through the reticular fibers, as if through a sieve, is cleared of all sorts of pathogenic agents that it has “collected” in the body (bacteria, viruses, protozoa, and so on). If a person has any disease, too many harmful elements enter the lymph. The lymph nodes can no longer cope with their task and become inflamed. This symptom always indicates the presence of some pathogenic process in the body.
While examining the patient, the doctor discovers that his lymph nodes are enlarged. In the abdominal cavity of a child and an adult, there are about 600 of them. They are located not one by one, but in groups, vaguely similar to a bunch of grapes. Lymph nodes are concentrated in the peritoneum where blood and lymph vessels pass - near the stomach, liver, spleen, mesentery, intestines.
Causes of lymph node hyperplasia
When characterizing the causes of lymph node hyperplasia, it is necessary to clarify that lymphoid or lymphatic tissue (consisting of reticuloendothelial cells, T-lymphocytes, B-lymphocytes, lymphatic follicles, macrophages, dendrites, lymphoblasts, mast cells, etc.) is located not only in the parenchyma of the organs of the lymphatic system : regional lymph nodes, spleen, thymus glands, pharyngeal tonsils. This tissue is also present in the bone marrow, in the mucous membranes of the respiratory system, gastrointestinal tract and urinary tract. And if there is a focus of chronic inflammation in any organ, accumulations of lymphoid tissue cells appear there too - to protect the body from the infection attacking it.
But we are interested in the regional lymph nodes, which ensure the production of lymphocytes and antibodies, filtering lymph and regulating its flow from organs. Today, the causes of lymph node hyperplasia are considered as the reasons for their enlargement, which is an immune response to any pathological process that makes changes both in the dynamics of tissue metabolism of the lymph node and in the ratio of certain cells. For example, in response to genetically distinct cells (antigens) in a lymph node, the production of lymphocytes and mononuclear phagocytes (macrophages) increases; When bacteria and microbes enter the lymph nodes, their waste products and neutralized toxins accumulate. And in the case of oncology, hyperplasia of the lymph nodes can involve any of their cells in the pathological process of proliferation. This causes an increase in size, change in shape and structure of the fibrous capsule of the lymph node. Moreover, the tissues of the lymph nodes can grow beyond the capsule, and in the case of metastases from other organs, they can be replaced by their malignant cells.
Based on this, lymph node hyperplasia can be of infectious, reactive or malignant origin.
[16], [17], [18], [19], [20], [21], [22], [23], [24], [25]
Hyperplasia of lymph nodes of infectious etiology
Hyperplasia of the lymph nodes (in the sense of an increase in their size) is a response to infection in diseases such as lymphadenitis caused by strepto- or staphylococci, rubella, chicken pox, infectious hepatitis, felinosis (cat scratch disease); tuberculosis, HIV, infectious mononucleosis, cytomegaly, tularemia, brucellosis, chlamydia, syphilis, actinomycosis, leptospirosis, toxoplasmosis.
With nonspecific lymphadenitis, depending on the location, hyperplasia of the lymph nodes in the neck, lower jaw or axillary lymph nodes is observed. Enlargement of the axillary lymph nodes has been noted with mastitis, inflammation of the joints and muscle tissue of the upper extremities, brucellosis, felinosis, etc.
Inflammatory processes in the oral cavity and nasopharynx (with actinomycosis, caries, chronic tonsillitis, pharyngitis, bronchitis, etc.) are characterized by hyperplasia of the submandibular, postauricular, preglottic and retropharyngeal lymph nodes. And with infectious mononucleosis, only the cervical lymph nodes become enlarged.
In the case of rubella, toxoplasmosis, tuberculosis, as well as syphilis, doctors note hyperplasia of the cervical lymph nodes. In addition, the symptoms of tuberculosis include hyperplasia of the intrathoracic and mediastinal lymph nodes. At the same time, healthy cells of lymphoid tissue are gradually displaced in the lymph nodes by necrotic masses of a caseous nature.
Hyperplasia of the mesenteric lymph nodes is also characteristic of tuberculosis. In addition, a significant increase in the lymph nodes of the mesenteric section of the small intestine occurs due to damage by the gram-negative bacterium Francisella tularensis, which causes tularemia, an acute infectious disease transmitted by rodents and arthropods.
Hyperplasia of the inguinal lymph nodes is noted by doctors in infectious mononucleosis, toxoplasmosis, brucellosis and actinomycosis, as well as in all genital infections and HIV.
Causes of inflammation
Based on the above, you can easily understand why the lymph nodes in the abdominal cavity of a child are enlarged. In general, this condition is called lymphadenopathy, and inflammation of the lymph nodes specifically in the mesentery is called mesadenitis. It is caused by the following reasons:
- Any bacterial infection (streptococci, staphylococci, salmonella, tuberculosis, E. coli).
- Any viral infection (enterovirus, herpes).
- Worm infestation.
- Fungal infection.
- In rare cases, toxic poisoning.
Pathogenic elements enter the lymph nodes with blood, lymph, and also through the lumen of the tract (worms).
Sometimes the infection seeps into the tissue of the lymph nodes directly from the intestines.
What is mesadenitis?
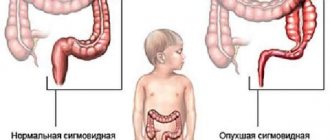
The disease mesadenitis is inflammation of the lymph nodes located in the mesentery (the abdominal fold of the intestine, through which the small intestine is attached to the wall of the abdomen).
