From the moment the baby is born, parents, together with pediatricians, carefully monitor the child’s health. The most accessible and informative way to diagnose various diseases at an early stage is a general blood test. And one of the most important indicators of the body, which doctors pay close attention to, is the number of leukocytes (white cells) in the blood. After all, they are the barriers to the passage of viruses and bacteria, determine the level of the body’s resistance and are responsible for the general immunity of a person.
The norm of leukocytes in the blood of children changes with age, but other physiological and pathological factors can also influence the results of the analysis. We will understand all the intricacies of passing a clinical analysis and determine when a decrease or increase in leukocytes is observed in a child and what this is connected with.
What are leukocytes needed for?
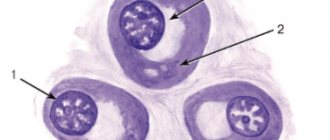
In children, white blood cells are formed mainly in the bone marrow, spleen and lymphatic system. Then the white blood cells spread throughout the body, penetrating all organs and tissues; their concentration is especially high if there are damaged areas or foci of inflammation and infection. Leukocytes try to resist and neutralize harmful microorganisms on their own. Leukocytes vary in composition and are divided into several types, each of which has its own function. For example, phagocytes digest and destroy foreign particles in the blood. The process of white blood cells fighting bacteria is called phagocytosis. When a foreign microorganism is larger than a leukocyte in size, a group of blood cells accumulates around it. After digesting unnecessary particles, white blood cells die.
Thus, white blood cells are responsible in recognizing, capturing and destroying harmful particles.
What kind of cells are these?
To be precise, red blood cells are not cells, but postcellular structures that, upon maturation, lose a large number of organelles and all nuclear components. This happens so that they can more effectively perform their main function - transporting oxygen to tissues and organs.
Red blood cells contain a lot of hemoglobin, which attracts molecules of the vital gas. Red blood cells are round, biconcave and elastic, which helps them move freely even in small vessels.
In addition to oxygen, red blood cells also carry other substances. These include:
- Immune elements;
- Complement components;
- Immunoglobulins;
- Biologically active substances.
The distribution of all these elements is an important function that helps maintain the protective and regulatory activity of the body; with the development of various diseases, it is disrupted.
Red blood cells
Types of erythrocytosis
An increased content of red blood cells in the blood is called erythrocytosis. There are two types of this pathology depending on the cause that caused it:
- Relative type. Its essence lies in the fact that the number of red blood cells themselves does not increase. Pathology occurs because blood thickens and plasma is lost. This is possible due to dehydration and other factors.
- Absolute type. This erythrocytosis is already associated with an increased number of blood cells themselves, which are synthesized too quickly in the bone marrow.
What to do
If the red blood cells increase more than 8.0 x 1012/l, repeat the analysis to exclude laboratory errors. If the results are reliable, additional research needs to be carried out:
- Determination of hemoglobin;
- Hematocrit values;
- Content of platelets and leukocytes;
- Erythrocyte sedimentation rate (ESR).
The morphological structure of red cells is of great importance in this disease. The presence of anisocytosis (cells of different sizes) in the absence of iron deficiency is inherent in erythremia. A severe course of the disease is indicated by a high level of platelets and leukocytes. ESR indicators are reduced and equal to zero. In addition to the general analysis, the following is prescribed:
- Biochemical blood test.
- Sternal puncture (bone marrow examination).
- Trepanobiopsy (histological examination of material from the ilium), a method that provides reliable information about the main symptom of the disease - three-line hyperplasia.
- Ultrasound of the abdominal organs.
Based on the results obtained and examination of the little patient, the doctor prescribes treatment. During treatment, the pediatrician recommends adhering to the following rules for caring for your baby:
- Organize the correct water regime for your child. Avoid carbonated drinks and use clean drinking water for drinking;
- Provide a balanced and rational diet with a predominance of fresh fruits and vegetables. Supplement your diet with lemons, berries, beets, garlic - blood thinning products;
- Ventilate the room more often and monitor air humidity.
Normal for a child
The concentration of red blood cells is calculated per 1 liter of blood. In children, the rate varies depending on age. Therefore, when deciphering the results of a blood test, you need to take into account how old the child is.
Cells that were formed during the perinatal period of development are capable of carrying much more oxygen than the red blood cells of an adult. But then the content of these bodies decreases.
Normally, the number of red blood cells is as follows:
- The first hours of life – 5.4-7.2*10*12 U/l.
- The first 3 days after birth – 4.0-6.6*10*12 U/l.
- From a month to a year – 3.0-5.4*10*12 U/l;
- From one year of age to 5 years – 3.6-4.9*10*12 U/l.
- From 6 years to 12 years – 3.6-5.2*10*12 U/l.
