Measles is a dangerous viral infection that claims hundreds of thousands of lives around the world every year. Only the measles vaccination can help protect against this serious disease. Let’s take a closer look at how long vaccination lasts, how long the body’s resistance to measles lasts, and what this disease actually is.
Measles
An RNA virus is considered the causative agent of the disease. In general, measles is more of a childhood disease, but if an unvaccinated adult becomes infected with the virus, the course of the disease for him is most complex, leaving behind various complications. The virus spreads when the patient coughs, sneezes with particles of mucus, or when talking with saliva. An infected person becomes contagious even when he himself does not feel symptoms of the disease, that is, during the incubation period. The only protection is the measles vaccination. How long it acts in the body is a question that interests many. You are guaranteed to be protected for 10-12 years, as doctors say.
If the virus has entered an unprotected body, the patient begins to notice symptoms that are more typical of many respiratory diseases:
- fever (temperature up to 40 degrees);
- sore throat, sore throat;
- dry cough, runny nose;
- weakness, malaise;
- headache.
Specific signs of measles include the following symptoms:
- conjunctivitis and photophobia;
- severe swelling of the eyelids;
- rashes on the mucous membranes of the cheeks appear on the second day (whitish small spots like grains of semolina, which disappear after a day);
- on the 4-5th day - a rash on the skin, first it appears on the face, then spreads down throughout the body.
Categories
How is vaccination of contact persons carried out in measles outbreak areas? Why do preventive measures sometimes turn out to be ineffective and those vaccinated for epidemic reasons among their contacts still get sick? What does the formation of the correct immune response during vaccine prevention of measles depend on in contact persons in the outbreaks of the disease?
In the language of numbers
Measles is a highly contagious, severe disease of viral origin. The infectivity index is 95–96%, and the natural susceptibility is 100%. The World Health Organization (WHO) estimates that there were 2.6 million deaths from measles in 1980, before widespread vaccination. Despite the availability of a safe and effective vaccine, measles remains a leading cause of death among young children worldwide. In 2013, 145.7 thousand people died from this disease, most of whom were children under 5 years of age.
According to WHO, accelerated immunization efforts have significantly reduced the death rate from measles. Since 2000, mass vaccination campaigns have immunized more than 1 billion children aged 9 months to 14 years living in high-risk countries against the disease, including about 145 million in 2012. Global measles deaths have fallen by 75% - from 544.2 thousand deaths in 2000 to 145.7 thousand cases in 2013. The countries of North and South America have achieved the greatest success in completely eliminating the incidence of measles thanks to the correct vaccine prevention strategy.
At the same time, in the Russian Federation, the incidence of measles in 2013 increased by 9.4% and amounted to 1.63 cases per 100 thousand population (for comparison: in 2012 - 1.49 cases per 100 thousand population) . From January to September 2014, 4,580 cases of measles were registered in Russia, the incidence rate was 3.2 cases per 100 thousand population. Compared to the same period in 2013, the incidence rate increased 5 times.
For immunoprophylaxis of measles in Russia, a live cultured measles vaccine is used, consisting of attenuated strains of the measles virus Leningrad-16 and Moscow-5. The strains are obtained by cultivating Japanese quail embryonic cells in a primary culture, followed by purification and lyophilization. The vaccine stimulates the production of measles antibodies in 95% of seronegative individuals on days 21–28 after administration; immunity persists for at least 18 years.
According to the National Preventive Vaccination Calendar[1], routine vaccination against measles, simultaneously with vaccination against rubella and mumps, is organized twice: at the age of 12 months, when infants usually lose maternal antibodies transmitted to them through the placenta, and at 6 years (before admission to school). In addition, routine vaccination against measles is carried out for children aged from 1 to 18 years inclusive and adults under the age of 35 who have not previously been vaccinated, have no information about vaccinations against measles and have not had this infection. It is performed in accordance with the instructions for the use of vaccines twice with an interval of at least 3 months between vaccinations. Persons previously vaccinated once are subject to a single immunization at least 3 months after vaccination.
In order to prevent and spread the incidence of measles, as well as rubella and mumps on the territory of the Russian Federation, the Decree of the Chief State Sanitary Doctor of the Russian Federation dated July 28, 2011 No. 108 approved SP 3.1.2952-11 “Prevention of measles, rubella and mumps.” This regulatory legal act regulates the activities that are required in measles outbreaks. Given the massive nature of the incidence of measles, the goal of carrying out anti-epidemic measures at the source of infection is its localization and elimination.
