General information about rhinocytogram
The internal cavity of the nose is covered with a mucous membrane with a special secretion that helps remove dust and microorganisms that have entered the nose. Some microbes, in certain quantities, are normally permanent inhabitants of the nasal mucosa. While a person is healthy, his immunity inhibits the increase in the number of microorganisms. As soon as it weakens, the active growth of the pathogenic environment begins. Inflammation of the mucous membrane, disruptions in the normal functioning of the nose, runny nose - symptoms of acute rhinitis.
Causes of rhinitis: decreased general immunity, airborne viruses, acute respiratory infections, allergic reactions. A rhinocytogram (nasocytogram) is a microbiological examination of a smear from the nasal passage. The number of lymphocytes, red blood cells, macrophages, yeast fungi, neutrophils, eosinophils, leukocytes (basophils and other cells), monocytes and ciliated epithelial cells is assessed. This helps to determine the nature of the disease: infectious, allergic or vasomotor.
Nasal swab for eosinophils is normal in children interpretation
The nasal passages and sinuses are one of the main barriers to infections, allergens and other irritants of the respiratory system. A runny nose is a standard safe reaction to infectious inflammation or hypothermia, but its prolonged course and the lack of effectiveness of symptomatic therapy should alert the patient or his parents.
A special study - a rhinocytogram - helps to establish the cause of a prolonged runny nose: the norm in children (in deciphering the analysis result) and adult patients is a small number of immune cells and the absence of pathogenic microorganisms.
Interpretation and norm of nasal swab for eosinophils
The mucous membrane of the human nasal passages and sinuses is inhabited by representatives of opportunistic microflora. The characteristic “opportunistic” means that bacteria with normal immunity are harmless to humans.
However, the weakening of the body's defenses creates favorable conditions for the proliferation of opportunistic microorganisms and the development of the inflammatory process.
To protect against pathogens and dust, the human nose secretes special mucus with antiseptic proteins.
Source: https://dou99.ru/nos/mazok-iz-nosa-na-eozinofily-norma-u-detej-rasshifrovka
Indications for analysis
Doctors prescribe a study of the microflora of the nasal mucosa when the patient complains of a long-term (more than a week) runny nose. At the same time, the medications used do not give a good effect. In this case, an accurate understanding of the nature of the disease and the type of pathogen helps to select an effective and correct treatment, and not to act at random with conventional vasoconstrictor drugs. It makes sense to conduct an analysis in case of frequent relapses of respiratory diseases.
The need to conduct a rhinocytogram increases if the patient has additional complaints against the background of a severe runny nose: frequent sneezing, itching of the mucous membrane of the nasal passages . Doctors identify a risk group - patients who are more susceptible to complications and risks than others. These are young children, people with a weakened immune system, diabetes mellitus, and patients after surgery (especially after internal organ transplantation).
During AR there are several stages:
- vasotonic , characterized by periodic nasal congestion associated with disturbances of vascular tone, and requiring occasional use of decongestants;
- vasodilation , characterized by frequent nasal congestion, accompanied by dilation of the vessels of the nasal mucosa and requiring frequent use of decongestants;
- stage of chronic edema , characterized by constant nasal congestion, the nasal mucosa becomes bluish in color, the use of decongestants is ineffective;
- hyperplasia , characterized by constant nasal congestion, proliferation of the nasal mucosa, and the formation of polyps; often the paranasal sinuses are involved in the process, secondary otitis develops, and a secondary infection occurs; the use of decongestants is ineffective.
Preparation for a rhinocytogram
To obtain correct nasocytogram results, there are a number of requirements that should be observed before taking a smear. First of all, do not take medications with antibiotics for 5 days before the procedure. Immediately before the test, you should not use antibacterial drops, spray, or nasal ointment for at least two hours. It is recommended not to rinse your nose several hours before the procedure (including solutions with sea water), not to brush your teeth, and to drink only clean water. If these rules are not followed, the result may be distorted.
- Cupcake Recipes
- High blood pressure - what to do. First aid and how to reduce blood pressure with drugs and folk remedies
- Ultrasound of the bladder
Neutrophilic leukocytes: causes of appearance in a smear, normal, possible diseases, treatment options
Today, in order to determine whether there is an inflammatory process or blood disease in the body, you just need to do a cytological smear or blood test. Neutrophilic leukocytes and their number in the analysis results can indicate some changes in the body. In order to understand this topic in more detail, this article was created.
Neutrophils. What is this?
Neutrophil leukocytes, or as they are also called neutrophil granulocytes, are a type of white blood cell. They look like white blood cells, their important function is to protect the body from the effects of bacterial infections, as well as support the human immune system itself.
The place of neutrophil maturation is the bone marrow, then they “migrate” into the blood, and their speed is 7 million per minute. Neutrophils circulate in the blood for 8 hours to 2 days, after which they move into tissues, where they perform their main function - protecting the body. In these same tissues, neutrophils die.
Neutrophils are the most significant and quite numerous of all subtypes of leukocytes in the blood, and their percentage is 45-70% of leukocytes, the diameter of which is 12-15 microns.
Neutrophilic leukocytes perform the “ambulance” function. They pick up “inflammatory signals” and immediately move to the site of the lesion. Inflammatory reactions can occur as a result of burns, wounds, ulcers, injuries, etc. A decrease in the level of neutrophils occurs as a result of the presence of a virus and parasitic infestations in the body.
Kinds
Neutrophil granulocytes in the blood are divided into two types according to the shape of the nucleus:
- Band neutrophil leukocytes - have the shape of a horseshoe-shaped nucleus, are considered immature or young neutrophils.
- Segmented neutrophil granulocytes are a mature form of neutrophil with a segmented nucleus. They are also called “heroic” because when they encounter microbes they absorb them and die.
In order to determine the condition of the human body, experts compare the percentage of mature and young neutrophils.
It is known that in newborn children there is an increased number of band neutrophils, but later such cells are replaced by segmented representatives.
And after three weeks of the child’s life, the balance between mature and young cells is equalized.
The norm of neutrophil leukocytes in the blood varies according to age criteria, but there are no differences according to gender.