- Over 13 years old – 3.6-5.6*10*12 U/l.
During adolescence, a specific level of red blood cells is established, which remains unchanged throughout life.
Causes of increased red blood cell levels
Among the reasons why there is an increased content of red blood cells in the blood, pathological and physiological are distinguished. The former mean the development of a disease that needs to be eliminated, while the latter do not pose a danger to patients and disappear on their own.
Important! According to medical practice, children who live in mountainous areas always have an increased level of red blood cells. In this case, the body tries to avoid developing altitude sickness. This is a purely physiological factor.
But there are other reasons that influence an elevated blood count. Red blood cells are elevated if the following phenomena occur:
- Diarrhea, vomiting due to intestinal infection.
- Increased body temperature.
- Excessive sweating during exercise or fever.
- Regular exercise.
- Being in hot climates or in a stuffy room.
- Inhalation of cigarette smoke by a child.
Relative erythrocytosis may occur if the child has received extensive burns. At this moment, the body loses proteins and plasma, and blood thickening occurs. In a newborn baby, an increased number of cells in a blood test may be due to hypoxia that occurred in the womb.
Absolute erythrocytosis appears due to the following pathological conditions in children:
- Erythremia. It is a blood disease. As a result, all blood cells begin to be rapidly produced, of which the largest number of red blood cells becomes.
- Chronic pathologies of the respiratory system. Blood cells may increase due to the fact that the child suffers from prolonged hypoxia, bronchial asthma and other lung diseases. An increased level of red blood cells is needed so that more oxygen reaches the cells of the organs.
- Congenital heart defects. Most often, the number of blood cells increases due to diseases in which blood circulation in the lungs is impaired.
- Hypernephroma. At the same time, a lot of erythropoietin is synthesized in the kidneys, which in turn provokes the active production of red blood cells in the bone marrow.
The worst thing that an increased level of red blood cells in the blood can indicate is malignant neoplasms of the liver or kidneys . But whatever the cause of erythrocytosis, the initial factor is the same - insufficient oxygen supply to the body. As a result, he tries to produce blood cells above normal to protect himself from starvation.
Hypoxia
Red blood cell count disorder
The content of the number of red cells, for various reasons, can change both in the direction of a lower blood count and in the direction of its increase from the norm.
Red blood cells below normal (causes, symptoms)
A low level of red blood cells is called erythropenia. This pathology can be of 2 types:
- relative or false erythropenia - the number of cells is in full, but a low indicator is associated with blood thinning, for example, in the case of a child taking copious amounts of fluid;
- absolute erythropenia is a pathology manifested by a lack of red blood cells in the blood.
A decrease in the number of red blood cells affects the child’s well-being and can develop for the following reasons:
- pathology of the formation of red blood cells in the bone marrow - this condition can be caused by an insufficient amount of vitamins and minerals supplied to the child’s body with food. Poisoning with various poisons or long-term use of medications that have side effects on the composition of the blood can play a negative role;
- destruction of red blood cells - this pathological process can be triggered by a long-term chronic infection, inflammation of internal organs, autoimmune processes and other toxic effects on the child’s red blood cell;
- increased outflow of red cells from the body - can occur with injuries accompanied by bleeding, surgery, kidney disease, when red blood cells enter the excretory system.
A decrease in the number of red blood cells appears in various diseases, such as:
- pyelonephritis and glomerulonephritis;
- hereditary pathologies of erythrocyte development;
- diseases of the digestive system in childhood;
- collagenoses;
- Iron-deficiency anemia;
- chronic renal failure;
- cirrhosis of the liver.
A quantitative decrease in red blood cells, in any disease, will manifest itself as clinical symptoms in a child in the following form:
- pale skin;
- capriciousness and lethargy of the baby;
- poor appetite;
- taste perversions in the form of using chalk;
- an increase in temperature to subfebrile levels;
- dry skin and brittle hair;
- fatigue, weakness;
- decreased blood pressure;
- periodic occurrence of dizziness and fainting;
- frequent cold infections.
Consequences of erythropenia
Most often in children, a decrease in red blood cells provokes the development of anemia, a characteristic feature of which is iron deficiency.
Bone marrow function can be assessed by the number of immature red blood cells. If the number of reticulocytes is observed to increase in number when treating anemia or the consequences of bleeding, then this is a positive symptom from the use of drugs.
In addition, to increase the level of hemoglobin, the baby needs to include foods rich in iron in his diet. If anemia is a consequence of another pathology, then the doctor will prescribe medication for the baby.
Sometimes, the development of iron deficiency anemia in children is psychosomatic in nature, when it is not possible to establish the cause of the pathology or long-term and high-quality treatment does not produce results. In this case, the appearance of the disease is associated with the influence of psychological factors and the characteristics of the baby’s emotional background.