As you know, the abdominal cavity contains about 500 lymph nodes, which do not allow infections to spread and take all the “fire upon themselves.”
Thus, inflammation and even suppuration may occur in the nodes. This disease is more common in children and adolescents.
What diseases cause mesadenitis?
Most often, a child's lymph nodes in the abdominal cavity are enlarged due to the development of diseases in the organs near which they are located. Among them:
- Helminthiases.
- Brucellosis.
- Hepatitis.
- Trichinosis.
- Ascariasis.
- Echinococcosis.
- Salmonellosis.
- Mononucleosis.
But often the lymph nodes in the child’s abdominal cavity are enlarged due to infectious diseases not related to the gastrointestinal tract. Among them:
- Flu.
- ARVI.
- Tuberculosis.
- Pneumonia.
- Herpes.
- Lupus erythematosus.
The following can also cause enlargement of lymph nodes in the peritoneum:
- AIDS.
- Syphilis.
- Malignant formations (metastasis in the gastrointestinal tract).
These ailments are mainly observed in adults, but they also occur in children.
What factors can cause mesadenitis?
Medical practice has confirmed that the disease is the result of inflammation in the intestines. Thus, the causes of mesadenitis can be appendicitis and infections (gastroenteritis, enteroviruses, salmonellosis, yersinia, E. coli, campylobacter), where the infection spreads enterogenously.
There are many examples when mesenteric lymphadenitis developed after a disease of the nasopharynx and respiratory canals (tuberculosis, pneumonia, acute respiratory infections, tonsillitis, infectious mononucleosis and others). In these examples, the infection enters the mesenteric lymph nodes through the blood. Although cases cannot be ruled out when it ends up in the intestines through sputum entering it.
Classifications
A disease in which the lymph nodes in the child’s abdomen are enlarged can occur suddenly or last for years. Depending on the nature of the flow, the following forms are distinguished:
- Spicy.
- Chronic.
Depending on the number of enlarged lymph nodes, the following forms are distinguished:
- Local (affects one node).
- Regional (more than one lymph node is enlarged).
- Generalized (the entire peritoneum is affected).
Based on etiology, the following forms are distinguished:
- Primary (occurs as an independent disease).
- Secondary (occurs against the background of infections in the gastrointestinal tract, respiratory tract and others).
Types of mesadenitis
Mesenteric lymphadenitis occurs in two forms.
Modern medicine calls them as:
- acute form (acute nonspecific mesadenitis). A characteristic feature of this form is the presence of cramping pain;
- chronic form (chronic mesadenitis). Its symptom is prolonged pain.
This disease is divided into several types.
The species determines the pathogen:
- Nonspecific mesadenitis is caused by pathogens such as staphylococcus, E. coli and viruses; pathogens exhibit activity when the body’s immunity decreases and some other factors. The nonspecific type is divided into simple and purulent.
- Specific mesadenitis has the following varieties: Tuberculous (appears due to the effect of the tuberculosis bacillus on the body).
- Pseudotuberculous.
- Yersinia (appears under the influence of the microbacterium Yersinia).
Types of mesadenitis differ in the way the infection enters the mesentery:
- The infection comes from another diseased organ (enteral route of penetration).
- The bacterium enters through the blood (lymph) from the damaged area (respiratory organs, appendicitis).
Enlarged lymph nodes in the abdominal cavity in a child: symptoms
In children, the acute form of the pathology is more often diagnosed. It is characterized by a violent manifestation. Its manifestations are as follows:
- A sharp increase in temperature.
- Complaints of abdominal pain (paroxysmal, acute, localized or vague).
- Children's anxiety, tearfulness, moodiness.
- Vomit.
- Complaints of nausea.
- Diarrhea (this symptom often makes parents think that the child has eaten something wrong).
- Palpation of enlarged lymph nodes.
In the chronic form, all these symptoms are less pronounced. Also, with a long course of the disease, in which the child has enlarged lymph nodes in the abdominal cavity, the stomach hurts in the navel area or the pain spreads to the lower sections. Sometimes children have difficulty explaining exactly where it hurts, since the unpleasant sensations are vague and palpable throughout the entire abdominal area.
What symptoms are characteristic of mesadenitis?
Each form of the disease manifests itself with its own symptoms of mesadenitis.
The acute form corresponds to the following symptoms:
- unexpected and acute pain in the solar plexus, high fever, feeling of nausea and vomiting;
- it is impossible to say where the source of pain is, since the entire gastrointestinal tract hurts;
- the pain feels dull, aching, constant and may intensify with the development of the inflammatory process;
- increased pain will be observed from body movements (if the lymph nodes in the child’s intestines begin to fester);
- there is an intestinal disorder (diarrhea), characteristic of colitis, gastritis and other gastrointestinal diseases;
- there is a feeling of dryness in the mouth, there is a desire to drink;
- temperature rises to 39 degrees;
- there are surges in blood pressure;
- heart rate and breathing rate increase.
The chronic form of mesadenitis has mild symptoms.
The pain has no specific localization, is distributed throughout the abdominal area and intensifies with heavy physical exertion and sudden body movements.
Pain may persist for weeks or months.
The tuberculosis form of the disease manifests itself in mild abdominal pain, weight loss, and an increase in body temperature to 37.5 degrees.
Sometimes there is a cough.
