Editor
Anna Sandalova
Pulmonologist, doctor of the highest category
Undeveloped immunity and physiological characteristics of the respiratory system of infants contribute to the rapid development of the disease and are fraught with complications.
Pneumonia occurs when a pathogen – a bacteria, virus, fungus or parasitic microorganism – enters the child’s body. It can develop as a complication of prolonged ARVI.
In our article, we focus on symptoms in newborns and infants under 6 months of age.
We urge you not to self-medicate and consult a doctor in a timely manner! Please do not use the described treatment regimens without consulting a doctor - it is dangerous to your health!
What is pneumonia
Pneumonia (pneumonia) is an inflammatory process that develops in the lung tissues. Refers to acute infectious diseases.
To diagnose pneumonia, interviewing and examining the patient is not enough, since the symptoms of pneumonia are often identical to those of other respiratory diseases.
Additionally, adult patients are prescribed the following studies:
- laboratory blood tests - general and biochemical;
- sputum analysis;
- X-ray examination of the chest;
- fibrobronchoscopy;
- computed tomography of the chest;
- bacterial culture.
If the preliminary diagnosis is confirmed, the patient is prescribed immediate treatment.
Temperature
Against the background of other symptoms, temperature is also a sure confirmation of pneumonia. You shouldn’t be scared right away - this is evidence that the child’s body has begun to fight the disease. The following types of temperatures in children during the inflammatory process are divided into:
- Hypothermia – observed in newborns, whose body’s thermoregulation is still poorly functioning.
- Normal - the course of the disease “without fever” can be observed with latent (sluggish) pneumonia.
- Low-grade fever - its range is 37-38°C ; small children may not even notice it, but the battle has already begun.
- Febrile – rises to 39°C ; here you need to be careful - the child’s body cannot cope, it needs active help.
- Area 40°C – critical condition; Immediate medical attention is required.
Upper limits of normal temperature in children when measured in the armpit.
The attitude of medical workers towards the use of antipyretics is now ambiguous. It is believed that it is better not to bring down a child’s temperature below 38°C with medication.
The respiratory system of a small person is not yet sufficiently developed, and there is also pneumonia; the use of antipyretic drugs in these conditions often leads to a lack of oxygen. It is enough to use, for example, special compresses.
Expert opinion
Lyudmila Sokolova
Pediatrician, doctor of the highest category
Ask a Question
If the temperature rises to 38-39°C, accompanied by shortness of breath, there is no need to think about lowering the temperature or not lowering it. Call an ambulance!
The use of medications in childhood is purely individual - a child may well suffer, for example, from a cardiovascular or nervous disease, here temperature control is necessary at any stage .
Pneumonia in infants: symptoms
Neonatal pneumonia in infants often manifests itself as a complication of a disease that precedes pneumonia: ARVI or influenza. Therefore, infants are diagnosed with respiratory dysfunction and nasal congestion. The classic clinical picture develops after pneumonia joins the main infection; the child’s body temperature rises. As a rule, its indicators range from 38 to 39.3o. Pneumonia in infants is accompanied by shortness of breath, frequent and intermittent breathing, and grunting wheezing is detected during listening.
Most often, parents notice the following alarming signs of pneumonia in their infants: difficulty breathing, a cough that was previously superficial becomes deeper with pneumonia, and the intensity and frequency of attacks increases. In some cases, a cough causes nausea and vomiting in a child.
Over time, signs of pneumonia in infants become more diverse:
- the baby burps more often, his stool is unstable;
- depigmentation of the skin appears;
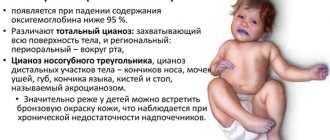
- cyanosis appears in the child’s nose area, which becomes brighter when eating;
- The baby has a loss of appetite.
A sick baby stops gaining weight, coughing attacks disrupt his sleep, and periods of wakefulness become whiny and restless. With pneumonia, there is a rapid development of intoxication and a deterioration in general health.
Age characteristics
Pneumonia in newborns and older infants manifests itself with some differences, depending on age, developmental characteristics and form of the disease.
In infants, pneumonia, in addition to acquired pneumonia, can be congenital and intrauterine. Then the child is born with signs of an already progressive disease.
Distinctive symptoms of pneumonia at birth :
- weakness or absence of basic reflexes;
- signs of asphyxia and hypoxia;
- sharply decreased or increased temperature;
- weak or absent cry;
- blue or gray skin color;
- incomplete opening of the lungs (often in premature infants);
- there may be areas of atelectasis.
A one-month-old baby , like others, becomes infected from the outside. His respiratory system is still very weak and not fully developed, so symptoms of the disease such as cough cannot appear.
Features of manifestations of pneumonia in children 1 month old:
- shortness of up to 70 breaths per minute (normally no more than 40 , shortness of breath in older people - 50 or more breaths );
- there may be no increase in temperature;
- often lack of sweating due to undeveloped thermoregulation;
- 35.5°C is common ;
- tendency to aspiration of vomit or excess mucus during ARVI;
- rapid deterioration of the condition and development of severe symptoms (hypoxia, apnea, toxicosis);
- accompanying intestinal disorders (often with lobar and interstitial forms);
- dehydration.