Diseases of a psychosomatic nature often develop in children in a certain age category. These are 1 year, 3 years, 7 years and 13 – 15 years. Treatment of anemia, as a manifestation of psychosomatics, by a specialist psychologist gives good results, which is confirmed by laboratory tests.
Red blood cells are higher than normal (causes, symptoms)
The detection of an increased number of red blood cells in children is called erythrocytosis, which can be relative or true.
The causes of erythrocytosis, which is relative in nature, may occur in the following circumstances:
- when blood thickens due to dehydration with diarrhea or frequent vomiting;
- physical activity;
- when staying in a hot and stuffy room;
- as the temperature rises.
With true erythrocytosis, when the baby’s red blood cells are elevated, their excessive formation occurs in the bone marrow. This pathology can be observed in the following diseases:
- erythremia;
- diseases of the respiratory system of a chronic nature;
- congenital heart defects;
- Itsenko-Cushing's disease;
- kidney tumors.
The manifestation of erythrocytosis is accompanied by the following symptoms:
- hyperemia of the skin;
- pain in the limbs that is burning in nature;
- increased blood pressure;
- enlarged spleen.
Consequences of erythrocytosis
In this case, it is important to diagnose the cause that caused the increase in the number of red cells in the baby. Lack of treatment threatens further thickening of the blood, which can lead to the formation of blood clots and deterioration of blood supply not only in the internal organs, but also in the vessels of the brain.
Mandatory systematic monitoring of the analysis of the quantitative content of red cells in the baby’s bloodstream, during preventive examinations or as indicated, will allow timely identification of pathology in the quantitative content of red blood cells and treatment.
How does ertocytosis manifest itself?
Since an increase in red blood cells in the blood becomes an indicator of the development of some pathology, the symptoms correspond to a specific disease. If the following signs are observed with erythrocytosis, you should immediately inform your doctor:
- The skin takes on a reddish or bluish tint.
- Blood pressure rises.
- The spleen enlarges.
- General symptoms of hypoxia are noted: dizziness, fatigue, headaches.
Important!!! With an increased number of red blood cells, the blood begins to thicken, therefore the risk of blood clots increases significantly. This can greatly affect the child's health and lead to serious consequences.
Red skin color may be a symptom of erythrocytosis
Clinical manifestations
There are no symptoms with relative erythrocytosis. In case of viral infection or gastrointestinal diseases, clinical manifestations will correspond to the underlying disease.
However, absolute erythrocytosis is characterized by the following symptoms:
- Changes in skin tone such as erythrocyanosis, redness of the eyes;
- Headache and dizziness;
- General malaise, weakness;
- Increased blood pressure;
- Pain in the left hypochondrium due to hyperplasia of the spleen;
- Joint pain;
- Impaired hearing and vision;
In the last stage of the disease, severe complications occur (thrombosis of the coronary vessels, gastric ulcer, cirrhosis of the liver).
Can red blood cells be low?
A blood test in a child may show a condition opposite to erythrocytosis, when there are not more blood cells, but less than normal. This is also possible due to the development of pathological disorders in the body.
The reasons for a low number of red blood cells include the following:
- Bone marrow disorders. The lack of red blood cells can be caused in this case by a deficiency of vitamins and microelements. This often occurs in people suffering from hypovitaminosis or who do not eat meat. Bone marrow function is negatively affected by the effects of poisons, neoplasms, medications, and radioactive substances.
- Destruction of red blood cells during circulation. This phenomenon is observed with the development of chronic inflammatory processes, infectious pathologies, autoimmune reactions of the body, intoxication, and taking certain medications.
- Intensive removal of red blood cells from the child's body. This usually happens with bleeding that occurs in the event of injury or surgery. The disorder may also be associated with internal bleeding.
The normal level of red blood cells decreases in children with iron deficiency anemia, leukemia, hemophilia, B12-deficiency anemia, pyelonephritis, intestinal infections, chronic renal failure, myeloma and many others.
Destruction of red blood cells
Red blood cells in your baby's blood
Red blood cells are the largest group of red cells, the formation of which occurs in the bone marrow.
Formation of red blood cells
This anucleate cell has the shape of a disk, the center of which is concave on both sides. The red color of this component of the blood is due to the presence of a large amount of hemoglobin.
Cells have pronounced plasticity and the ability to change their shape, which allows them to pass into the smallest capillaries of the bloodstream.
The viability of red blood cells is 3–4 months, after which they are destroyed in the liver and spleen. In newborns, the life of a red blood cell is short, amounting to only 12 days. But soon, it begins to increase, reaching a duration of 3 - 4 months, that is, like in adults.