In accordance with clause 5.10 of SP 3.1.2952-11, persons who have had contact with a patient (if the disease is suspected), have not had measles before, are not vaccinated, and do not have information about vaccinations against measles are subject to immunization against measles for epidemic indications without age restrictions , as well as persons vaccinated against measles once [2]. It is carried out within the first 72 hours from the moment the patient is identified. If the boundaries of a measles outbreak expand (at a place of work, school, within a district, a settlement), the immunization period can be extended to 7 days from the moment the first patient in the outbreak is identified. According to clause 5.12 of SP 3.1.2952-11, children who have not been vaccinated against measles or mumps (who have not reached vaccination age or who have not received vaccinations due to medical contraindications or refusal of vaccinations), no later than the 5th day from the moment of contact with the patient normal human immunoglobulin is administered in accordance with the instructions for its use.
Why are preventive measures sometimes not effective? The immunization deadlines established by sanitary rules have been met, but those vaccinated for epidemic reasons among their contacts still get sick. To answer this question, it is necessary to understand the features of the pathogenesis of measles.
The causative agent of measles is a virus from the paramyxovirus family. It usually develops in cells located in the back of the throat and in the lungs. The main source of infection is humans, the transmission mechanism is aerosol, and the route of transmission is airborne.
The clinical picture of measles is divided into 3 periods:
- catarrhal (prodrome);
- period of rashes;
- period of pigmentation or convalescence [1].
A reliable clinical diagnosis of “Measles” is established during the period of manifestation of the rash, before which the clinical picture resembles the course of ARVI with symptoms such as cough and (or) runny nose, general intoxication, temperature 38 °C and above.
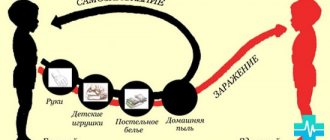
The entry points for the virus are the respiratory tract and the conjunctiva of the eyes. Initially, the measles virus multiplies in the epithelial cells of the mucous membranes of the cheeks and upper respiratory tract, then enters local lymphoid tissues, which leads to primary viremia and spread of the virus to other regional lymph nodes and organs, including the kidneys, gastrointestinal tract, liver, etc. It is known that the primary reproduction of the measles virus occurs in the local lymphoid tissue, and on the 3rd day of the incubation period it enters the blood. The amount of virus in the initial period is not large and can be neutralized by the introduction of gamma globulin, which is what passive immunization carried out in foci of measles infection is based on. However, we would like to remind you that the period of passive immunization is limited to 72 hours from the moment of contact.
The first wave of viremia reaches its greatest intensity in the catarrhal period and on the 1st day of the rash period, when the measles virus is contained in large quantities in the secretions of the mucous membranes of the upper respiratory tract. From the 3rd day of the rash period, the amount of virus secreted sharply decreases; by the 5th day it ceases to be detected in the blood.
The second wave of viremia is recorded at the end of the incubation period and the beginning of the catarrhal period, when fixation and reproduction of the measles virus occurs in the cells of the macrophage system of lymph nodes, tonsils, liver, spleen, and in the lymphoid tissue of the bone marrow. This coincides in time with the clinical manifestation of the infection. Complete elimination of the measles virus from the blood and other tissues occurs within 1–2 weeks from the onset of the rash [7, 8].
The incubation period for measles is 8–17 days, in most cases it lasts 8–11 days. The infectious period for measles is observed in the last 2–3 days of the incubation period, 3–4 days of the catarrhal period and 3–5 days of the rash period [3, 4, 6]. The patient is most contagious in the catarrhal period, when transmission of the virus occurs especially actively during coughing, sneezing, lacrimation, talking, etc. Accordingly, more than 3 days (72 hours) can pass from the moment of initial contact to the entry and primary reproduction of the measles virus in the body of the contact. until the patient’s diagnosis is reliably confirmed clinically (a rash appears) (see Fig. 1). If contact occurred with a person with measles on the first day of the onset of the rash (diagnosis was established clinically), then vaccination of contact persons in the outbreak can be carried out within the time frame established by SP 3.1.2952-11, i.e. within 72 hours (see Fig. 2).