Artificial ventilation for hypoxia
Children aged 4 months to 6 months have a more advanced immune response and reflexes, therefore the manifestations of pneumonia are more vivid and typical.
Features of symptoms:
- more frequent hyperthermic reaction;
- reducing the likelihood of aspiration;
- more frequent cough as the main symptom.
Online selection of an individual diet for weight loss
How to recognize pneumonia in a baby without fever
Pneumonia in a baby without fever is a rather dangerous phenomenon. The severity of this pathology lies in the absence of pronounced symptoms, as a result of which the disease is detected in the later stages, when the situation has significantly worsened. For a long time after the onset of the disease, parents may not realize that the child is sick; the only reason to see a doctor may be the symptoms of ARVI and the baby’s excessive tearfulness.
Pneumonia in an infant without fever and without the main characteristic symptom – cough, can develop due to weakened immunity, as well as due to the use of antitussive drugs.
Carrying out diagnostics
Immediately after the onset of symptoms of pneumonia in children under one year of age, a comprehensive diagnosis is required, which is carried out in a hospital setting. For this purpose, the baby is examined and then the following methods are prescribed:
- blood analysis;
- sputum examination;
- serological tests;
- X-ray;
- determination of concentrations and gases in arterial blood.
These diagnostic techniques help to quickly make a diagnosis and prescribe appropriate treatment.
Pneumonia in an infant: treatment in a hospital
The treatment regimen is based on antibacterial therapy. Infants under six months of age are prescribed intramuscular and intravenous injections instead of oral forms of medications.
The attending physician, based on the collected medical history and the severity of the disease, specifies the first-choice drugs and makes situational adjustments to the treatment regimen.
In hospitals, oxygen inhalations are used for infants. For the most effective cleansing of the trachea and bronchi, inhalations with special medications or medicinal herbs are prescribed.
If the child has concomitant diseases that complicate the course of pneumonia and are manifested by signs of general intoxication of the body (convulsive syndrome, constant increase in temperature), the baby is given infusion therapy, which provides the body not only with drugs, but also with nutrients and fluid.
If there are specific indicators, therapy is carried out with antipyretic and expectorant drugs. As a rule, these are herbal decoctions that thin and remove phlegm. In the event of the development of a condition that threatens the child’s life, the administration of immunoglobulin is prescribed, which accelerates the rate of the immune response and suppresses the replication of the infectious agent.
Treatment
Principles of treating pneumonia in young children:
- Differential diagnosis to determine the type of disease.
- Antibacterial therapy.
- Inhalations.
- Rational nutrition appropriate to the age and level of development of the child.
- Massage and physical therapy after recovery.
By medication
The basis of drug treatment for pneumonia is antibiotics. Their intake should be carried out strictly on time, so if, for example, the medicine needs to be taken twice a day, then the break between doses should be twelve hours.
The most commonly prescribed antibiotics are penicillins, cephalosporins and macrolides. Their effectiveness is assessed within three days. A good result will be indicated by an improvement in appetite, a decrease in temperature, and the disappearance of shortness of breath.
Taking antibiotics for uncomplicated pneumonia should not exceed seven days (macrolides for five days).
When taking antibiotics, the intestinal microflora is disrupted.
To restore it, probiotics are prescribed. And sorbents are used to cleanse the body of toxins. Antipyretic drugs are needed if the child's temperature rises above thirty-eight degrees. You need to know that during high temperatures, the body produces antibodies against the pathogen, so if a child normally tolerates a temperature of up to thirty-eight degrees, then it is better not to knock it down.
Parents should remember that in case of pneumonia there is no need to give the child restoratives, antihistamines and immunomodulators, as they can cause side effects and do not contribute to the treatment of pneumonia.
If the treatment has shown its effectiveness, then on the sixth to tenth day the child can already walk. And hardening can be carried out after two to three weeks.
Folk remedies
Treatment of pneumonia with the help of folk remedies is best done at the initial stage of the disease and better in combination with other medications.
The child should be given as much to drink as possible. The liquid helps eliminate toxins and reduce temperature. It provides the most effective action of expectorants. It is useful to give your baby water, compote of fresh fruits and berries or dried fruits, herbal tea (mint, chamomile), cranberry or currant juice.
It is very useful to do a honey massage. But we must remember that it is contraindicated for children under six months. Massage helps remove mucus, which is very necessary for pneumonia.
Black radish is very useful and is often used in folk medicine to treat pneumonia because it has expectorant properties. To prepare the syrup, you need to cut a small funnel in the radish where the tail is, fill it with honey and let it brew in a dark place.
Eucalyptus tincture will help restore breathing. It can be used for both inhalation and gargling.
To reduce the temperature, you should give your child barley juice and water sweetened with honey to drink.