The role of red blood cells
Participation in tissue respiration is the delivery of oxygen by hemoglobin from the alveoli of the lungs to the tissues of the whole body with the subsequent utilization of carbon dioxide, that is, its transfer from the tissues to the lungs. Gas exchange occurs in the capillary network of the organ, where the speed of blood flow is minimal. Hemoglobin is a special, complex protein containing iron.
Only a normal number of red blood cells can ensure the full functionality of all body systems and individual organs.
Functions of red blood cells
The functions of red blood cells are diverse and important in the normal life support of the body:
- nutrition – red blood cells transport amino acids from the digestive organs to the cells of the whole body;
- protection – red cells absorb toxic substances and antigens pathological for the body;
- regulation of blood pH – the body maintains a normal acid-base composition;
- enzymatic function - red cells transport various enzymes and vitamins, that is, specific protein catalysts;
- blood group characteristics - markers present on cell membranes determine the blood group;
- participation in the blood coagulation process - the presence of coagulation factors in red cells.
Considering the importance of the functions performed by red cells to ensure the normal functioning of all systems, their quantitative composition in the body plays a large role.
Preparing and conducting analysis
In order for the test result to be reliable, you need to prepare for donating blood. First of all, you should know that the procedure is carried out in the morning on an empty stomach. You can take your last meal 8 hours before the start of the procedure. The only thing you can do is drink water.
Important!!! This rule does not apply to infants. They cannot be left without food for such a long time. In these cases, the laboratory takes into account the fact of food intake, and the result is deciphered and adjustments are made.
Blood is taken from children only from the capillaries that run in the finger. In newborn babies, the material is removed from the heel. The blood is then sent to specialists who use a microscope to determine the number of red blood cells in the blood.
Carrying out a blood test
Treatment
If your child complains of constant fatigue and has pale facial skin, contact your pediatrician. To clarify the type of anemia, the doctor prescribes a number of laboratory tests:
- Clinical blood test;
- The average volume of red blood cells in the blood (reduced in anemia);
- Erythrocyte indices;
- Hematocrit
When establishing a diagnosis, the morphological characteristics of red blood cells are also important. Example: iron deficiency anemia is characterized by an erythrocyte index (anisocytosis) and anisochromia (heterogeneity of cell coloring) with low hemoglobin. Normally, these indicators are absent. The pediatrician prescribes treatment based on tests. In case of erythropenia associated with other diseases, the cause of the underlying disease should first be eliminated.
A deviation of red blood cells from the norm is not always a disease; however, parents should consult a pediatrician so as not to miss a possible disease. Only an additional diagnostic examination will provide a complete picture of the blood and help make an accurate diagnosis.
Treatment of erythrocytosis
The treatment regimen is developed individually, depending on what caused the development of erythrocytosis. After a blood test shows that there are more red blood cells than normal, you will need to undergo additional diagnostics.
If the patient is not bothered by any symptoms, it means that the enlargement of the corpuscles was caused by a physiological factor. After some time, the indicator will return to normal on its own, so no therapeutic measures will be required. If symptoms exist, then an examination will help identify the disease and eliminate it.
There is a method of treatment called bloodletting. It is used if a person has a large volume of blood, which increases the pressure in the vessels. With this therapy, the doctor makes incisions on the patient's body or uses leeches. This procedure can also be used for some heart defects.
In addition, the attending physician can prescribe medications that help thin the blood and vitamins. During the treatment period, it is important to eat well. You should not eat fatty foods. It is best to feed your child fruits, vegetables, dairy products, fish, cereals, and nuts.
It is recommended to give your baby more to drink. The amount of liquid that should be consumed per day depends on the age of the child. It is best to drink purified still water. It is important to regularly ventilate and humidify the room in which the child is located.
If red blood cells are elevated in children, then it is imperative to find out the cause of this phenomenon. It may not pose any danger to the health and life of the baby, or, conversely, lead to unpleasant consequences. Therefore, elevated red blood cells should not be left unattended.
Restoring blood counts
Preventive measures
To prevent erythropoiesis, general recommendations are used to reduce the risk of developing most pathologies.
You can protect yourself if:
- Lead a healthy and active lifestyle. To refuse from bad habits.
- Eat nutritiously and rationally. Don't eat a lot of salty, fried, fatty foods. Try to plan your menu so that the body is provided with all the necessary nutrients and vitamins. Elements such as vitamin B, folic acid, and iron are especially important for hematopoiesis.
- Consult a doctor promptly if there is even the slightest suspicion that a child is developing any disease. This is the surest way to prevent diseases.
If every parent is attentive to the health of their children and takes them for medical examinations on time, then the likelihood of negative consequences will be reduced to a minimum.