Tuberculous mesadenitis
According to medical statistics, enlarged lymph nodes in the peritoneum are more often observed in children aged 6-14 years. In view of this, the occurrence of such a condition due to infection with Koch bacilli (tuberculosis form) is diagnosed in rare cases. It occurs due to the fact that pathogenic bacilli from the lungs enter the lymph, and with it are carried into the lymph nodes of the peritoneum. In this case, the following signs of inflammation are observed:
- The child becomes indifferent to games and lethargic.
- Lost appetite.
- There is weight loss.
- I am worried about a cough that cannot be treated with classical methods.
- The skin becomes pale.
- The temperature stays between 37.1-37.3 degrees Celsius.
If the lymph nodes in the child’s abdominal cavity are enlarged precisely because of suspected tuberculosis, what should be done? First of all, you need to perform a test for the presence of Koch bacilli in the blood. It is better known as the Mantoux reaction.
Nowadays, you can catch tuberculosis anywhere - in transport, in child care institutions, during public events. At risk are children whose family members suffer from this disease, as well as those children who have undergone any disease or surgery after which their immunity has decreased. Parents of such children should immediately consult a doctor if the child develops the above symptoms.
Is there a diet for mesadenitis?
When treating the above-described illness, as well as other gastrointestinal diseases, a diet is prescribed for mesadenitis in children (table No. 5).
The main nutritional requirement is to eat food frequently (every 3-4 hours) in small portions.
It is forbidden to eat before bedtime, but drinking is allowed without restrictions.
Food should be cooked in the oven or boiled.
For this disease, the following products are prohibited:
- fatty meat and fish products, lard, all fried foods;
- fatty meat broths;
- tea, coffee, chocolate;
- hot, salty, smoked, spicy food;
- semi-finished products, eggs, canned food, mushrooms;
- ice cream, buns, cakes;
- radishes, sorrel.
There are a number of products approved for consumption.
These include:
- salads, vegetable soups, milk soups, lean meat broths;
- crumbly porridge;
- compote, tea with sugar, honey, tomato juice;
- low-fat cottage cheese and sour cream.
The difference between mesadenitis and appendicitis, gastritis and other gastrointestinal diseases
Symptoms such as abdominal pain, nausea, loss of appetite, weakness, fatigue, stool upset (diarrhea/constipation) are observed in most diseases of the gastrointestinal tract. Therefore, it is almost impossible to make a diagnosis based on clinical manifestations alone. This is especially true if the patient is a small child who cannot really explain anything. The following characteristic signs can help in making a preliminary diagnosis:
- With gastritis, discomfort intensifies after eating. Also (in addition to the signs of mesadenitis listed above), patients may experience flatulence, heartburn, and belching. With inflammation of the lymph nodes, there are no such symptoms.
- With appendicitis, sharp pain is most often localized in the right side of the peritoneum (in the iliac region). Palpation of this area causes muscle tension and increased pain. Another sign is that the temperature in the rectal area differs from that measured in the armpit by 1 or more degrees. There are a number of syndromes by which an experienced doctor can distinguish appendicitis from inflammation of the lymph nodes.
- With shigellosis (dysentery), the symptoms are very similar to the manifestation of the acute form of mesadenitis. The difference is that in the first case, patients experience repeated diarrhea, accompanied by the appearance of mucus and blood in the stool.
ethnoscience
To restore intestinal function when inflammation of the lymph nodes in the abdomen is detected, traditional medicine and doctors recommend the following decoctions:
- A decoction of blackberries (roots) has a good anti-inflammatory, antipyretic and bactericidal effect. The crushed roots of the plant (10 g) are poured with boiling water, boiled for 10 minutes and left for 3 hours. Every 2 hours, drink 1 tbsp of the decoction. l.
- Chamomile infusion (flowers) exhibits strong antispasmodic, carminative and anti-inflammatory effects. For one glass of boiling water you will need 1 tsp. medicinal chamomile flowers. The infusion is kept in a thermos for 3 hours, after which it is decanted. Take 4 times throughout the day, 1/4 cup.
- A decoction of cumin seeds. One glass of boiling water is poured into 1 tbsp. l. seeds and boil for 30 minutes. Take 2 tbsp before meals. l. decoction 4 times throughout the day.
Diagnostics
All parents should remember that it is necessary to immediately call an ambulance for their child if they experience:
- A sharp increase in temperature.
- Vomit.
- Complaints of abdominal pain.
- Diarrhea.
Self-medication in such cases is unacceptable, since drugs “for diarrhea” or “for fever” can reduce or temporarily completely eliminate symptoms, which will affect the diagnosis. As a result, the child may die.
The doctor first conducts a clinical examination of the patient, performs palpation of the peritoneum, and various medical tests that help to exclude certain gastrointestinal diseases.
In a medical institution, the child is required to perform a number of tests:
- Total blood (determines the level of hemoglobin and leukocytes).
- Biochemical blood (detects the presence of hepatitis viruses and other pathogenic microorganisms).
- Total urine (shows the number of leukocytes in it).
- Coprogram (this analysis detects the presence/absence of blood in the stool).
- Mantoux test.
- Feces on worm eggs.
These studies help doctors rule out appendicitis, hepatitis, helminthiasis, and inflammation of the gastrointestinal tract in the patient.
How is the disease determined by diagnosis?
The diagnosis of the disease is determined by the following methods:
- the patient or his parents are asked about their health, past illnesses, etc.;
- The patient is examined: skin color is examined (patients tend to be pale), tongue (the patient has white spots), pulse (the patient usually has an increased frequency), body temperature (with mesodenitis it is elevated), breathing (the frequency is increased).