The norm table is presented below.
| Age | Average rate | |
| Band neutrophils | Segmented neutrophils | |
| Newborns/infants | from 1 to 5% | from 27 to 55%. |
| Children under 5 years of age | from 1 to 5% | from 20 to 55% |
| Children under 15 years of age | from 1 to 4% | from 40 to 60% |
| Adults | General indicator from 45 to 70% |
In order to determine the amount of neutrophils in the blood, doctors prescribe a detailed blood test.
Rhinocytogram
A rhinocytogram is a study that is carried out using a smear from the nasal cavity to clarify inflammatory processes in the nose or other diseases. This diagnosis is especially important to prevent the progression of allergic rhinitis.
So, what will this study reveal:
- allergic cause of inflammation of the nose;
- conduct diagnostics to screen out other causes of rhinitis;
- prevent the progression of allergic reactions;
- choose the appropriate treatment in time;
- prevent the development of complications.
Before carrying out such a diagnosis, you should not rinse your nose or use other means for it.
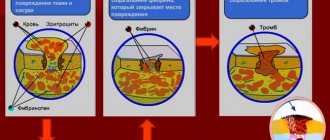
Based on the results of a study of the ratio of eosinophils and neutrophil leukocytes in a nasal smear, the intensity of the allergy or infection can be determined:
- If there are more neutrophils in the microflora, it means that there are bacterial infections in the nasal cavity and in the body as a whole. An increased level of neutrophils is especially characteristic during the period of acute illness.
- If there are more eosinophils (more than 10%), it means that the person has acute allergic reactions.
- An excess number of neutrophils and eosinophils indicates allergic rhinitis, which is complicated by secondary infections.
- A small number or absence of neutrophils and eosinophils will indicate the presence of vasomotor rhinitis.
Pathological causes of low neutrophils
Reduced neutrophil leukocytes in a smear may be due to:
- peptic ulcer;
- various viral diseases;
- bacterial infections;
- purulent inflammation;
- anemia;
- protozoal infections;
- agranulocytosis;
- typhus, etc.
Not only diseases can lead to a decrease in neutrophils in the blood, but also the condition of the person himself:
- after administration of the vaccine;
- due to chemotherapy;
- as a result of a serious illness;
- with drug therapy;
- due to anaphylactic shock;
- after radiation therapy;
- due to living in a poor ecological area.
In addition, there are a number of other factors that can affect the level of neutrophil leukocytes: excessive physical activity or a congenital feature (the level of neutrophils from birth is below normal).
Pathological causes of elevated neutrophils
Elevated neutrophilic leukocytes in cytology may mean that there is an inflammatory process in the body. The latter are generalized and localized in appearance.
Generalized is the defeat of the entire body by such severe infections as, for example, cholera and sepsis.
Localized inflammation is inflammation that is concentrated in one place or area of the human body, for example: sore throat, purulent wounds, pyelonephritis, pneumonia, etc. An increased level of neutrophils is observed as a result of such pathologies:
- diabetes mellitus;
- burns;
- cancerous tumors;
- dermatitis and other skin diseases;
- disorders of the genitourinary organs;
- gangrene;
- exposure and damage to toxic substances in the body.
Exceeding the normal level of neutrophils in the blood may be a temporary manifestation that was caused by external factors.
These include psycho-emotional stress, stress, excessive physical activity, administration of a vaccine or other medications.
In order for the test results to be as reliable as possible, you need to get rid of all these factors before laboratory diagnosis.
Due to various types of diseases and viruses, the chemical elements in the blood change, which allows doctors to determine the exact disease using tests.
Neutrophil granulocytes can be elevated due to a variety of reasons, but the fact that there is a deviation from the norm forces a complete examination of the human body.
Such diagnostics are carried out taking into account all possible factors that negatively affect the body.
Features of the neutropenia process
Neutropenia is a condition when neutrophilic white blood cells are low in the blood. It has already been said above that neutrophils react to foreign bodies in the body and in every possible way protect and keep the immune system in order.
That is, when neutrophils detect an infection in the body, they form a “block” around the inflammation, thereby creating obstacles to the further spread of foreign agents.
The result of such a struggle between neutrophilic leukocytes and infection will be the formation of pus in the wound, inflammatory and intoxication syndrome.
The disease can be hidden if the person initially has neutropenia, but because of this, the infection can spread throughout the body and lead to sepsis. The first clinical manifestations of neutropenia may be:
- stomatitis;
- gingivitis;
- purulent sore throat;
- osteomyelitis;
- abscess;
- sepsis.
Those patients who are susceptible to neutropenia should avoid contact with other sick people, and they are also not recommended to be in a place where there are large crowds of people. Every year it is necessary to carry out planned prevention of seasonal diseases. In addition, microbes that are completely safe for the average person can adversely affect the health of patients with neutropenia.
Treatment for neutrophilia
If neutrophilic leukocytes are elevated (from the nose in a smear, for example), you first need to identify the reason why this is happening. This should be done, since there are no direct means that will help reduce neutrophils.
Below is a list of actions to take if neutrophilia (increased number of neutrophils) is observed:
- It is imperative to visit a general practitioner and provide him with test results, as well as tell him about the presence of certain symptoms.
- In order to confirm the accuracy of the tests, you need to take them again, while following all the rules for preparing for diagnosis.
- If neutrophilia is nevertheless confirmed, then the next step will be a complete diagnosis of the body to detect inflammatory diseases.
- After a detailed diagnosis, specialists, in accordance with the disease, prescribe drug therapy:
- antibiotics;
- immunostimulants;
- sedatives;
- corticosteroids;
- cleansing the blood of excess leukocytes.
Treatment for neutropenia
If the neutrophil leukocytes in the cytology smear are below normal in the same way as in the case described above, the cause needs to be determined. But very often, after a person has suffered an infection and recovered, neutrophils begin to recover on their own. As a rule, treatment for neutropenia is aimed at getting rid of the primary factors. These types of drugs are usually prescribed:
- leukopoiesis stimulants (moderate effect);
- “Pentoxyl” (moderate effect);
- “Methyluracil” (moderate effect);
- “Filgrastim” (strong effect);
- “Lenograstim” (strong effect).
