Due to anatomical features and weak immunity, young children often suffer from viral diseases. For some, they go away quickly, and for other small patients, complications of ARVI are possible, such as bronchitis, pneumonia, and so on.
Pediatricians make the diagnosis of bronchitis quite often. The bronchopulmonary system is not yet strong enough to withstand the attack of pathological cells. And the spread of these destructive microorganisms leads to inflammation of the bronchi. Parents are often interested in the question of how to cure bronchitis in a child at home. Below we will look at the causes of this disease and methods of effective treatment.
Concept and characteristics
Chronic bronchitis is a complication of diseases of various etiologies associated with damage to the respiratory system. This pathology can develop against the background of acute respiratory infections, acute respiratory viral infections and other diseases that are not uncommon in pediatrics.
Chronic bronchitis is a progressive inflammatory process of a diffuse type , accompanied by a cough and not associated with lung damage.
The basis for testing a child is if cough symptoms persist for two or three months.
Why does bronchitis occur?
Bronchitis is inflammation in a specific area of the respiratory tract – the bronchi. It can occur when :
- Viral or bacterial infections.
- Allergic reactions.
- Mechanical irritation.
- Chemical or toxic irritation.
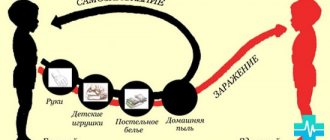
Viruses, allergens, dust and other substances that provoke inflammation enter the bronchi simultaneously with air during breathing. However, the inflammatory process does not always occur . The key point is the state of local and general immunity, which, in most cases, manages to neutralize microorganisms and prevent infection from developing.
A feature of diseases in adolescents is precisely their irresponsible attitude towards their health and the treatment process. Most of them do not accurately follow doctor's orders during an exacerbation.
In addition, when healthy, teenagers often lead lifestyles that
reduce the body's defenses , for example:
- Alcohol consumption.
- Smoking.
- Clothing inappropriate for the weather and hypothermia.
Untreated previous bronchitis or the transition of the disease to a chronic form increases the likelihood of relapses. This is especially common among teenagers from disadvantaged families. In some cases, hereditary factors may play a role.
Causes of the disease
The main reason for the development of chronic bronchitis in children is a combination of a tendency to frequent infectious diseases and a critically low level of the immune system.
Pathogenic microorganisms, entering the mucous membranes of the respiratory organs, spread through the bloodstream through the lymph nodes. The baby begins to get sick often.
The lack of proper treatment provokes the persistence of microbes in the lymphatic system . If this problem is not eliminated for a long time, then there is a risk of developing chronic forms of diseases, including bronchitis.
factors can provoke pathology in a child :
- increased bronchial reactivity;
- constant contact with carriers of infections;
- low level of protective functions of the body;
- lack of timely treatment of infectious diseases;
- anatomical features of the bronchi;
- exposure to an unfavorable climate on the child’s body;
- consequences of passive smoking;
- presence of a tendency to allergic reactions.
Prevention
Teenagers should especially pay attention to the prevention of respiratory diseases. This will help increase local immunity and reduce the number of exacerbations. To do this you need to follow these recommendations :
- Avoid alcohol and smoking until adulthood.
- Eat a healthy diet rich in vitamins.
- Pay attention to the first symptoms of respiratory diseases and treat them promptly. Treatment of prolonged bronchitis will take much longer and more difficult.
- Lead a healthy lifestyle with daily moderate physical activity. Sports train not only the muscles, but also the respiratory system.
During a child’s illness, parents are interested in the following questions :
- Is it possible to walk if you have bronchitis? If the child does not have a temperature, then you can go for a walk. Fresh air speeds up the recovery of the mucous membrane and enriches the body with oxygen.
- Is it possible to smoke if you have bronchitis? Even passive smoking irritates the bronchial mucosa, so not only teenagers, but also their parents should not smoke during illness.
The causes of frequent obstructive bronchitis in children and adolescents lie in a decrease in local immunity and deterioration in the functioning of the organ. Antibiotics will help quickly relieve inflammation, but will not improve the functioning of the respiratory system. Therefore, children over 12 years of age should begin to take care of their health independently, as adults do.