Palpation of the abdomen confirms pain near the navel and in the right lower abdomen.
There are no signs of tension in the abdominal cavity.
These factors confirm inflammation of the intestinal lymph nodes and distinguish it from appendicitis.
Sometimes only palpation reveals enlarged lymph nodes, and pressing on them provokes vomiting.
Additional methods for diagnosing mesadenitis:
- Blood test for leukocytes and red blood cells.
- Biochemistry analysis to identify liver (kidney) pathologies.
- Analysis of venous blood and feces to detect helminthiasis.
- Ultrasound examination, which reveals an increase in mesenteric nodes (more than 5 mm).
- Colonoscopy, abdominal x-ray, esophagogastroduodenoscopy.
- Laparoscopy, using an incision in the abdomen and a special camera, allows you to examine the intestinal cavity from the inside and simultaneously perform micro-surgery.
It is important to understand that ultrasound examination data alone is not enough, since in children a node diameter of 5 mm is an acceptable norm.
Therapy methods
If a child has enlarged lymph nodes in the abdominal cavity, treatment can be carried out at home or in a hospital. This is determined by the doctor, depending on the severity of the pathological process. In some cases, all treatment consists of bed rest, eliminating the underlying disease (for example, influenza) and taking vitamins to strengthen the immune system. After recovery, all systems and organs gradually return to normal. This also applies to lymph nodes.
In other cases, drug therapy is carried out, which is primarily aimed at eliminating the causes of the pathology, that is, the underlying disease.
To relieve inflammatory processes in the lymph nodes, the following are prescribed:
- "Tempalgin".
- "Papaverine".
- "Drotaverine".
- "Ketorolac".
If inflammation of the lymph nodes is caused by intoxication, infusion solutions such as Neocompensan and its analogues are prescribed.
Children may also be prescribed physiotherapy, including compresses, mud applications, and ultraviolet radiation.
Both children and adults, when enlarged lymph nodes are detected, are required to be prescribed a diet (table No. 5). She excludes from the diet all foods that promote active digestion (spicy, spicy, salty, etc.), fresh bread, fried, smoked, hot seasonings.
How is diagnosis carried out?
A comprehensive study will help to find out the cause of the development of pathology
Any diagnosis begins with an external examination of the patient and a history study. Just by the appearance of the lymph nodes, an experienced doctor can predict the development of a particular disease.
To clarify the diagnosis, the patient is sent for a comprehensive examination, which includes the following procedures:
- general and biochemical blood tests;
- immunological research;
- general urine analysis;
- blood test for the presence of tumor cell markers;
- throat swab;
- Wasserman reaction, which involves conducting a serological test.
The Mantoux test can be used as an additional procedure. Taken together, all the above procedures make it possible not only to determine the specific pathogen of the disease, but also to obtain information about its activity.
To obtain more accurate data regarding the localization of the pathological focus, the following instrumental diagnostic methods are used:
- Ultrasound;
- plain radiography of the chest organs;
- lymph node biopsy, suggesting subsequent laboratory tests.
Instrumental studies are necessary to determine the structure of the affected node and identify the cause of the development of the inflammatory process. They allow you to select the right treatment and predict the possible course of the disease.
The basis of diagnosis in this case is histological examination (a tissue sample is obtained by biopsy). This technique allows you to obtain the most reliable data about the nature of the pathological process.
Complications
If you do not consult a doctor immediately as soon as the child begins to complain of abdominal pain, accompanied by vomiting, diarrhea and high fever, and instead self-medicate, then mesodenitis and lymphadenopathy, which are not considered life-threatening, can lead to serious complications:
- Suppuration of inflamed lymph nodes. In this case, the patient’s condition worsens significantly: abdominal pain intensifies, the temperature rises (up to 40 degrees), and symptoms of severe intoxication appear.
- Peritonitis (inflammation of the peritoneum).
- Localized mesadenitis develops into generalized (throughout the body).
- Sepsis. This is one of the most dangerous complications that occurs when pathogenic microorganisms enter the blood.
Which doctor should I contact?
If your lymph nodes are enlarged, you should make an appointment with a therapist. Based on the patient’s complaints and the results of the initial examination, he can refer the patient to the following specialists:
- Dermatologist - if damage to the skin or pustular elements is noticed above the nodes.
- Otolaryngologist. She examines patients with hyperplasia of the submandibular lymph nodes, as well as lesions of the cervical and parotid nodes.
- Oncologist. If tumor markers are detected in the blood, consultation with this specialist is necessary.
- Surgeon. Examines patients in whom the most severe stages of the disease have been identified. This specialist also deals with surgical treatment of lymph node hyperplasia.
The child has enlarged lymph nodes in the abdominal cavity and spleen
In the human peritoneum, in its upper left part, there is a small organ called the spleen. In the fetus it is a hematopoietic organ. In the newborn baby and throughout the rest of a person’s life, the spleen performs many important functions, including lymphopoiesis. This means that lymphocytes and antibodies are produced in it. It also serves, like lymph nodes, as a natural filter that retains pathogenic agents (bacteria, viruses, foreign particles).
If a child has a stomach ache, ultrasound shows that the lymph nodes in the abdominal cavity and the spleen are enlarged - this is a sign that an inflammatory process is occurring in the body caused by infection with pathogenic microbes or protozoa.
However, an enlarged spleen can mean another unpleasant disease - lymphoma. It is diagnosed in people of any age, including children. Other names of the pathology are lymphogranulomatosis, Hodgkin's disease.