Who to contact?
If there is a deviation from the norm in the tests, you should contact the following doctors:
- therapist;
- immunologist;
- hematologist,
- allergist.
If there is an accumulation of neutrophilic leukocytes, doctors can not only prescribe therapy, but also recommend adhering to the following instructions:
- stop drinking alcohol and smoking;
- healthy sleep;
- correct daily routine;
- drink about 2 liters of water per day;
- do light sports;
- eliminate stress and other emotional stress;
- rational nutrition (5 times a day) in small portions;
- consumption of vitamins.
Source: https://FB.ru/article/416514/neytrofilnyie-leykotsityi-prichinyi-poyavlenie-v-mazke-norma-vozmojnyie-zabolevaniya-variantyi-lecheniya
Carrying out the procedure
The collection of mucus for examination is carried out with a cotton swab, with which the nurse takes the material from one and the other nostril. Manipulation time is a few seconds. The patient only needs to tilt his head back slightly. The process is absolutely painless, even small children do not need anesthesia. Samples for analysis are examined under a microscope, some are placed in a special container. It contains a nutrient medium that promotes the growth of microorganisms present in the material.
In some cases, when sinus inflammation is suspected, a more precise analysis is required. The material is taken deeper, the process is controlled by an endoscope video camera. This will require local anesthesia. The study determines the composition of the microflora, studies its susceptibility to antibiotics of different groups, and makes an accurate diagnosis in order to prescribe the correct treatment.
myLor
Determining the cause of a prolonged runny nose that cannot be treated with conventional nasal and antibacterial agents can be quite difficult. It is believed that a frequent runny nose in a child is a completely common and understandable phenomenon, especially if he attends kindergarten or school.
But when a runny nose lasts for weeks or months (and this happens not only to children), this may indicate the allergic nature of rhinitis. As an analysis that can confirm the allergic etiology of the runny nose, a rhinocytogram procedure, or a nasal smear for eosinophils, is used.
Why is an analysis taken from the nasal mucosa to determine the number of eosinophils?
The fact is that increased eosinophils in a scraping or smear from the nasal mucosa are most often observed with allergic rhinitis. Therefore, the transcript of this study is used as an argument confirming the allergic nature of prolonged rhinitis.
The treatment of allergic rhinitis is fundamentally different from the treatment of infectious rhinitis, so a smear test for eosinophils is crucial. A smear test is indicated when a runny nose lasts more than 2 weeks and there is a suspicion of swelling of the nasal mucosa or allergic inflammation of the sinuses.
The material is collected using sterile swabs and a cotton swab.
When examining the nasal mucosa, the cytological picture is analyzed, represented by the ratio of blood cells and microorganisms present in the material. The composition of a healthy biomaterial usually includes:
- leukocytes;
- neutrophils;
- lymphocytes;
- macrophages;
- red blood cells;
- yeast mushrooms (in small quantities);
- streptococci and staphylococci (in small quantities);
- mucus and other microflora.
Under certain conditions, eosinophils are detected, the number of which can be used to judge the presence of pathology.
In addition to the number of eosinophils, which is determined by staining mucus with a special Romanovsky-Giemsa substance during examination under a microscope, other fractions of the blood composition and leukocyte formula are analyzed:
- red blood cells - a certain number of red blood cells in a nasal smear indicates increased permeability of the walls of the vessels of the nasal mucosa, characteristic of influenza, diphtheria and other infections;
- if lymphocytes are elevated, chronic infectious inflammation of the nasal mucosa can be assumed;
- neutrophils - an increased amount of this fraction usually indicates an acute viral or bacterial infection, which caused prolonged rhinitis.
Finally, a significant increase in the number of eosinophils suggests an allergic nature of the runny nose; a high level of eosinophils (both in nasal mucus and in blood tests) is also characteristic of the presence of polyps in the nasal cavity.
If leukocyte fractions are absent in a smear of the nasal mucosa, this may indicate the development of vasomotor rhinitis (not caused by either infection or allergy), chronic rhinitis due to addiction to vasoconstrictor nasal drops (sprays) or rhinitis provoked by a violation of the anatomy of the nasal passages or a violation hormonal balance.
Normally, the number of eosinophils in a smear from the nasal cavity should be zero, that is, they should not be present in healthy nasal mucous membranes.
If, during the analysis of nasal secretions, at least single eosinophilic leukocytes are detected, it means that some pathological process is beginning or already occurring in the body. Ordinary inflammation of the mucous membrane can lead to an increase in the number of eosinophils 1:10 in relation to neutrophils.
A significant excess of the norm of eosinophils in the nasal mucosa (with normal levels of this fraction in the blood) in almost 100% of cases indicates an allergic etiology of the runny nose. An increase in eosinophil levels of 10% or more is considered significant. In children 1-13 years old, the threshold for normal levels ranges from 0.5% to 7%. This deviation from the norm is characteristic not only of allergic rhinitis, but also of some other conditions.
Eosinophilia observed in a smear from the nasal cavity indicates a disruption in the normal balance of blood cells in the mucous membrane. This condition may be caused by:
- allergic respiratory diseases;
- non-allergic respiratory diseases (eosinophilic rhinitis);
- periarteritis nodosa - a pathology accompanied by inflammation and necrosis of the middle muscular arteries;
- bronchial asthma;
- ascariasis and other helminthiasis (most common in children);
- leukemia (characterized by an increased level of eosinophilic leukocytes in the blood);
- parasitic infestations (giardiasis, opisthorchiasis, echinococcosis, toxocariasis, trichinosis).
Based on a single analysis of a smear from the nasal mucosa, a diagnosis, of course, is not made, but this study makes it possible to detect pathology (including allergies) at the initial stage of development.
Test results may be affected by the use of nasal drops or sprays containing corticosteroids.
False-negative results for eosinophilia can also be observed when taking medications with corticosteroids or drugs that have antihistamine (antiallergic) properties. Therefore, the use of these drugs on the eve of taking a nasal swab is not recommended. In order to clarify the results, a repeat study is usually carried out after 1-2 weeks.