Classification and types
Classification of chronic bronchitis is carried out in several directions. Based on severity, the disease is divided into mild, moderate and severe.
Only a doctor can determine the stage of development of the pathology based on an examination of a small patient.
Chronic bronchitis goes through two stages of progression - the phase of exacerbation and remission (recovery).
Other classification options for chronic bronchitis:
- According to the course, the disease is divided into a latent form , a disease with frequent or rare exacerbations, as well as a continuously relapsing variant.
- Based on the nature of the inflammatory process, the disease is divided into purulent and catarrhal forms.
- According to the functional nature, the pathology can be obstructive ( with complications ) and non-obstructive ( simple form).
Characteristic symptoms
The main signs and symptoms of bronchitis in children:
- At first, the child becomes weak, loses appetite, and headaches appear;
- then parents notice the appearance of a dry cough or with a small amount of sputum. Over time, pain in the throat increases, distinct wheezing, barking cough, and runny nose appear.
On average, body temperature rises to 38 degrees; mild forms are characterized by a mark of 37.5 degrees. After a week, the dry cough turns into a wet one, facilitating the expectoration process; the baby can be completely cured in 14–21 days. Improper treatment can lead to complications and a longer course of the disease.
In case of relapse after recovery, consult a doctor; sometimes the cause of relapse is hidden chronic diseases or weakened immunity. In this case, you will need to take a course of antibiotics, which are prescribed exclusively by a doctor.
Symptoms and signs
The development of chronic bronchitis occurs gradually . At first, coughing attacks occur in the child mainly in the morning. Then their frequency increases, and the symptoms disturb the baby’s sleep, disturbing him at night.
The cough may be dry or accompanied by sputum of varying consistency and color.
With this pathology, it is not possible to eliminate attacks with medications.
In the acute stage, chronic bronchitis develops with additional symptoms . The following symptoms may indicate the development of chronic bronchitis:
- general weakness of the body;
- symptoms of intoxication;
- increased body temperature;
- decreased appetite;
- lingering cough that is difficult to treat;
- a gradual increase in the amount of sputum that is clear or greenish in color;
- dry cough with wheezing and characteristic whistling.
Symptoms of the disease
Obstructive bronchitis in a child can occur suddenly and intensely. If it is strongly expressed, it frightens the parents, and the little patient begins to be fed unnecessary medications. Therefore, it is important to know the symptoms of the disease in order to navigate how to treat obstructive bronchitis.
- The disease manifests itself as a painful, debilitating dry cough that occurs in attacks. Often, at the end of such an attack, the child begins to vomit, as the cough is hysterical.
- This cough is accompanied by severe wheezing. They are whistling in nature and can be clearly heard from a distance.
- When inhaling, the child’s chest rises, and the intercostal spaces are noticeably drawn in.
- With bronchitis of an infectious nature, the temperature often rises. It can rise to 39 degrees.
- Sometimes accompanying symptoms are a runny nose and throat hyperemia. The infection spreads in the throat and nasopharynx. Allergic rhinitis may develop and cannot be treated with conventional antiviral drugs.
- An important and dangerous symptom of this type of disease is shortness of breath; it is difficult for the child to breathe.
- Nonspecific signs of bronchitis are weakness, increased fatigue, lethargy - these are signs of general intoxication.
Why is it dangerous?
Chronic bronchitis is one of the deadly diseases. As the pathology progresses, clogging of the bronchi with mucus .
This condition can provoke irreversible inflammatory processes in the respiratory system.
If chronic bronchitis is not treated for a long time, then the risk of death of the baby reaches a critical level.
The following conditions may cause complications
- pulmonary emphysema;
- formation of polyps;
- bronchial obstruction;
- death.
Chronic bronchitis in a child, symptoms
What signs characterize the course of the disease:
- General intoxication of the body. The younger the child, the more pronounced it is. Characterized by loss of appetite, increased sweating, fever and lethargy.