Its characteristic features are that in the first stages, enlarged lymph nodes practically do not manifest themselves at all and are discovered only by chance, for example, during an ultrasound of the abdominal cavity. They can spontaneously increase and decrease without causing any discomfort to the patient. As the disease progresses, symptoms such as fever, weight loss, refusal to eat, night sweats, and abdominal pain appear. Inflamed lymph nodes and the spleen stop performing their main function - protection against microbes. Therefore, people with this pathology have a sharply reduced immunity.
The cause of an enlarged spleen is the presence of the Epstein-Barr virus (herpes 4) in the blood. It is found in approximately 50% of children over 5 years of age, but not everyone gets lymphoma. Provoking factors include conditions that reduce immunity (diseases, surgeries, stress, poor nutrition) and genetic predisposition.
Treatment methods depend on the degree of development of the disease. In the early stages, antiviral therapy is prescribed using the drugs Valacyclovir, Ganciclovir and their analogues. If indicated, surgery may be performed to remove the spleen.
Symptoms of acute mesadenitis in a child
The signs of this disease are quite vague and if a child is admitted to the inpatient department in unsatisfactory health, there is a high probability that the doctor examining the young patient will not be able to immediately recognize the presence of mesadenitis.
Therefore, it is necessary to pay special attention to the following list of symptoms indicating inflammation of the abdominal lymph nodes:
- acute pain inside the abdomen, which resembles a spasm and forces the child to take a horizontal position with the legs tucked to the chest;
- body temperature rises to 38-39 degrees Celsius;
- fever and increased sweating;
- general physical weakness, drowsiness, headache;
- loss of appetite with complete or partial refusal to eat;
- nausea, vomiting and stool upset, manifested in liquid diarrhea or prolonged constipation.
During palpation of the surface of the abdomen in the circumference of the navel, you can feel dense tubercles, which have different sizes, but are located next to each other. These are clear signs that the child is developing the initial stage of mesadenitis.
Mesadenitis
Mesadenitis
– inflammatory disease of the lymph nodes of the mesentery of the small intestine. The disease manifests itself as intense abdominal pain of various localizations, which intensifies with exercise, increased body temperature, tachycardia, shortness of breath, nausea, and diarrhea.
To confirm the diagnosis, it is necessary to conduct a surgical examination, laboratory tests, ultrasound and MRI of the abdominal cavity. In controversial situations, diagnostic laparoscopy is performed. Treatment involves the prescription of dietary nutrition, antibiotics, painkillers and parenteral detoxification solutions.
When suppuration occurs, abscesses are opened and the abdominal cavity is sanitized.
I88.0
Nonspecific mesenteric lymphadenitis
Mesadenitis (mesenteric lymphadenitis) is an inflammation of the lymph nodes located in the fold of the peritoneum, the main function of which is to suspend and attach the small intestine to the posterior wall of the abdomen. There are about 600 lymph nodes in the abdominal cavity, which perform a protective function and prevent the development of infection.
The prevalence of mesadenitis among acute surgical pathologies is 12%. The disease mainly affects children and young people of asthenic physique between the ages of 10 and 25 years. Females are somewhat more likely to suffer from this pathology.
The seasonality of the disease is noted: the number of patients increases in the autumn-winter period, when the number of patients with ARVI increases.
Mesadenitis
The disease develops in the presence of a primary focus of inflammation in the appendix, intestines, bronchi and other organs. Lymphogenous, hematogenous or enteral (through the intestinal lumen) the infection enters the lymph nodes of the mesentery, where pathogenic microorganisms multiply. The following pathogens can cause the formation of mesadenitis:
- Viruses
. Inflammatory lesions of the mesenteric lymph nodes can occur secondary to a viral infection of the respiratory tract, genitourinary system and gastrointestinal tract. Most often, mesenteric lymphadenitis is a consequence of adenoviral tonsillitis, pharyngitis, conjunctivitis, cystitis, enterovirus intestinal damage, infectious mononucleosis caused by the Epstein-Barr virus. - Bacteria
. The causative agents of mesadenitis can be both opportunistic microorganisms (staphylococci, streptococci, E. coli) - representatives of the normal flora of the mucous membrane of the gastrointestinal tract, nasopharynx, and pathogenic species of bacteria. Inflammation of the mesenteric lymph nodes can be observed with salmonellosis, campylobacteriosis, yersiniosis, generalization of the infectious process with tuberculosis of the bronchi, lungs, bones and joints, etc.
Predisposing factors to the development of mesadenitis are decreased immunity and concomitant inflammatory lesions of the gastrointestinal tract. The predominant damage to children and adolescents is associated with imperfections of the immune and digestive systems, frequent food poisoning and ARVI.
The mesenteric lymph nodes are a barrier to the penetration of infection from the intestines and internal organs into the abdominal space. When a primary inflammatory focus exists (in the intestines, upper respiratory tract), infectious agents enter the lymph nodes by lymphogenous, enterogenous or hematogenous routes.
In the presence of predisposing factors, the number of pathogenic microorganisms increases. Swelling and hyperemia of the mesentery occurs. Lymph nodes, mainly in the area of the ileocecal angle, have a soft consistency and red color.
When the lymph nodes suppurate, an infiltrate with purulent melting and areas of necrosis is formed. Generalization of the infectious-inflammatory process is accompanied by damage to the adipose tissue of the mesentery.