The WHO position paper on measles vaccines [10] outlines the following vaccine prophylaxis to eliminate a measles outbreak:
Extracted from Measles Vaccines: WHO Position Paper
To limit the impact of measles outbreaks, WHO supports surveillance for early detection, full risk assessment of spread and outcome of severe cases, and rapid response, including widespread use of measles vaccine. The district or regional outbreak coordinating committee, with broad representation, should decide on the type of vaccination response to be implemented at the local level. To protect high-risk individuals during an outbreak, vaccination may be administered within 2 days of exposure to the virus to mitigate the clinical course of measles; it may even prevent symptoms from occurring. In individuals for whom vaccination is contraindicated, administration of measles immune globulin within 3 to 5 days of exposure may have a similar benefit.
Please note that the severity of damage during infection with the measles pathogen depends on the dose of the virus received during contact [9]. According to foreign studies, the premorbid background (age, malnutrition, concomitant diseases, etc.) in this case has an insignificant effect. The severity of the disease in secondary patients is usually higher than in primary patients, which is due to a higher dose of the virus received during contact. The clinical picture of the disease in this case may develop more intensively, and the incubation period will be shortened.
It is also important that the accumulation of antibodies begins only 7–18 days after the vaccine is administered, and reaches maximum levels after 3–4 weeks. Accordingly, in areas with a large number of sick people, who may be in different periods of the clinical picture, including latently infectious, before obvious signs of infection appear, a vaccinated person for epidemic indications can receive an additional dose of the virus even before it enters his body. antibodies will accumulate to develop protective immunity against measles, and, as a result, you will get sick.
Immune response to measles vaccination
The immune response to live measles vaccine varies. The organisms of one group of people react strongly, while others react weakly. Even among vaccinated people, both children and adults, there are those whose bodies respond to the vaccine very weakly, up to complete insensitivity (5%) to the administered immunobiological drug. First of all, this concerns frequently ill children, in whom repeated respiratory diseases lead to disruption of the functioning of various organs and systems and help reduce the body’s immunoresistance [5]. In such children, as a rule, the schedule of preventive vaccinations is disrupted. It has been proven that children living in the Arctic react to live measles vaccine with a slight formation of specific antihemagglutinins [2]. With increasing age, there is an increase in the number of seronegative individuals among previously vaccinated and revaccinated individuals.
There are primary and secondary immune responses during vaccination.
Primary immune response. It starts immediately after the introduction of the antigen, but it can only be detected after a certain latent period. Antibodies appear in the blood after 7–10 days. Antibodies belonging to different classes of immunoglobulins are formed at different times. Early antibodies (IgM) usually exhibit low affinity for the antigen, while late antibodies (IgG) usually exhibit high affinity. The transition from IgM synthesis to IgG synthesis is regulated by T helper cells (CD4 lymphocytes). IgG antibodies to T-independent antigens are practically not produced. Some people do not develop antibodies even after multiple vaccinations. This condition is known as primary vaccine deficiency.
Secondary immune response . When the antigen is reintroduced, the immune response is significantly enhanced by both cellular and humoral immunity. The secondary immune response develops quickly, usually within 4–5 days, and is accompanied by a sharp increase in IgG titer. It is mediated by memory cells formed after the first contact with the antigen, and is characterized by intense proliferation of B lymphocytes and cytotoxic T lymphocytes. Conjugation with proteins converts polysaccharides into T-dependent antigens, therefore leading to the formation of memory cells upon first contact with the antigen and an increase in the immune response upon repeated contact. Often after vaccination, the antibody titer decreases quite quickly. This condition is called secondary vaccine deficiency. However, even in this case, immunity does not necessarily disappear completely: revaccination or contact with a pathogen, as a rule, causes the rapid production of antibodies (mainly of the IgG class). Thus, the absence of antibodies does not always indicate a loss of immunity, and conversely, the presence of antibodies after vaccination does not guarantee protection against infection [11].
To form the correct immune response during vaccine prevention of measles in contact persons in the outbreaks of the disease, three factors are important:
- timing of vaccination:
- if contact with the patient occurred on the first day of the appearance of the rash, then vaccination is carried out within 72 hours from the moment of contact;
- if contact with the patient was long-term (2-3 days, typical for family outbreaks) and occurred before the appearance of the rash, then the vaccination period is reduced to 12 hours from the moment the rash appears in the patient;
- no contact with a person with measles after vaccination for 2–3 weeks (until the required amount of antibodies is produced);
- Features of the immune response of the vaccinated body.