- Cough, which is the body's attempts to get rid of accumulated phlegm. There are both dry and wet coughs. Dry is the most painful for the baby, causing pain, soreness, and irritates the mucous membrane of the throat. When a child often experiences exacerbations of the disease, the cough can be quite long.
- During coughing, sputum may be released, both transparent, which is serous, and with a green tint, purulent in nature. With the duration of the process, the amount of sputum produced gradually increases. Parents are faced with the problem of how to explain to their little toddler the need to cough and also spit out mucus.
- If the baby has obstructive chronic bronchitis, then it may be accompanied by specific wheezing sounds. An experienced wheezing specialist will be able to determine in which part of the bronchi the maximum damage is present.
- Asthma attacks and shortness of breath can also characterize the obstructive form of chronic pathology. More often it occurs in the first half of the day, and attacks of suffocation occur when exhaling.
- By listening to the baby's chest with a stethoscope, the doctor will be able to determine the type and stage of chronic bronchitis. Possible weakening or harshness of breathing.
- The doctor, after conducting a series of studies, will be able to determine the presence of chronic bronchitis:
- a general blood test is characterized by reduced hemoglobin and a high level of ESR;
- On x-ray, expansion is noticeable in the root section of the bronchial tree.
- The exacerbation of chronic bronchitis is attributed to the change of seasons. It lasts up to four weeks.
Diagnostics
The basis for suspecting chronic bronchitis is the child’s tendency to protracted respiratory diseases (if the diseases occur 4-5 times a year and are difficult to treat).
This diagnosis is not given to children until the age of three.
This nuance is due to the process of formation of the respiratory system . After three years, the risk of developing chronic bronchitis increases. The diagnosis is confirmed by conducting a comprehensive examination of the small patient.
The following methods are used for diagnosis:
- cytological, biochemical and macroscopic examination of sputum;
- bronchoscopy;
- PCR analysis;
- laboratory blood test;
- X-rays of light;
- bronchogram.
Duration of acute form
How long the treatment of acute bronchitis in a child will last depends on the correct treatment of the disease and the creation of optimal conditions for recovery. Children are not recommended to visit public places, school, or kindergarten during this period. Violation of the pulmonologist's instructions can lead to aggravation of the condition and poor health.
The acute form is an illness lasting more than 12 days. In case of severe inflammatory processes, bed rest should be observed. Antibiotic therapy is prescribed for up to 10 days. The age of the child is the main determining factor in the duration of the pathological condition.
In young patients under one year old, bronchitis may disappear only after three weeks. Children from 2 to 5 years old, according to average data, get sick for up to 14 days. The age of a child of 5-9 years allows the formation of the body’s protective functions, which affects the recovery time, reducing it to 10 days.
If the cough persists for more than two weeks, there is a risk of developing complications, or it is a sign of an allergic reaction of the body to the irritant. It is important to promptly determine the cause of the symptoms. A sharp, paroxysmal cough that persists for more than three weeks may indicate whooping cough.
Treatment
How to treat a baby? Treatment of chronic bronchitis is carried out using a complex method. The child may be prescribed not only drugs of certain categories, but also additional procedures.
Halotherapy, therapeutic massage, physiotherapy, and breathing exercises are highly effective. The techniques increase the body’s protective functions and have a beneficial effect on the baby’s respiratory system.
Medicinal and non-medicinal
A list of necessary medications for the treatment of chronic bronchitis should be compiled by a doctor.
The disease requires long-term therapy, which will combine specific drugs.
If they are not effective, they will be replaced with potent drugs .
In some cases, children are placed in a hospital. The treatment regimen for bronchitis in this case is selected individually.
Examples of drugs:
- drugs from the adrenergic stimulant group (Salbutamol, Ephedrine);
- drugs for thinning sputum (Bronchicum, Mucaltin, Stoptussin);
- proteolytic enzymes (Chymotrypsin, Trypsin);
- mucoregulators (Bromhexine);
- antipyretics (Ibuprofen, Paracetamol);
- preparations for clearing phlegm from the bronchi (Doctor IOM, ACC, Ambrobene);
- bronchospasmolytic drugs (Eufillin).