Histological examination reveals leukocyte infiltration and lymphoid hyperplasia of the nodes, thickening and swelling of the capsule. Depending on the severity of mesadenitis, a serous or serous-purulent effusion forms in the abdominal cavity.
The disease causes damage to both individual lymph nodes and the whole group. According to the pathological process, acute and chronic mesadenitis are distinguished.
Acute pathology is accompanied by sudden development and vivid symptoms. The chronic course of the disease has a blurred clinical picture for a long time.
Depending on the type of pathogen, the following types of mesadenitis are distinguished:
1. Non-specific
. It is formed when viruses or bacteria migrate from the main source of infection in the body. Nonspecific mesadenitis can be simple and purulent.
2. Specific
. It is formed under the influence of Koch's bacillus (Mycobacterium tuberculosis) or Yersinia bacteria.
The acute form of the disease is characterized by a sudden onset and rapid development of symptoms. Prolonged cramping pain occurs in the umbilical region or in the upper abdomen. In some cases, patients cannot indicate the exact location of the pain.
Intense pain is gradually replaced by dull and moderate soreness, which intensifies with a sudden change of location or coughing. The disease is manifested by fever, increased heart rate (up to 110-120 beats per minute) and respiratory movements (25-35 per minute). Dyspeptic disorders increase: nausea, dry mouth, diarrhea, and single vomiting appear.
Sometimes the disease is accompanied by catarrhal symptoms (runny nose, cough, hyperemia of the pharynx), herpes on the lips, wings of the nose.
With the formation of purulent mesadenitis, the intensity of pain decreases, intoxication of the body increases, and the patient’s general condition worsens. The chronic course of the disease is characterized by mild symptoms. The pain is mild, without specific localization, is short-term in nature and intensifies with physical activity.
Periodically, short-term nausea, constipation or loose stools occur. Tuberculous mesenteric lymphadenitis is accompanied by a gradual increase in symptoms. Severe intoxication is noted with the development of weakness, apathy, pallor of the skin with the appearance of a sallow skin tone, and low-grade fever.
The pain is aching, short-lived, and has no clear localization.
The progression of the disease can cause suppuration of the lymph node, the formation of an abscess and the development of purulent mesadenitis. The prolonged course of the purulent process leads to the melting and breakthrough of the abscess with the release of the contents of the lymph node into the abdominal cavity. As a result, peritonitis develops.
When pathogenic microorganisms enter the blood, a serious complication occurs - sepsis, which can lead to death. The long course of mesenteric lymphadenitis contributes to the formation of adhesive disease of the abdominal organs. Adhesions and cords of the peritoneum can lead to strangulation intestinal obstruction.
In rare cases, the process generalizes with the development of extensive inflammation of the body's lymph nodes.
The nonspecific clinical picture causes significant difficulties in diagnosing the disease. In order not to miss the development of serious complications, diagnostic procedures are recommended to be carried out in full. Diagnosis of mesenteric lymphadenitis includes:
- Examination by a surgeon
. Palpation of the abdomen reveals dense, tuberous formations of various locations. Positive symptoms are noted: McFadden (pain along the outer edge of the rectus abdominis muscle), Klein (migration of pain from right to left when the patient turns from the back to the left side), Sternberg (pain when pressing along the line connecting the left hypochondrium with the right iliac region). - Ultrasound of the abdominal cavity
. This method allows you to determine dense enlarged lymph nodes and increased echogenicity in the mesentery. Examination of the gallbladder, pancreas, and spleen excludes the presence of diseases with similar symptoms (acute pancreatitis, cholecystitis). - MRI of the abdominal cavity
. It is the most informative and modern diagnostic method. Allows you to determine the exact location, size and number of affected lymph nodes. This method helps to visualize changes in the gastrointestinal tract and other abdominal organs. - Laboratory research
. The CBC shows leukocytosis and an increase in ESR. A bacterial infection is characterized by a shift in the leukocyte formula to the left, neutrophilia; for viral – lymphocytosis. Blood culture for sterility allows you to determine the pathogen circulating in the blood. If the tuberculosis nature of the disease is suspected, a Mantoux test and intradermal diaskintest are performed. To determine the pathogen or the presence of antibodies to it, specific serological methods of blood testing are used (ELISA, RSK, etc.). - Diagnostic laparoscopy
. It is performed when non-invasive diagnostic methods are insufficiently informative. The method allows you to visualize the affected lymph nodes, determine their number and location, and examine other abdominal organs to exclude concomitant pathology and carry out differential diagnosis. To establish a final diagnosis, material (lymph node) is collected intraoperatively for histological examination.
CT scan of the abdominal organs. An increase in the size and number of lymph nodes in the root of the mesentery of the small intestine against the background of its pronounced compaction
Differential diagnosis
Differential diagnosis of mesadenitis is carried out with acute surgical pathology of the abdominal cavity:
For pain in the lower abdomen, the disease is differentiated from adnexitis and ovarian apoplexy. Benign and malignant neoplasms, specific enlargement of mesenteric lymph nodes in HIV infection, syphilis, and lymphogranulomatosis may have similar symptoms.
The main task in treating the disease is to identify and sanitize the primary source of infection. In uncomplicated acute course of the disease, conservative therapy is used. Antibacterial drugs are prescribed etiotropically, based on the type of bacterial pathogen.
For tuberculous mesadenitis, specific therapy is indicated in an anti-tuberculosis dispensary. Anti-inflammatory, painkillers, and immunostimulating drugs are prescribed symptomatically. For intense, prolonged pain, a perinephric block is performed.