Literature
- Anisimova Z. P., Zhireva A. I., Sukharev V. M. Clinic of modern measles // Pediatrics. 1977. No. 1. P. 13–15.
- Anpilogova L.V. The state of measles post-vaccination immunity in children living in the Far North // Abstract of thesis. diss. ...cand. biol. Sci. M., 1986. 20 p.
- Bystryakova L.V. Infectious exanthemas in children. L.: Medicine, 1982. P. 216.
- Measles in adolescents and adults / L. V. Bystryakova, A. N. Platonov, I. N. Smorodinova [and others]. In the book: Children's viral infections. Tr. Linen. Institute named after Pasteur. 1997. T. 5. P. 35–39.
- Tsareva N. M. Immune status in frequently ill children living in an industrial city // Diss. ...cand. honey. Sci. Saratov, 2000. P. 127.
- Yuminova N.V., Zverev V.V. Elimination of measles in Russia // Medical records. 2003. No. 7/8. pp. 24–25.
- Acute measles in patients with and without neurological involvement: distribution of measles virus antigen and RNA / TR Moench, DE Griffin, CR Obriecht // J. Infect. Dis. 1988. 158: 433–442.
- Degree and length of viremia in adults with measles / D.N. Fortal, S. Aaranes, J. Blanding // J. Infect. Dis. 1992. 166: 421–424.
- Long-term survival after Edmonston-Zagreb measles vaccination in Guinea-Bissau: increased female mortality rate /P. Aaby, K. Knudsen, H. Whittle // J. Pediatr. 1993. 122: 904–908.
- Measles vaccines: document on the WHO position // Electronic resource. Access mode: https://www.who.int/immunization/WER_35_Measles_Position_paper_Russian_23Sep_09.pdf?ua=1.
- Immune response during vaccination // Knowledge base on human biology: electronic resource. Access mode: https://humbio.ru/humbio/infect_har/0018f5e8.htm#00190924.htm.
[1] Approved by Order of the Ministry of Health of Russia dated March 21, 2014 No. 125n.
[2] This requirement is also established by the Calendar of Preventive Vaccinations for Epidemic Indications, approved by Order of the Ministry of Health of Russia dated March 21, 205 No. 125n.
Possible complications of measles
Vaccination against measles will save you from the disease. As long as it works, the body will be protected from infection. In unvaccinated children, and even more often in adults, measles causes serious complications:
- measles or bacterial infection often causes pneumonia;
- bronchitis;
- sinusitis;
- keratitis (every 5th patient loses vision);
- meningitis and meningoencephalitis;
- otitis and eustachitis (later - hearing loss);
- pyelonephritis.
There is no effective antiviral treatment for measles. Only vaccination carried out in advance can save a person! In 0.6% of cases, measles is complicated by brain damage (encephalitis), and 25% of patients die.
How dangerous is measles?
At first glance, measles seems to be a fairly mild disease. Some opponents of vaccinations even believe that it is useful, as it strengthens the child’s body. And epidemics are a thing of the past because hygiene has improved.
The measles virus greatly disrupts the baby's immune system. Protection against other, more severe infections is weakened. Because of this feature, dangerous complications often arise.
The immune system spends a lot of effort to defeat the disease and eventually becomes exhausted. The child’s body simply will not have the strength to withstand the dangerous complications that bacteria will cause. Under normal conditions, the baby would not get sick at all, but his strength is exhausted, and the body becomes defenseless.
More often, complications of measles occur in children under five years of age, adolescents, the elderly, and women at any stage of pregnancy. Among the consequences are the following:
- one child out of ten, after suffering from measles, will develop otitis media caused by dangerous bacteria and will lose hearing for a long time;
- one in ten people who get sick will develop severe diarrhea;
- Every 20th sick child will have pneumonia. Because of such a terrible complication, children die most often;
- one in a thousand develops severe viral brain damage, which is incurable and leads to complete immobility and mental retardation;
- One or two children out of a thousand who have had measles die.
When to vaccinate
In Russia, vaccination against measles has been introduced into the scheduled vaccination calendar. A child is vaccinated at the age of 1-1.3 years. Revaccination is carried out at 6 years of age.
Due to the fact that the increase in the disease in 2014 in Russia led to serious consequences among the adult population, it was decided to vaccinate the population. According to the national program, free measles vaccination is introduced up to the age of 35. How long does the drug last? The immunity of a vaccinated person is on average resistant to the disease for up to 12 years (sometimes longer).