Additional non-drug procedures are prescribed to children not only for the treatment of chronic bronchitis, but also to prevent complications and relapses of the disease.
The procedures help normalize the condition of the respiratory system, strengthen the general immune system and speed up the recovery process of the little patient.
Some methods require a mandatory preliminary examination by a specialist and are carried out according to the appropriate direction of the doctor.
Non-drug methods for treating chronic bronchitis:
- Bronchodilator therapy (inhalation of drugs from the group of bronchodilators, hyperbaric therapy, etc.).
- Physiotherapeutic procedures (magnetic therapy, electrophoresis, UHF therapy, etc.).
- Antihypoxic therapy (oxygen therapy, etc.).
- Immunomodulatory procedures (for example, heliotherapy).
- Myostimulating approach (electrical stimulation of the diaphragm using the percutaneous method).
- Mucolytic therapy (vibration, therapeutic, vacuum massages, aromatherapy, etc.).
Folk remedies
How to cure chronic bronchitis in a child using folk remedies? Alternative medicine recipes in the treatment of chronic bronchitis can be used as an auxiliary means of therapy.
Some methods of using natural ingredients help speed up the child’s healing process and improve the general condition of the body. They are not able to eliminate the main cause of the disease or completely eliminate complications and relapses .
When selecting recipes, it is important to take into account a possible allergic reaction to products (honey, for example, can be used only after the child is four years old).
Examples of traditional medicine recipes:
- Lard with milk (melt the lard in a water bath, dilute a teaspoon of the preparation in a glass of milk, take the product in small sips a maximum of twice a day, the course of treatment of chronic bronchitis with this method is one month).
- Herbal decoction (combine linden blossom, peppermint and sage in equal proportions, pour 300 ml of boiling water over a tablespoon of the preparation, leave for twenty minutes, take several times a day in small portions, you can add a small amount of honey).
- Linden tea with honey (pour boiling water over a teaspoon of linden flowers and leave for twenty minutes, add a teaspoon of honey to the resulting tea, take several times a day, the product can be used to prevent complications of infectious respiratory diseases).
How to choose a medicine for bronchitis in a child
When prescribing medications, the doctor relies on the cause of the disease:
- Viral infection. It often occurs in an acute form without complications, the patient recovers within 10 days. Bronchitis in this situation can be treated with immunostimulants and drugs that remove mucus from the respiratory tract. The patient is advised to rest in bed and drink plenty of fluids.
- Bacterial. For mild cases, therapy is symptomatic. If there are pronounced signs of intoxication (fever, chills, malaise), wheezing in the chest, thick mucus is released when coughing, antibiotics are used.
- Allergic bronchitis. Antihistamines are needed to reduce swelling and inflammation.
For any bronchitis, symptomatic therapy is necessary:
- Anti-inflammatory (hormonal, non-steroidal). They relieve swelling of the mucous membrane, but have many side effects. It is better to treat bronchitis in a teenager without glucocorticoids, because they negatively affect growth and development.
- Antipyretic. They are needed at temperatures above 38.5º, which do not fall for more than a day.
- Mucolytics, expectorants. A mandatory component of treatment to get rid of sputum accumulation.
Clinical guidelines
Chronic bronchitis is a complex and dangerous disease. The prognosis for the child directly depends on the correctly selected treatment regimen. If the diagnosis is confirmed and complications are identified, hospitalization is necessary.
Therapy at home must be carried out in strict accordance with the doctor’s instructions. If there is no effect or the baby’s condition worsens, then a repeat examination is necessary.
Clinical guidelines:
- treatment begins with the use of mucolytics;
- in addition, the doctor prescribes procedures performed in medical institutions;
- Measures must be taken to strengthen the body’s immune system;
- further treatment regimen depends on the individual clinical picture of the child’s health condition;
- After therapy, a follow-up examination is required;
- Treatment is not limited to a single course; parents need to regularly take measures to prevent relapse of the disease.