A rhinocytogram can be called one of the most painless collections of biomaterial for research, so assigning this procedure to a child should not alarm or upset parents. Pathology detected in time is much easier to eliminate, so it is better to promptly check the child for the presence of helminths or allergic manifestations. This will allow you to choose the right treatment strategy and prevent possible complications.
Inflammation of the nasal mucosa, swelling, reproduction of transparent muconasal secretion indicates a violation of the integrity of the upper and lower respiratory tract. Catalysts for irritation of the inner shell are external factors such as dust, pet hair, spores of seasonal plants, tobacco smoke, household chemicals, and infectious agents.
In order to competently draw up a therapeutic regimen, it is advisable to identify the genesis of rhinitis through research. If an allergic rhinitis is suspected, the doctor will prescribe a rhinocytogram procedure to confirm or refute the etiology of the snot.
Eosinophilic granulocytes, as a subtype of leukocytes, are present in every organism in limited numbers . They promote tissue regeneration, develop immunity against parasitic worms, exhibit phagocytic activity, and slow down the growth of tumors.
Immune cells are formed from the building material of the brain. The formation process takes up to 4 days , after which eosinophils leave the central nervous system and circulate in the blood. The final stage is the localization of granulocytes in the skin, digestive system, and liver, where the duration of their life cycle varies from 8 to 12 days .
For reference! The number of cells in the body can be identified based on the results of a blood test, scraping from the nasal cavity and pharynx.
There are no specific figures for the content of eosinophils in mucus ; it all depends on the strength of the allergen or parasitic agent. The number of blood cells changes under the influence of hormones, medications, and the development of pathological processes.
The norm of leukocytes in a child’s nose is measured by a single number of neutrophils and lymphocytes, the rate of which should not exceed 5% . In case of allergies, granulocytes can appear in large quantities in the lymph and accumulate in muconasal mucus.
The size of the eosinophil in the lymph is 12 µm, after migration into the connective tissue it increases to 20 µm
When the mucous membrane is irritated, the immune system produces a protective secretion with an increased or decreased concentration of white blood cells . There are several types of leukocytes: neutrophils - perform a protective function in case of bacterial damage, lymphocytes inhibit the synthesis of foreign structures of viral origin.
When the body is sensitized to antigens, eosinophils also appear on the mucous membrane.
A nasal swab for eosinophils allows you to determine the etiology of the disease, stage of development and reactivity of the body .
Indications for microscopic cytological examination are patient complaints:
- respiratory disorders;
- prolonged secretion from the nose, sneezing;
- lacrimation;
- itching;
- swelling.
A scraping is taken from the posterior part of the inferior nasal sinus , the discharge is painted over with acidic inhibitors, which affect the heterogeneity of blackening of the photographic material. Eosinophils acquire a red color and become available for counting under a microscope.
Collecting mucus from a child requires special care so as not to damage the fragile epithelial layer and blood vessels.
Steroid hormones produced by the adrenal cortex change the concentration of eosinophils in the body. Therefore, the day before the examination, it is advisable to limit the intake of antihistamines and vasoconstrictor drops .
It is optimal to carry out a nasal test in the morning , when the cell level decreases by 20% of the daily norm.
Rhinocytogram is a non-invasive research method (does not violate the integrity of the inner lining of the nose)
The optimal number of granulocytes is measured by their percentage to the total number of cells. The norm in children under 13 years of age varies between 5-7% eosinophils, in adults – from 0.5 to 5% .
These indicators are considered to be reference ones, because With age, the concentration of leukocyte growth cells decreases. Their content in mucus and sputum should be minimal .
For reference! In women, at the beginning of ovulation and the end of the menstrual cycle, the rate of leukocytes in the blood decreases, and before the onset of menstruation, it increases.
With pathological changes, the eosinophil index is disrupted; the higher the coefficient, the more serious the stage of the disease . With a mild degree, the percentage of immune cells reaches 10%, moderate up to 15%, severe - over 15%. An increased number of eosinophils has the medical term “eosinophilia.”
Analysis of snot, where an increased number of granulocytic cell groups is noted, indicates pathologies of allergic origin . When exposed to allergens, the immune system becomes vulnerable, the mucous membrane produces substances that cause allergy symptoms.
Neutrophils in a nasal swab with an increased number of eosinophils signal a bacterial infection . An elevated level may be the result of bronchial asthma, the formation of a malignant tumor, or the presence of helminths.
An increase in the indicators of leukocyte lineage cells in infants is a consequence of intrauterine infection, skin dermatitis, and an allergic reaction to cow's milk.
For reference! Snot analysis is repeated after 3 days. If the results are identical, then we can judge the reliability and accuracy of the survey.
Less commonly in the clinical picture, eosinophilia causes serious pathological disorders :
- leukemia . Hematological disease is manifested by a sharp development of heart failure against the background of damage to granulocytes, platelet and erythrocyte lineages in the bone marrow;
- periarteritis nodosa . An autoimmune process in which the immune system perceives its tissues as foreign and attacks them, resulting in necrosis of the middle arteries of the muscular type. Patients complain of fever, pain in the abdomen, kidney failure, skin rashes;
- parasitic infestations . The patient is actively infected with parasitic worms of various types. They enter the body through intact or damaged skin.
During pregnancy and after recent surgery, a rhinocytogram may not detect the presence of eosinophilic granulocytes
The reason for the increase in the level of leukocyte lineage cells is a decrease in local immunity due to intoxication of the body, hypothermia, and activation of pathogenic strains.
Reduced levels of eosinophils are characteristic of the development of sluggish pathological processes under the influence of viruses and bacteria . The absence of leukocyte lineage cells in the smear indicates the development of vasomotor rhinitis.
Against the background of hypersecretion, a decrease in the number of red blood cells, leukocytes and platelets in the nasal mucosa is observed.
If the indicators are normal and the symptoms of rhinitis are not relieved, then the formation of secretion is associated with long-term use of vasoconstrictor drugs , hormonal changes, anatomical changes in the nasal passages, and destabilization of the patient’s psycho-emotional state.