What should people over 35 do? Vaccination is carried out to everyone, but on a paid basis. The monovaccine is administered twice with a three-month interval. If you once received one vaccine, you need to get vaccinated again. Revaccination is not carried out for adults.
A little about the current state of affairs
Infectious disease doctors say that outbreaks of this insidious disease are characterized by periodicity. Increases in incidence occur at intervals of 5 or 6 years. It is no secret that in Russia over the past 2 years the number of people with measles has increased. Until July 2021, 127 cases of the disease were registered, mainly in Moscow and Dagestan. The increase in the number of cases is associated with numerous refusals of vaccination.
In order to prevent measles from entering the country, 95% of its population must be vaccinated. The so-called herd immunity is created. It will also protect those for whom vaccination is contraindicated. And a decrease in vaccination coverage by just 5% triples the incidence!
A similar situation is observed not only in the Russian Federation. Europe is also suffering from measles. Many cases of infection have been reported in Italy, France, Germany, Belgium, and Austria. Romania has the highest mortality rate among cases.
Emergency immunization
Regardless of the vaccination calendar and schedule, emergency immunization is carried out in the following cases:
- In the source of infection, all persons in contact with the patient are vaccinated within three days (free of charge). Unvaccinated children over one year of age are included.
- For a newborn, if anti-measles antibodies are not detected in the mother’s blood. The baby is re-vaccinated at eight months, and then according to the calendar.
- When traveling abroad, a measles vaccination must be done one month before departure. Particular attention to those traveling to Georgia, Thailand, Ukraine, where over the past 3 years many cases of measles with a fatal outcome have been recorded. Field services know how long the measles vaccination lasts. Vaccination will be noted in your documents, and this will allow you to travel abroad without fear for many years.
- Unvaccinated women who are planning a pregnancy, since during pregnancy, measles is very dangerous for the fetus.
- Persons from 15 to 35 years old who do not have proof of vaccination and if they are in risk groups (teachers, health workers, students).
How is emergency prevention of measles in children carried out?
If there is a threat of infection of unvaccinated children with this disease, emergency prevention is carried out. This procedure is carried out when the epidemic situation in a given area regarding this infectious disease worsens. Prevention can be carried out in 2 types: through the administration of measles vaccine or normal human immunoglobulin.
Use of measles vaccine
Measles vaccination is given in the first 3 days after contact with sick people.
Cultured measles vaccine live
The vaccine is given to children after one year of age who have not previously received measles vaccination, as well as to unvaccinated adults. Thanks to correct and timely emergency prevention, the disease can either be completely prevented or its course significantly alleviated.
Use of measles immunoglobulin
Children from 3 months to a year can also receive emergency vaccination with measles vaccine. But for them, a more effective way would be to administer 1 or 2 doses of human immunoglobulin. The number of doses depends on the time since contact.
Human immunoglobulin
This prophylactic agent is also used for pregnant women and people with immunodeficiency. If immunoglobulin is administered before 4 days after possible infection, this will be a very effective way of protecting against infection.
For people with immunodeficiency, the procedure is carried out regardless of previous measles vaccination.
Where is the vaccine given?
When administering the measles vaccine, you must follow some rules that every physician must know about, as well as how long the measles vaccine lasts.
For children, the drug in an amount of 0.5 ml is injected into the subscapular region or just below the middle third of the outer surface of the shoulder.
For adults, the vaccine is injected into the muscle or subcutaneously into the upper third of the shoulder. The drug is not recommended to be administered into the gluteal region due to an excess of subcutaneous fat. Intradermal contact is also undesirable. Injection into a vein is strictly contraindicated!
Vaccination of both children and adults should always be carried out with written consent. If there is a refusal to vaccinate, it must also be made in writing. The waiver must be renewed annually.
To whom?
Vaccination is indicated for children and adults who have been in contact with a patient with measles and
- have not had measles before;
- unvaccinated against measles or vaccinated once;
- have no information about vaccinations against measles
and have no contraindications to vaccination [1–4]. Read more in the article “Vaccination against measles.”
For those who have been vaccinated against measles (there is information about two vaccinations completed), emergency prophylaxis is not indicated, since these individuals are considered immune, that is, impervious to infection.
Read more about vaccination in the article “Vaccination of children against measles.”