Chronic bronchitis in children - clinical protocol.
Antibiotics for children with bronchitis
These drugs should be used to treat a child if the disease is of bacterial origin, but the doctor selects them based on test results. In pediatrics, penicillins or macrolides are often used (better tolerated). In severe cases, cephalosporins and sulfonamides are needed. Medicines are given to children in liquid form, and to children over 6 years old - in tablet form. It is important to complete the course completely so that the remaining bacteria do not develop resistance to the drug and complications arise.
Zinnat
It is recommended to treat severe, protracted bronchitis with an antibiotic from the cephalosporin group. Cefuroxime (the active substance) has a wide spectrum of action and helps where penicillins do not work. Take it after meals, the course is 5-10 days. Children are prescribed Zinnat in tablets and powder for solution from the age of 3 years. It can cause headaches, gastrointestinal disorders, and skin rashes. The medicine is prohibited if you are intolerant to beta-lactam antibiotics. Price – 210 rub./10 pcs.
Sumamed
A drug made from macrolides (azithromycin) is popular in pediatrics and is approved from 3 years of age. Sumamed has a wide spectrum of action, is indicated for allergies to penicillins, but is prohibited for severe kidney and liver disorders. The drug is effective for infections caused by atypical pathogens; for bronchitis, it is taken for only 3 days. Long-term treatment may cause diarrhea. The tablet can be dissolved in water if the child has difficulty swallowing it. Price – 380 rub./3 pcs. (500 mg).
Bactrim
Children are treated with a combined antibiotic of sulfonamides in the form of a suspension from 3 weeks, the dose is adjusted according to weight. The drug is used for severe acute infections, with pneumonia and other complications, when other drugs do not work. The course of treatment is 5-14 days. Bactrim has many contraindications: liver and kidney pathologies, anemia, leukopenia, asthma (drink with caution). Adverse reactions from all body systems are possible. Price – 1890 rub./100 ml.
Doctor Komarovsky's opinion
Dr. Komarovsky strongly recommends that parents not self-medicate if they suspect chronic bronchitis in children.
If the child’s cough is prolonged, difficult to treat, and relapses of the disease become regular, then the child must be examined. The inflammatory process in the bronchi can only be determined by a doctor using special diagnostic procedures.
Additionally, Dr. Komarovsky advises :
- Provide the child with plenty of fluids (liquid will help speed up the process of sputum discharge);
- a small patient should not be in a room with high air humidity (regular ventilation and wet cleaning are mandatory conditions);
- You should not start treating a viral infection with antibiotics (the best option is antiviral drugs);
- The symptoms of colds in children cannot be ignored (any disease must be fully and promptly treated).
Acute bronchitis
Authors : Ryltsov A. Yu.
Acute bronchitis (AB) is an acute respiratory infection of the respiratory tract, the leading symptom of which is cough. [1] The main causes of acute bronchitis are viruses: respiratory syncytial virus (RS virus), adenovirus, coronavirus, influenza and parainfluenza viruses. Acute bronchitis is a purely clinical diagnosis, which is, in fact, a type of acute respiratory viral infection. Very rare causes of acute bronchitis are bacteria, mycoplasmas, chlamydia, and fungi. Since acute bronchitis is a viral infection in most cases, symptomatic therapy is usually sufficient to treat it.