To identify the allergic or infectious nature of inflammation of the nasal mucosa, doctors prescribe a rhinocytogram. Its indicators are taken as the basis for drawing up a therapeutic regimen.
Acute respiratory viral infections, autoimmune processes, allergic manifestations, helminthic infestations lead to an increase in the growth of eosinophils in the mucous membrane of the ENT organ. Decreased values most often indicate progression of vasomotor rhinitis.
When a runny nose bothers you, a person has to deal with more than just local symptoms. Lack of oxygen due to impaired nasal breathing causes fatigue, decreased attention and headaches, which negatively affects the quality of life. Allergic rhinitis is accompanied by much more unpleasant symptoms, and if a child is sick, then redoubled attention to the problem is required.
To effectively cure a runny nose, you need to undergo high-quality diagnostics, which necessarily includes a nasal smear for cytology. Why is it needed, how and to whom is it carried out, what are the standards of analysis - these questions worry many. But only a competent specialist can answer them.
The nasal cavity is an important element of the respiratory tract. It is lined with mucous membrane covered with ciliated prismatic epithelium. The goblet and glandular cells located in it produce a secretion containing many useful substances. The mucus contains antimicrobial components: lysozyme, immunoglobulins and interferon, lactoferrin, enzymes, etc. The membrane itself contains macrophages and lymphocytes that absorb foreign agents, thereby inducing an immune response.
The movement of the epithelial cilia helps remove harmful particles (dust, aerosols, microbes) that have entered it from the nasal cavity. The air, passing through the initial section of the respiratory system, is not only purified, but also moistened and warmed. Therefore, the secretion of the mucous membrane plays an extremely important role in maintaining the normal state of the respiratory tract.
In the medical community, a nasal swab is called a rhinocytogram. The study is based on an analysis of the cellular composition of nasal secretions. This is necessary to determine the cause of the runny nose. Most often, cytology is performed for prolonged rhinitis (more than 2 weeks), especially in children. If the prescribed drugs do not help, then it is necessary to clarify the origin of the pathology and repeat the differential diagnosis.
The most common types of rhinitis are infectious, allergic and vasomotor. They can also become chronic when the symptoms last for a long time. Allergies occupy a special place among the causes of runny nose. Sensitization of the body to foreign antigens leads to seasonal or year-round runny nose, which is manifested by the following symptoms:
- Copious discharge of watery mucus.
- Nasal congestion.
- Paroxysmal sneezing.
- Itchy feeling in the nose.
This process is based on hypersensitivity reactions (usually immediate type). When faced with an allergen, macrophages engulf it and present it to B lymphocytes. Those, in turn, begin to synthesize class E immunoglobulins, which are deposited on mast cells and eosinophils. And upon repeated contact with the same agent, allergy mediators are released: bradykinin, histamine, serotonin, prostaglandins and leukotrienes. Vascular permeability increases, which leads to swelling, hypersecretion of mucus and other symptoms of rhinitis.
That is why a rhinocytogram becomes a key parameter in the differential diagnosis of a runny nose. By making a nasal swab for eosinophils, it will be possible to establish the cause of the pathology, confirming or denying its allergic origin. Indeed, according to statistics, a fifth of the population suffers from such rhinitis.
Analysis of nasal swabs is done in cases where it is necessary to find out the exact origin of rhinitis. Treatment measures will depend on this.
Before taking a smear for eosinophils, it is worth making preliminary preparations. Before taking biomaterial, the patient is not recommended to:
- Blow your nose thoroughly.
- Toilet the nasal cavity.
- Use drops and sprays with vasoconstrictors and topical corticosteroids.
- Use hygienic creams and ointments.
- Take antiallergic and hormonal pills.
Thus, it is contraindicated to do anything that changes the composition of nasal secretions. Indeed, in this case, the result may turn out to be unreliable. The analysis is prescribed by a general practitioner, family doctor, otolaryngologist or allergist after a clinical examination and rhinoscopy. The patient is given a referral to a laboratory (for example, Invitro or others).
https://youtu.be/jnHwQ72xQvE
It is not difficult to make a rhinocytogram. Nasal swabs for eosinophils are taken by nursing staff working in laboratories. To do this, you need special sterile tuffers, which are passed along the mucous membrane. The procedure is completely painless and non-invasive.
The resulting biomaterial (nasal secretion) is applied to a glass slide and stained according to Romanovsky-Giemsa. Some structures acquire a blue tint (cytoplasm of lympho- and monocytes, basophil and neutrophil granules), while others become pink (eosinophil granules, leukocyte nuclei). Next, the cellular elements are counted under a microscope.
The results of a cytological examination should be interpreted in combination with other signs of pathology. For a more reliable result, it is recommended to repeat the analysis after a couple of days. Having received a form with the identified indicators, the doctor evaluates them in accordance with the reference values. And only he can make the appropriate conclusion.
In a nasal smear for eosinophils, the cell norm depends on age. For a child under 13 years of age, this value should not exceed 7%, and for older children and adults – 5%. The lower limit is at 0.5%. But rhinocytology allows us to identify other cellular elements (Table No. 1):
But it should be noted that reference values may also depend on the location from which the smear was taken. Therefore, when conducting analysis, it is important to adhere to established techniques. Each laboratory (Sinevo, Invitro and others) indicates normal values in the form next to the actual ones. And the patient, just like the doctor, can compare them.
Normal cytology indicates no changes in the mucous membrane. But the presence of clinical signs should be the basis for repeating the analysis.
An increase in cellular elements in the smear indicates a pathological process affecting the nasal mucosa. The origin of violations can be judged by what indicators go beyond the norm.
If more than 10% of eosinophils are detected in a child or adult, then one has to think about the allergic nature of the runny nose. But a similar phenomenon is often observed in other diseases with signs of immune disorders in the body:
- Eosinophilic rhinitis (polyposis).
- Periarteritis nodosa.
- Leukemia.
- Helminthic infestations.