How long does the measles vaccine last?
So, for how long after a measles vaccination is our immunity strong against this terrible disease? If we talk about adults, the average validity period lasts 12-13 years. There are cases where a period of 10 years is indicated. If we delve into this issue more deeply, it is worth saying that everything is individual. “Post-vaccination immunity” (there is such a concept) can be different for each individual, for some it will be 10 years, for others 13 or even more. There was a recorded case where a patient showed antibodies to measles already 25 years after vaccination.
It is also important to understand that if you are vaccinated, this will not provide a 100% guarantee of protection. According to the vaccine developers themselves, you simply have a much higher chance of not getting sick than those who are not vaccinated.
How long does it take for the measles vaccine to take effect? This happens as soon as your body forms immunity (antibodies) to the disease. On average, this occurs after 2-4 weeks after vaccination. Each case is individual.
Vaccination and revaccination scheme
LCV is administered intramuscularly or subcutaneously. The injection is placed under the shoulder blade, in the outer area of the thigh or shoulder. During adolescence and adulthood, the injection is given in the arm. It is recommended that children be vaccinated at the hip. The vaccination and revaccination schedule in each case is selected by the doctor individually, taking into account the person’s health condition.
According to the National Vaccination Calendar, measles prevention is carried out according to the following schedule:
- first injection – at 12 months;
- the second - at 6 years old;
- third dose – at 15-17 years.
If antibodies to the measles virus are not detected in the blood of the baby’s mother, then immunoprophylaxis of the child is performed according to the following scheme:
- first injection – at 9 months;
- the second - at 15-18 months;
- third - at 6 years old;
- the fourth – at 15-17 years old.
After vaccination given at 9 months, only 80-90% of children develop specific immunity. Therefore, six months later, the LCV is administered again. After this, the baby becomes reliably protected. At the age of 30, revaccination can be carried out.
After contact with a sick person, emergency immunoprophylaxis is performed. For this purpose, LCV is administered within the first 72 hours after the suspected infection.
Measles vaccination contraindications
We have found out how long the measles vaccine lasts in adults; now we will figure out what contraindications to the vaccine exist. The most serious ones include the following:
- It is not recommended to administer the vaccine to pregnant women. If there is a need, it is necessary to consult with specialists.
- Vaccination is contraindicated for patients with AIDS, HIV, as well as those who have diseases affecting the bone marrow or lymphatic system.
- You should not get vaccinated if any of your chronic diseases have worsened at the moment.
- If you have general ailments or diseases, also postpone vaccination.
- Vaccination is also contraindicated if it has previously caused complications for you.
- Be sure to check with your doctor to see if the medications you are taking are compatible with this vaccine.
- Allergy to egg white.
- Malignant neoplasms.
- Antibiotic intolerance.
For whom vaccination is contraindicated
Measles vaccination, despite the need for vaccination, has a number of contraindications.
It could be:
- individual hypersensitivity of the body with the risk of developing systemic allergic reactions - anaphylaxis, angioedema (Quincke). Including hypersensitivity to aminoglycoside antibiotics, quail or chicken egg white;
- severe reactions or complications from a previous vaccination;
- the presence of primary or secondary immunodeficiency conditions;
- malignant blood pathologies and neoplasms;
- pregnancy.
There are other nuances of vaccination:
- The non-anaphylactic nature of egg allergy and the presence of contact dermatitis provoked by neomycin (aminoglycoside antibiotics) are not an obstacle to vaccination.
- Measles vaccine can be administered to patients with asymptomatic HIV and AIDS infection.
- Vaccination is postponed in case of exacerbation of chronic disease until acute processes are relieved.
- In acute clinical cases of intestinal pathologies and uncomplicated forms of acute respiratory viral infections, vaccination is carried out after the temperature has normalized.
Common effects of measles vaccination in adults
Adults begin to feel the effects of vaccination on the first day. There may be pain at the injection site, redness of the skin, and some thickening. Similar symptoms are common with other types of vaccination, for example, against hepatitis B.
Further, depending on your immunity, often on the fifth, and for some on the tenth day, lethargy, fatigue, and body temperature rise. This is considered normal because your body begins to produce antibodies to measles. You need to inform your doctor about your condition, he will competently explain the cause of the ailment and fill you in on how long the measles vaccine is valid. These are the main consequences of the measles vaccine that all normal, healthy people experience.