To reduce intoxication, parenteral detoxification therapy is performed.
For purulent mesadenitis, surgical treatment is indicated. The abscess is opened and drained with an inspection of the abdominal cavity. All patients are recommended to follow a diet (table No. 5). It is necessary to give up fatty, fried, smoked foods, flour products, coffee, and alcohol.
Preference should be given to low-fat varieties of fish and meat, vegetable soups, porridges, and fruit drinks. It is recommended to take food 4-5 times a day in small portions. Physiotherapeutic treatment includes magnetic therapy and UHF therapy.
During the period of remission and rehabilitation, therapeutic exercises under the supervision of a physical therapy doctor are indicated.
The prognosis of mesenteric lymphadenitis is favorable with timely diagnosis and proper treatment of the disease. The development of complications can lead to severe, life-threatening conditions (peritonitis, sepsis, intestinal obstruction).
The basis of prevention is the identification and treatment of chronic foci of inflammation, which can serve as a source of the formation of mesadenitis.
For prevention, periodic medical examinations, maintaining a healthy lifestyle and strengthening the immune system (taking multivitamins, walking in the fresh air, hardening) are of great importance.
Source: https://www.KrasotaiMedicina.ru/diseases/zabolevanija_gastroenterologia/mesadenitis
Causes of inflammation of the intestinal lymph nodes in children
Mesadenitis is an acute or chronic inflammation of the lymph nodes located in the abdominal cavity near the mesentery of the small intestine.
It is a fairly rare disease that is not often diagnosed in children, regardless of their age group. In most cases, it occurs in an acute and dynamically developing form with many severe complications if an adequate treatment process with the use of drug therapy does not begin in a timely manner. It is believed that the younger the child, the more severe the disease and is accompanied by severe pain.
At risk are children who have a weak immune system, whose cells are not able to resist infectious microorganisms.
Symptoms of acute mesadenitis in a child
The signs of this disease are quite vague and if a child is admitted to the inpatient department in unsatisfactory health, there is a high probability that the doctor examining the young patient will not be able to immediately recognize the presence of mesadenitis.
Therefore, it is necessary to pay special attention to the following list of symptoms indicating inflammation of the abdominal lymph nodes:
- acute pain inside the abdomen, which resembles a spasm and forces the child to take a horizontal position with the legs tucked to the chest;
- body temperature rises to 38-39 degrees Celsius;
- fever and increased sweating;
- general physical weakness, drowsiness, headache;
- loss of appetite with complete or partial refusal to eat;
- nausea, vomiting and stool upset, manifested in liquid diarrhea or prolonged constipation.
During palpation of the surface of the abdomen in the circumference of the navel, you can feel dense tubercles, which have different sizes, but are located next to each other. These are clear signs that the child is developing the initial stage of mesadenitis.
Causes of inflammation of the lymph nodes in the intestines in a child
There are not such a large number of causative factors influencing the occurrence of this disease. Therefore, based on rich medical practice in the field of diagnosis and treatment of pathologies of the lymphatic system in children of all age groups, the following causes of mesadenitis are identified:
- hereditary predisposition, when close relatives suffered from this disease in the family;
- the lumen of the small intestine is too thin, allowing infection to enter the tissue of the mesenteric lymph nodes;
- the presence in the body of dangerous strains of microorganisms in the form of tuberculosis bacillus, HIV, hepatitis, hospital type Staphylococcus aureus;
- an overly weakened immune system, the cells of which do not react aggressively enough to biological agents that penetrate the child’s body;
- focus of chronic infection in nearby gastrointestinal organs;
- abdominal injuries and recent surgical interventions on the gastrointestinal tract.
In the latter case, inflammation of the lymph nodes develops during the process of rehabilitation and healing of damaged tissues, as a natural and physiological reaction of the body to external intervention. It is much worse when the pathological state of the lymphatic tissue persists after complete restoration of the operated area.
Diagnostics and tests
To make the most accurate diagnosis with the further formation of a therapeutic course aimed at curing the child of mesadenitis, it is necessary to undergo the following types of examinations and pass the appropriate tests:
- blood from a finger for clinical study of its cellular composition;
- venous blood to isolate viral, bacterial and fungal infections, as well as toxic compounds that poison the lymphatic system;
- gastroscopy of the stomach to exclude gastritis or peptic ulcer;
- endoscopy of the small and large intestines;
- morning urine, which is given on an empty stomach, and its results reflect the severity of the inflammatory process in the baby’s body;
- Ultrasound diagnostics of the abdominal organs, as well as the area of the mesentery, where enlarged lymph nodes are localized.
If these types of diagnostic measures are not enough, then an additional MRI of the peritoneum is performed so that the surgeon can determine how extensive the pathological focus of inflammation is and what type of treatment is required in a specific clinical situation.
Treatment of mesadenitis in children
There are several methods for ridding a child of this disease with minimal risk of relapse of the disease. In this regard, the following directions are used in the treatment of mesadenitis, regardless of the patient’s age.
Diet
Properly organized nutrition is also part of general therapy that strengthens the digestive, lymphatic, and immune systems of children. To achieve a positive therapeutic effect, it is recommended to include in the child’s menu the following types of products:
- salads of fresh vegetables with herbs, seasoned with sunflower or olive oil;
- cottage cheese, kefir, fermented baked milk, yogurt, low-fat sour cream;
- cereal porridges boiled to a jelly state (buckwheat, wheat, barley, oatmeal, corn, pearl barley);
- chicken breast meat, cooked in a steam bath or boiled in water;
- compote of dried fruits, rose hips;
- milk jelly;
- chicken broth with croutons;
- lean fish meat baked in the oven or boiled in water;
- vegetable soups.