In addition, eosinophilia alone cannot be a sufficient basis to confirm allergic rhinitis. As a rule, additional diagnostics should be carried out with a general blood test (these cells are also elevated in it) and determination of the level of immunoglobulins. Often it is necessary to identify the specific antigen to which sensitization occurred (allergy tests).
It should be noted that the level of eosinophils in the secretion correlates with the severity of the pathological process. The allergic reaction is also accompanied by a parallel growth of basophils and mast cells. The mentioned dependence is reflected in table No. 2:
Neutrophilia in biological environments indicates the infectious nature of the pathology. These cells are the first to penetrate the site of inflammation, and therefore are most characteristic of acute rhinitis. With a chronic runny nose, their level is much lower, but still exceeds the norm. As a rule, we are talking about bacterial damage to the mucous membrane, but viral agents also provoke the growth of neutrophils.
Lymphocytic infiltration of the nasal mucosa is characteristic of acute viral inflammation and prolonged runny nose. Chronic rhinitis is often accompanied by hyper- or atrophic changes. Prolonged inflammation is certainly accompanied by a reaction from lymphocytes, since they are the main cellular elements of local defense. But their number does not grow as quickly as neutrophils.
When a cytology smear shows the content of red blood cells, one can think about increased permeability of the vascular wall or deeper damage to the mucous membrane. This is possible with influenza, diphtheria, atrophic rhinitis (ozena), and ulcerative lesions of the nose. These situations require a more serious approach to diagnosis.
An increase in cellular elements in the rhinocytogram indicates a pathological process of allergic or inflammatory origin.
If the analysis indicates a decrease in formed elements in the nasal secretion, then you have to think about a different nature of the runny nose. Most likely, inflammatory and allergic processes are not the cause of the symptoms, but it is worth thinking about vasomotor (neuroreflex) rhinitis, which occurs due to the irrational use of vasoconstrictor drops, with hormonal and psycho-emotional disorders, and anomalies of the nasal passages.
A rhinocytogram is an important element in diagnosing a runny nose. And the determination of eosinophils in a smear allows us to assume with a high degree of certainty the allergic nature of rhinitis. But the doctor will not limit himself to just analyzing nasal mucus, but, most likely, will prescribe additional studies to the patient to clarify the nature of the process. After all, the effectiveness of treatment depends on the correct diagnosis.
Inflammatory processes occurring in the nasal cavity are a very big problem for children. It happens that parents carry out incorrect treatment of chronic rhinitis, since there are many varieties of this disease and each requires the use of a specific therapy technique.
It is very important to carry out diagnostics to make a diagnosis. For this purpose, a rhinocytogram is performed. Deciphering a nasal swab will allow you to determine the presence of the disease and identify the features of its course.
A rhinocytogram is a comprehensive analysis of the microflora of the nasal sinuses. To do this, a nasal swab is taken to obtain nasal secretions. This research method involves assessing the number of cells such as:
- lymphocytes;
- red blood cells;
- neutrophils;
- ciliated epithelium;
- macrophages;
- yeast mushrooms;
- eosinophils.
By conducting research, it is possible to determine which bacteria provoked the occurrence of a runny nose in order to carry out the most successful fight against it.
A rhinocytogram is an analysis of a smear taken from the nasal mucosa. The procedure is prescribed for adults and children. Often, such an analysis is prescribed for people who have a long-term persistent runny nose or frequent relapses of respiratory tract infections.
High-risk groups include:
- children;
- people with weakened immune systems;
- have undergone organ transplantation;
- people with diabetes.
This study is mandatory if the patient has one or several complaints, namely:
- nasal congestion lasting more than a week;
- nasal discharge that cannot be treated;
- sneezing;
- itching of the nasal mucosa.
This is a fairly simple analysis that does not cause any discomfort to the child.
Many patients wonder how to do a rhinocytogram and how to prepare for the study. To obtain accurate results, you must follow certain rules. Two days before the test, you need to stop using various ointments inside and outside the nose. It is prohibited to use drops and sprays containing antibacterial components and corticosteroids.
5 days before sampling, you must stop taking antibiotics. There is no need to rinse your sinuses the day before taking a smear, and on this day it is advisable not to brush your teeth and drink only water.
A rhinocytogram in a child and an adult is performed at any time, but it is best to do this in the initial stages of the disease. The analysis is carried out in a fairly simple way. The procedure is completely painless, and even children do not need to be afraid of it.
To collect material, the patient tilts his head back slightly, and the doctor or nurse uses a cotton swab to take the required amount of material for the study. The exact same procedure must be done with the other nostril. The resulting samples are then placed in a special container with a special nutrient medium required for the growth of microorganisms.
Often, the doctor may use an endoscope to obtain a more accurate result. This study is performed under local anesthesia. This type of sampling of material for analysis causes some discomfort, since it is carried out from the paranasal sinuses. The resulting material is considered more informative, since it can be used to determine the presence of neutrophils in the smear.
A qualified doctor must describe the result obtained, since he knows how to decipher the analysis (rhinocytogram). The nasal mucosa consists of several cells, each of which performs a specific function. If bacteria or viruses enter the mucous membrane, the level of leukocytes increases to combat them. These cells are involved in the formation of immunity.
An increase in leukocytes indicates the presence of infection in the body, and an excess of one of the leukocyte fractions indicates the cause of the disease. When allergens come into contact with the surface of the nasal mucosa, an allergic reaction occurs. It is caused by the formation of eosinophils on the surface of the mucosa. In addition, during the study, epithelium and bacteria can be detected.
When conducting research, it is imperative to know what the normal rhinocytogram is in children. The interpretation in the table allows you to determine the normal indicators of the components of discharge from the nasal sinuses for adults and children.
| Components | Norm in percent |
| Eosinophils | 0-5 |
| Neutrophils (rods) | 1-6 |
| Neutrophils (segment.) | 47-72 |
| Macrophages | 3-11 |
| Leukocytes | 65-75 |
The content of these cells is not constant; it can fluctuate throughout the day. In the morning or evening, this figure can decrease by about 20%, and at night it can increase by 30%.