What you need to know about measles
Measles is a serious viral disease of childhood, the main manifestations of which are fever and rash. The measles virus is easily transmitted through airborne droplets. Only humans get measles. It begins to secrete the virus 5 - 7 days before the first signs of the disease appear. After the symptoms disappear, the measles virus will be released for another 4 to 5 days.
Measles is very easy to get! Even after a short exposure of an unvaccinated child to this virus, the chances of getting sick are more than 90%!
This disease can be very mild. On average, a week after infection, the child’s body temperature rises to 38 - 39 degrees, and his health is impaired. The baby is capricious, does not play, refuses to eat, and tries to be in his mother’s arms. He develops severe weakness, cough, nasal discharge, eyes turn red, and watery eyes appear. Such symptoms can easily be confused with those of a common viral infection.
After 2 - 3 days from the onset of the disease, when examining the child’s oral cavity, white spots can be detected on the mucous membranes of the cheeks. And after some time, a rash appears on the face, which within a day spreads to the whole body. With the appearance of the rash, the body temperature rises sharply, and then it becomes clear that the child has measles. The rash lasts up to 7 days.
No drugs have been developed that will cure the disease. There are only those that will relieve the symptoms.
Only timely vaccination can protect against measles. But following the banal rules of hygiene: frequent hand washing, wearing masks, etc. are ineffective if the child lives in an area where there is an outbreak of this disease.
Side effects of vaccination
In rare cases, adverse reactions to the vaccine occur, some of which can be considered severe. You can’t do this without the help of doctors. They may be as follows:
- A toxic reaction can occur 6-11 days after vaccination. The temperature rises, a sore throat occurs, intoxication occurs, and a rash appears. The period may last five days, but it should be distinguished from any infectious diseases.
- Convulsive or encephalic reaction. High temperature and seizures. Most pediatricians do not classify these symptoms as severe complications.
- Post-vaccination encephalitis. Symptoms resemble those of other infections: dizziness, headaches, nausea, confusion, agitation, convulsions, neurological symptoms.
- Allergic reactions to vaccine components. Quincke's edema. Hives. Joint pain.
- Exacerbation of allergic diseases. Bronchial asthma.
- Anaphylactic shock.
- Pneumonia.
- Myocarditis.
- Meningitis.
After all of the above, many may have the impression that vaccination is dangerous. But that's not true. Many side reactions are formulated purely theoretically. For example, a complication in the form of encephalitis can occur once in a million. If measles occurs, the risk of complications increases thousands of times.
How long does it take for the measles vaccine to take effect? As soon as antibodies are formed in the body (from 2 to 4 weeks). If during this time you do not feel any side effects in your body, going to the doctor is not necessary.
Is it necessary to lower the temperature after vaccination?
Any vaccine is an aggressive, unfamiliar component for the body, and all its resources must be included in the fight against it.
Penetrating into the body, vaccine viruses trigger a series of complex reactions in it. The rise in temperature is evidence of their beginning.
After receiving the measles vaccine, fever usually begins a week after the procedure . But this does not always happen; each organism is unique and responds to the vaccine in its own way.
But is it worth lowering your temperature after immunization? Pediatricians believe that an increase in temperature does not benefit the child’s body, so it should be reduced with the help of special medications.
If the temperature exceeds 37.3 degrees, then the use of antipyretics is permitted. It is better to immediately take care that the temperature does not rise too high.
Only a doctor can recommend specific antipyretic drugs. Only he will be able to select them taking into account the characteristics of the vaccine recipient’s body.
Treatment of complications after vaccination
How long does the measles vaccine last? For a long time (from 10 to 13 years) you will be protected from the disease. It is worth considering that the body’s reactions, even if they occur, pass quickly, after a few days, but complications after the disease itself can be disastrous, even fatal.
- If negative reactions occur, consult your doctor.
- Symptomatic medications will help to cope with the consequences: antiallergic, antipyretic.
- If the complication is severe, it is better to treat it in a hospital. The doctor will prescribe you corticosteroid hormones.
- If bacterial complications arise, antibiotics will help to cope with them.
How is the vaccine tolerated and is it dangerous for the child?
As soon as the vaccine enters the body, a “confrontation” immediately begins in the form of the production of measles antibodies, which externally manifests itself as swelling of the puncture site (up to 5 cm) or redness (no more than 8 cm). This is the norm.