The principle of dietary nutrition for a child with mesadenitis is to not overload the intestines and at the same time provide the child’s body with all the nutrients.
Pills
Drug therapy plays a key role in stopping further progression of the disease, as well as the onset of severe complications. The type of drug that is advisable to use in a specific clinical case is determined individually by the attending surgeon. The most commonly used drugs are in the following categories:
- potent antibiotics to fight infectious microorganisms;
- antiviral drugs, if the cause of the inflammatory process is invasion by microorganisms of this type;
- broad-spectrum antispasmodics for pain relief of pathological symptoms;
- vitamin and mineral complexes to stimulate the child’s immune system to work more actively and relieve inflammation of the intestinal lymph nodes.
Tablet medications are not always able to have a positive therapeutic effect, therefore, if necessary, the child is additionally prescribed intramuscular or intravenous injections. It all depends on the severity of the disease.
Folk remedies
In addition to conservative methods of treating mesadenitis in children. There is an alternative direction in the fight against this disease, which consists in using an anti-inflammatory decoction of several types of medicinal herbs. This recipe has been used by traditional healers for many decades and has proven highly effective in practice.
To prepare a home remedy for mesadenitis, you must follow the following recipe:
- Take 5 grams of dried plants in equal proportions - chamomile, plantain, thyme, coltsfoot, St. John's wort.
- Pour ingredients into a metal ladle or pan.
- Pour running water and boil for the next 15 minutes.
- Upon completion of the cooking process, allow the broth to settle and cool.
- Strain the anti-inflammatory remedy for mesadenitis for children so that there are no particles of dried plants in the liquid.
Take folk medicine 50 grams 3 times a day 30 minutes before meals. This drink has a bitter taste, so children of the younger age group may be capricious and refuse to take it. In this case, you can add a little honey to make the broth have a more pleasant taste and aroma. Duration of treatment is 10-15 days.
Possible complications in the absence of proper treatment
In the absence of an adequate therapeutic effect on the source of inflammation of the lymphatic tissue in the intestine, it is not excluded. That the following negative consequences will occur in the child’s body:
- exacerbation of the pathological process in the lymph nodes of the abdominal cavity and the formation of a purulent abscess;
- critical decrease in the protective functions of the immune system;
- leakage of pus from the area of the abscess into the abdominal cavity and the onset of inflammation of adjacent internal organs;
- transition of the disease into a chronic form with periodic exacerbations;
- the need for surgical intervention to remove the affected intestinal lymph nodes.
The most dangerous and severe complication of mesadenitis for a child’s body is septic blood poisoning, when the concentration of infectious microorganisms in the lymphatic system becomes critical and they enter the bloodstream. In this case, death occurs quite quickly.
Mesadenitis in children: causes, symptoms and treatment
In recent years, there has been an increase in the incidence of mesadenitis among the child population, although it is possible that this is due to improved diagnostics and the introduction of ultrasound and computer technology. Children aged 6-13 years are most susceptible to the disease, with girls getting sick less often than boys. In this article, we will look at mesadenitis in children, talk about the symptoms of this disease, as well as possible treatment.
Source: https://tsitologiya.su/zheludok/vospalenie-limfouzlov-kishechnika-u-detej-prichiny
Symptoms
Mesadenitis is a pathology, the existence of which people most often do not suspect. Abdominal lymph nodes are located inside the peritoneum, and their enlargement can only be diagnosed using ultrasound.
Symptoms of the disease appear suddenly and are more typical only in acute cases. Patients suffer from pain in the abdominal area, in some cases it is impossible to indicate the exact location of the discomfort. If enlarged lymph nodes occur in the lower abdomen on the right, patients often confuse the pathology with appendicitis, since the pain and all the symptoms are very similar:
- Increased body temperature.
- Nausea and vomiting.
- Lack of appetite and stomach pain.
- Diarrhea or constipation.
- Tachycardia.
- Enlarged spleen and liver.
- Dry mouth, dehydration.
If symptoms are ignored for a long time, the patient may receive unpleasant symptoms in the form of peritonitis, intestinal obstruction and other serious diseases. This happens because the lymph nodes begin to fester without proper treatment.
The chronic form of the course is less noticeable to humans, the clinical picture is blurred and rarely causes concern. There is practically no pain syndrome, pain is felt only during physical activity.
The pathology often affects children. According to statistics, girls get sick less often than boys. Age range from 6 to 13 years. The symptoms are no different from adult mesadenitis. When palpating the abdomen, you can find that it is tense, this is due to the formation of lymphoid follicles. It is necessary to consult a specialist to avoid complications and begin the necessary treatment on time.
Diagnostic methods
The treating pediatrician must first collect information from parents about previous illnesses and also study the medical history. After this, the specialist conducts an examination, assesses the condition of the tongue, skin color, and breathing. Normally, there should be no spots on the tongue. Rapid breathing, pale skin, pain on palpation of the abdomen are the first symptoms that the child needs to be checked for mesadenitis.
Additional diagnostic measures include:
- general clinical blood test;
- biochemical blood test;
- ultrasound diagnostics or x-ray of the abdominal organs;
- fecal analysis for helminths;
- colonoscopy;
- tuberculin test.