When deciphering a rhinocytogram, the norm for eosinophils in children under 4 years of age should be 0-7, and in children over 4 years of age, the indicators for adults are taken into account. The rest of the test indicators depend on the age of the child, so the doctor must interpret the results.
To determine the main cause of a prolonged, persistent runny nose, the quantitative ratio between the cells is calculated during the follow-up. When analyzing a rhinocytogram (deciphering), normally in children there should be up to several units of leukocytes in the field of view. During the course of the infectious process and inflammation, their number increases sharply.
Normally, neutrophils should be 1-3%. In the presence of a bacterial type of runny nose, frontal sinusitis or sinusitis, their number increases sharply, in proportion to the intensity and complexity of the inflammatory process. This manifests itself in the appearance of thick yellow or green nasal discharge. Initially, a viral infection can be complicated by a bacterial one, which is why the number of neutrophils can increase simultaneously with lymphocytes.
Deciphering the (normal) rhinocytogram in children suggests that lymphocytes should not exceed 5%. A sharp increase in the level of lymphocytes may indicate the presence of influenza, parainfluenza, adenovirus or any other viral infection. In addition, their number may increase with chronic runny nose.
The presence of more than 10% eosinophils in the tests indicates the presence of hay fever, or allergic rhinitis, in the body. The amount of epithelium is not always taken into account when conducting research, but a significant amount of it indicates an inflammatory process occurring in the body.
When deciphering a rhinocytogram, children should not normally have red blood cells. If they are present, we can talk about the flu, since red blood cells in this case penetrate through thinned blood vessels into the nasal cavity.
The microflora is normally negative, but if it is present, then the type of infectious agent is determined. Pathogenic microorganisms can occur with bacterial rhinitis or viral rhinitis.
Normal indicators
Deciphering the rhinocytogram in adults is carried out by comparison with indicators accepted as the norm. Results vary depending on the age of the person. The doctor takes into account that deviations from standard indicators do not always indicate the presence of a disease. For a correct diagnosis, an integrated approach is important: taking into account the patient’s complaints, a careful examination by a specialist, the treatment used and its results and other factors. The following are accepted as standard indicators:
| Index | Normal for adults | Norm for children |
| Lymphocytes | No more than 10% | No more than 5% |
| Leukocytes | Single cells | Single cells |
| Microflora | Not identified | Not identified |
| Red blood cells | Single cells | Single cells |
| Eosinophils | No more than 10% | No more than 10% |
| Neutrophils | Between 1 and 3% | Between 1 and 3% |
New classification of allergic rhinitis (ARIA, 2002):
- takes into account symptoms of allergic rhinitis and quality of life indicators;
- involves highlighting:
- intermittent and persistent rhinitis based on the duration of symptoms;
- mild, moderate and severe rhinitis, taking into account the severity of symptoms and the degree of deterioration in quality of life.
The term “episodic (or intermittent)” means that manifestations of allergic rhinitis bother the patient less than 4 days a week or less than 4 weeks. per year. The term “frequent (persistent) presence of symptoms” means that the patient notes the manifestation of symptoms of the disease more than 4 days a week or more than 4 weeks. per year.
Decoding the results
Deviations from the norm of various indicators indicate the presence of a particular disease:
- An increase in the concentration of lymphocytes is observed in chronic, advanced infectious inflammation of the nasal mucosa.
- An increase in the number of eosinophils is characteristic of the allergic nature of the runny nose or eosinophilic rhinitis. In the latter case, nasal polyps may be detected, and the patient complains of lack of relief from taking antihistamines.
- Neutrophils in the rhinocytogram (over 3%) are an indicator of infectious rhinitis caused by bacteria or viruses. An increase is typical in the acute phase of the disease.
- Red blood cells in noticeable quantities indicate an increase in the permeability of the walls of the vessels of the nasal mucosa, which occurs with influenza or diphtheria.
- If microflora is detected (normally absent), a study of the type of microorganisms is carried out. In this case, a viral or bacterial runny nose is diagnosed.
If the decoding of the rhinocytogram in children or adults shows the norm, and the symptoms of a runny nose do not subside, then this is a sign of vasomotor, medicinal or other type of rhinitis. They are caused by long-term use of vasoconstrictor drugs, hormonal imbalances, anatomical features of the nasal passages, vascular dysfunction due to stress, or a specific reaction to cold. In this case, patients are prescribed other studies to clarify the diagnosis.
Rhinocytogram: normal in children and adults, interpretation of nasal smear for eosinophils
The nasal passages and sinuses are one of the main barriers to infections, allergens and other irritants of the respiratory system. A runny nose is a standard safe reaction to infectious inflammation or hypothermia, but its prolonged course and the lack of effectiveness of symptomatic therapy should alert the patient or his parents.
A special study - a rhinocytogram - helps to establish the cause of a prolonged runny nose: the norm in children (in deciphering the analysis result) and adult patients is a small number of immune cells and the absence of pathogenic microorganisms.
Rhinocytogram - what is it?
Rhinocytogram is a method for diagnosing diseases of the nasopharynx based on the cellular composition (cytology) of a nasal smear.
The mucous membrane of the nasal cavities and sinuses consists of various types of cells. Some of them secrete mucous contents, which perform a protective and drainage function. The introduction of a pathogen (fungus, bacteria or virus) provokes tissue inflammation and activation of immune cells - leukocytes.
Viral, allergic and bacterial rhinitis causes swelling of the nasal mucosa and copious secretion of mucus.
At the site of inflammation, blood elements are abundantly present, providing humoral and cellular immunity.
A smear from the affected nasal cavities and examination of a sample of biomaterial can establish the ratio of different types of leukocytes, see the desquamated epithelium and draw a conclusion about the cause of a prolonged runny nose.
In case of a bacterial or complicated viral disease of the nasopharynx, a rhinocytogram allows one to detect the presence of bacteria (mainly cocci).
Many patients are interested in how painful this procedure is and how many days the analysis takes. The rhinocytogram is completely painless: local anesthesia is only necessary for endoscopic sampling of the nasal sinuses. In most laboratories, research and interpretation of the analysis taken takes no more than 1-2 days.