The baby may experience itching and slight pain. Most patients tolerate the procedure easily. The peak activity of clinical manifestations occurs 5-15 days after the injection.
During the post-vaccination period, the baby may be diagnosed with:
- crying and worrying;
- runny nose;
- poor appetite and sleep;
- cough or conjunctivitis;
- muscle pain (minor);
- mild skin rashes. Antihistamines will help: for children under 2 years old - Fenistil, and for older children - Claritin;
- temperature up to 39 °C. It is recommended to give your child Ibuprofen or Paracetamol.
These symptoms can last up to 2 days and then disappear. Help your baby cope with his illness, distract him with an interesting game and ensure a restful sleep. Measles vaccines are characterized by low reactogenicity, so there are almost no negative manifestations.
However, in very rare cases, the baby may develop:
- severe and extensive allergies;
- temperature over 39 °C;
- purulent abscess at the puncture site;
- hypotension and convulsions;
- long-term (more than 3 days) progression of post-injection reactions.
These cases require immediate medical supervision. Measles prevention is one of the safest.
Types of vaccines
Measles vaccine is made from live but very weakened measles viruses. In medicine, both single vaccines (for measles) and combined ones (for measles, mumps and rubella) are used. The vaccine virus itself is not capable of causing the disease in the body; it only promotes the production of measles-specific antibodies. Features of the live vaccine:
- To prevent the drug from losing its potency, it should be stored at a temperature no higher than +4 degrees.
- Unused vaccine is destroyed according to special rules.
- The composition includes egg white and antibiotics. This may cause allergic reactions in some people.
In Russian clinics, domestically produced drugs are used for vaccination - mumps-measles vaccine and measles monovaccine. Single vaccines have fewer adverse reactions.
We found out how long it takes for the measles vaccine to work, what side effects and contraindications there may be. Well, now let’s talk about how to prepare for vaccination so that vaccination is as successful as possible.
Types and names of vaccines
All vaccinations that are recorded in the national calendar are divided into monocomponent and multicomponent:
- monocomponent – contain one type of pathogen (in this case, the measles virus);
- multicomponent - contain several pathogens and can protect against various diseases at once (a common option is measles, mumps, rubella).
It is more convenient to administer a vaccine that will immediately protect against various pathogens. This will allow you to give your child just one injection and get a complex effect.
Vaccinations are divided into:
- domestic - those drugs that are traditionally offered in public medical institutions;
- imported - you can purchase it yourself and make it in a clinic or supply it in a private institution.
Names of measles vaccines:
- Cultural measles . Made in Russia. Quail or chicken protein is used as a base. The protection period reaches 18 years.
- Ruwax . The vaccine is single-component with live components. Made in France.
- Live mumps measles . The combined product provides protection against two diseases. Made in Russia.
- MMR Vaccine with live pathogens . Protects against mumps, rubella and measles at the same time. Made in America.
- Priorix . Belgian analogue of a multicomponent vaccine. Protects against measles, mumps and rubella. This option will be preferable for patients who want to simultaneously immunize against hepatitis, polio, tetanus, whooping cough and diphtheria.
Using an injection, a weakened infectious agent is introduced into the patient's body. The immune system recognizes it and destroys it. As a result of contact, protective antibodies are formed, which subsequently protect the person upon repeated contact with the virus.
Expert opinion
Irina Katykova
Pediatrician, pediatric neurologist
Ask a Question
Do you still have questions about your child's health? Ask them right here on the website and we will definitely answer!
What's the best way to get vaccinated?
- You need to come for vaccination absolutely healthy, without any signs or manifestations of ARVI.
- Before vaccination, ideally you will visit a doctor and undergo all general tests.
- After the vaccine is administered, avoid visiting crowded places for three days to avoid contracting any foreign virus.
- Is it possible to swim? Yes, but do not rub the injection site. It's better to take a shower rather than a bath.
- After vaccination, you should not introduce any new foods or dishes into your diet, so as not to provoke allergic reactions.
How long does the measles vaccine last? For more than ten years in your life you can be calm. A terrible disease is unlikely to affect the body, because thanks to vaccination you have developed a strong immunity to measles.
Instructions for use of measles vaccines
Any measles vaccine (according to the instructions) requires a single subcutaneous or intramuscular injection.
Before use, the lyophilized drug is diluted with a sterile solvent. Each dose contains more than a thousand viral units of the measles strain. This applies to both single vaccines and combination drugs.