Complications of pneumonia
If symptoms of the disease are detected early and adequate treatment is prescribed, the risks of complications are minimized. However, if the body is weakened due to a previous disease or due to delayed treatment, the inflammatory process may drag on or become subacute.
In the chronic form of pneumonia, exacerbations and increased body temperature occur. Even adequate therapy does not always help prevent damage to healthy areas of the lung.
Due to the merging of inflammatory foci into conglomerates, several large zones of infectious damage may appear. In such cases, pneumonia is complicated by pulmonary edema with further development of acute pulmonary failure.
The inflammatory process can also affect the pleura - the membrane of the lung, as a result of which pleurisy develops, chest pain appears and the intensity of spontaneous breathing decreases.
Causes
A child can become infected while passing through the mother's infected birth canal or from the medical personnel who care for him.
The main causative agents of pneumonia are gram-positive cocci (streptococci, staphylococci) and gram-negative bacilli (Escherichia coli, proteus).
The following routes of infection have been identified:
- Transplacental route as part of a generalized infectious process.
- Inhalation of infected amniotic fluid before delivery.
- Aspiration of infected maternal genital secretions during labor.
- Infection with microorganisms after birth.
Neonatal pneumonia can be an independent disease, but most often pneumonia occurs against the background of acute respiratory diseases or as a complication of influenza, measles or whooping cough.
Infants with weak immune systems are at risk of developing pneumonia. Immunity weakens if the child often suffers from acute respiratory infections or has congenital pathologies of the heart or respiratory system, as well as rickets or dystrophy. In addition, pneumonia can result from hypothermia in an infant.
Prevention of pneumonia
The longer children are breastfed, the less susceptible they are to infectious diseases. Therefore, even if there is a shortage of mother’s milk, you should not immediately transfer the baby completely to artificial nutrition. It is advisable to mix breast milk into the mixture. Thanks to the beneficial substances contained in it, the child’s immunity is built.
To strengthen the baby’s body’s defenses, parents should monitor sleep and rest schedules and, in order to avoid the development of anemia and rickets, take more walks with the child in the fresh air.
In order to prevent the baby from hypothermia, parents need to monitor the air temperature in the children's room. We should not forget about moderate hardening: air baths and contrast showers are useful. Persons showing signs of a cold should not come into contact with the baby.
Diagnosis and treatment of respiratory tract diseases are carried out by specialists from the Yusupov Hospital Therapy Clinic - true professionals in their field. As part of the diagnostic examination at the Yusupov Hospital, the full range of studies necessary to identify infectious lesions of the lungs is carried out. Treatment and rehabilitation of patients is carried out using modern medical equipment from the world's leading manufacturers, thereby achieving high efficiency of therapy. If hospitalization is necessary, the Yusupov Hospital has everything you need for a comfortable stay: cozy rooms, nutritious meals and round-the-clock assistance from medical staff. You can make an appointment with a therapist or pulmonologist at the Yusupov Hospital by calling the clinic.
Features in premature babies and after cesarean
Features of pneumonia in prematurity are immaturity of the pulmonary system, atelectasis, collapse of the alveoli and general unpreparedness of the immune system. A common cause of illness after childbirth in premature infants is infection through artificial respiration devices .
When treating pneumonia in premature infants, surfactants (drugs that accelerate lung maturation), immunoglobulins and oxygen therapy are additionally used.
In case of caesarean section, risk factors include the lack of seeding with beneficial microflora from the mother at birth through natural means. Therefore, increased attention when treating such a child is paid to the immunomodulatory component.
More details about pneumonia in premature babies >,>, and after cesarean >,>,.
Recommendations of Dr. Komarovsky for infants
According to pediatrician Komarovsky, special attention should be paid to the prevention of the development of pneumonia (this applies to acquired forms). It is important to notice and not ignore early signs:
- ARVI lasts a week or more,
- fever does not respond to paracetamol,
- shortness of breath even without fever,
- cough and pallor with colds and ARVI.
It is impossible to treat pneumonia without pharmacological agents, and outside the hospital it is dangerous for the child’s life.
Therefore, if early signs are detected, it is necessary to call a doctor and carry out the necessary diagnostics, and if the diagnosis is confirmed, immediately hospitalize the baby in a hospital.
For the purpose of prevention, it is important to ensure ventilation, optimal temperature and humidity in the room where the baby is located.
Important! Under no circumstances should you self-medicate and refuse hospitalization! Pneumonia in newborns is treated exclusively in the clinic’s hospital!
Prevention and rehabilitation in infants
Prevention of congenital pneumonia should include strict monitoring of the health of the expectant mother and timely detection and treatment of detected infections.
To prevent acquired pneumonia in infancy, it is necessary to:
- proper diet and enough fresh air,
- maintaining optimal temperature and humidity in the rooms,
- timely and correct treatment of colds,
- avoiding hypothermia and overheating.
The rehabilitation process includes strict adherence to the recommendations of the attending physician, clinical observation for 12 months after the illness, monitoring of test results and examinations by related specialists (as indicated).