Indications for the procedure
A rhinocytogram is performed to diagnose diseases of the nasal passages. Carrying out a bacteriological analysis and an antibiogram of mucus additionally makes it possible to clarify the composition of the microflora and prescribe the most effective antibacterial drugs.
This analysis is performed for the following indications:
- nasal congestion that persists for more than 7 days;
- copious secretion of mucous contents, which does not decrease with regular rinsing of the nose with saline solutions and the use of local vasoconstrictors;
- frequent sneezing;
- severe itching in the nose;
- diagnosis of bacterial complications of viral rhinitis.
If an infectious inflammation is suspected, the doctor pays attention to the leukoformula of the mucous contents. The presumably allergic nature of rhinitis is an indication for a nasal smear for eosinophils.
During a preventive examination, a rhinocytogram can be prescribed only to patients at risk. These include:
- children who suffer from infectious diseases of the nasopharynx more than 4 times a year;
- people with weakened immunity or immunodeficiency of any etiology;
- patients who have undergone organ transplantation;
- people suffering from diabetes.
Preparing for analysis
To obtain a reliable research result, it is necessary to properly prepare for the collection of biomaterial. Before performing a rhinocytogram, the patient must:
- 5 days before taking the biomaterial, stop therapy with antimicrobial drugs;
- for 1-2 days before the analysis, do not apply antibacterial, hormonal, vasoconstrictor and other ointments, drops and aerosols to the surface of the mucous membrane inside the nasal passages and the skin near the nostrils;
- during the day before the rhinocytogram, do not rinse the nasal passages and sinuses;
- On the day of the test, avoid eating and brushing your teeth.
On the day of the procedure, it is not recommended to drink anything other than water.
In order not to interrupt antibiotic therapy, a rhinocytogram is prescribed mainly in the early stages of the inflammatory process.
Technology
The methodology for conducting this study is simple:
- The patient tilts his head back, and the laboratory technician or nurse uses a special brush or cotton swab to take the required amount of biomaterial.
- The manipulation is repeated with the other nostril.
- The obtained samples of biomaterial from both nasal cavities are placed in a storage container, in which a special environment is created that is favorable for the rapid growth and reproduction of pathogens.
In some cases, analysis of the flora of the nasal passage is insufficient to clarify the diagnosis and exclude complications. To obtain a more reliable result, the doctor may order a sample to be taken from the paranasal sinuses. An endoscope is used to carry out this procedure.
Since deep insertion of the instrument into the nasal cavity causes discomfort, the examination is performed with local anesthesia. The results obtained using the endoscopic method are more accurate and informative than with a standard rhinocytogram.
What indicators are considered normal?
When examining a rhinocytogram, indicators such as the total number and ratio of leukocytes, erythrocytes, epithelium and microorganisms are assessed.
In children and adults with runny nose, the content of various cells in the mucus is normally almost identical. The only obvious difference is the different limits of the permissible value for eosinophils.
In adults
The norm for adult patients is the following values:
- squamous and ciliated epithelium: a small amount in the field of view (f.o.);
- leukocytes: single in p.z.;
- erythrocytes, basophils: absent;
- yeast fungi, pathogenic coccal and rod-shaped microflora: absent (in some laboratories the presence of single bacteria is allowed).
When studying the leukoformula of a smear, the following indicators are important:
- band neutrophils – 1-5%;
- segmented neutrophils – 47-72%;
- eosinophils – 0.5-5%;
- lymphocytes – 0-10%;
- monocytes – 0-10%.
The ratio and concentration of various cells in the mucus of the nasal passages change throughout the day. In the morning and evening the values decrease by 10-20%, and at night they increase by 25-30%.
In children
When conducting an eosinophilic test, it should be taken into account that the normal concentration of leukocytes of this type for children under 13 years of age is 0.5-7%.
Other indicators may also depend on the child’s age and his medical history, so the decoding of the rhinocytogram result must be carried out by an otolaryngologist or allergist.
Decoding the results
The nature of the deviation of study results from normal values for a patient of the same age group may indicate pathology. A rhinocytogram can detect the following diseases:
- Acute viral rhinitis. When infected with adenovirus, influenza and other acute respiratory infections, the value of lymphocytes sharply increases. The value of neutrophils may remain within normal limits. Large numbers of both types of epithelial cells are also detected.
- Acute bacterial rhinitis. The sample reveals a large amount of mucus and up to 85% neutrophils. The bacterial flora must be determined. With severe inflammation, the test shows the presence of squamous epithelium.
- Allergic rhinitis. A runny nose of allergic origin is characterized by eosinophilia - an increase in the value of eosinophils to 10-75%, depending on the severity of the reaction. In case of allergic rhinitis, the analysis reveals basophils and a large number of flat epithelial cells.
- Chronic rhinitis. With chronic runny nose, there is an increase in the number of neutrophils, but to a lesser extent than with acute rhinitis (up to 75%). The analysis results may contain undifferentiated cells (up to 25%).
When infected with certain bacteria and viruses (diphtheria, severe influenza), the smear may reveal single red blood cells sweating through the walls of blood vessels.
It is impossible to independently determine what each indicator means for a given result. When making a diagnosis, the doctor analyzes not only the rhinocytogram data, but also the anamnesis, the nature of the patient’s complaints, the results of an allergy test, bacteriological analysis and PCR.
The absence of deviations in the rhinocytogram during a prolonged runny nose may indicate vasomotor and medicinal rhinitis, endocrine disorders and pathologies in the structure of the nasal passages.
Identifying possible pathogens
When a bacterial flora is detected, a bacteriological study is often prescribed (seeding biomaterial on nutrient media), which determines the type of pathogen and its sensitivity to antimicrobial drugs.
A large number of pathogenic microorganisms are observed mainly in acute rhinitis. In chronic rhinitis, undifferentiated cells are more often found, which are the result of prolonged inflammation, leading to a change in their structure.
Yulia Kalashnik
Source: https://VipLor.ru/nos/rinit/rinotsitogramma-norma-rasshifrovka