Pharmacotherapy of acute bronchitis. Antibiotics should not be routinely prescribed for acute bronchitis. Meta-analyses of studies suggest that antibiotics may slightly reduce the duration of cough in some patients. However, it is impossible to identify a subgroup of patients who benefit from antibiotics, and the beneficial effect itself appears to be very modest. Thus, in a meta-analysis of 8 studies, it was shown that the use of erythromycin, doxycycline and co-trimoxazole reduces the duration of cough by 0.5 days, the duration of purulent sputum production by 0.4 days, and the duration of disability by 0.3 days. [2] This “success” turned out to be statistically significant, but does not justify the prescription of antibiotics for OB, taking into account the risk of side effects. A Cochrane meta-analysis of 15 randomized clinical trials [3] showed a statistically significant reduction in cough (less than 1 day) when treating acute bronchitis with antibiotics. This effect deprives clinical value of the risk of side effects, increasing bacterial resistance to antibiotics and the financial factor of treatment costs. However, the vicious practice of treating OB with antibiotics has not been eliminated, both in the post-Soviet space and in foreign countries. Most studies show that antibiotics are inappropriately prescribed in 65% to 80% of cases of acute bronchitis. [4] A doctor can individually prescribe an antibiotic for OB if he finds criteria for a bacterial infection, for example, neutrophilic leukocytosis in a general blood test or a confirmed connection between OB and the causative agent of whooping cough. However, in the latter case, the diagnosis will be whooping cough, not OB. Specific antiviral treatment is appropriate only for acute bronchitis caused by the influenza virus. Two antiviral drugs for influenza - oseltamivir or zanamivir - are prescribed mainly in the first 48 hours from the onset of the disease, in severe and complicated influenza, as well as in groups at risk for complications.
Use of beta-2 agonists. A Cochrane meta-analysis [5] showed a small benefit of beta-2-agonists in reducing cough in acute bronchitis. In the presence of bronchospasm syndrome, the administration of short-acting beta-2 agonists (salbutamol) is effective and safe. Bronchospasm in acute bronchitis requires the exclusion of bronchial asthma and COPD. Criteria for bronchospasm are shortness of breath, prolongation of expiration during auscultation of the lungs and dry rales. Spirography objectifies bronchospasm. Particularly noteworthy is the inappropriate use of salbutamol preparations orally. A single dose of salbutamrol in such preparations is usually 2-4 mg, while a single dose of salbutamol in an inhaler is 0.1 mg. Clenbuterol, a beta-2 agonist for systemic use, is inferior to salbutamol in terms of side effects and has no evidence base for use in OB.
The inhaled anticholinergic drug ipratropium bromide has a bronchodilator effect and is effective for prolonged cough associated with acute respiratory syndrome. [6] Of particular note is the problem of unaccountable fear of inhalers among the post-Soviet population. Many patients say this: “I'm afraid of inhalers! They say that once you spray, you will spray for the rest of your life!” This fear is rooted in the deep Soviet past, when bronchial asthma was diagnosed only in severe form and treated with inhalers, so much so that it often led to asthmatic status and death from asthma. Whereas the most common mild asthma was not diagnosed at all and was called chronic bronchitis with an asthmatic component. So an association has developed in the popular consciousness between the use of inhalers and severe asthmatic suffering.
Remedies used for dry cough. The variable and episodic nature of OB prevents the establishment of a clear evidence base for antitussives in high-quality clinical trials. However, there is evidence that some cough suppressants are effective. Dextromethorphan is an opiate that has an antitussive effect and, in a therapeutic dose, is free from the side effects of opiates. [7] The generally recommended dose of dextromethorphan appears to be subtherapeutic. A pronounced antitussive effect is shown with a single dose of 60 mg. [8] However, it is unacceptable to exceed the dose recommended in the instructions for the dextromethorphan-containing drug. Due to the risk of side effects and intoxication with other components of the drug, if we are talking about combined drugs. Dextromethorphan is incompatible with MAO inhibitors. Cytochrome P450 inhibitors (quinidine, amiodarone, fluoxetine). Combination with tricyclic antidepressants and SSRIs can cause serotina syndrome. Inhaled menthol [9] Cough suppression with menthol occurs quickly but does not last long. Menthol-containing cough drops are a safe, effective and inexpensive alternative to other cough suppressants. Representatives of the first generation of antihistamines (diphenhydramine, clemastine, chloropyramine, etc.) suppress cough very effectively, but at the same time cause drowsiness. Therefore, they are suitable for solving the problem of night cough. Codeine is no better than dextromethorphan in relieving dry coughs, but has a wider range of side effects.
Medicines used for productive cough. [11] The expectorant guaifenesin does not have mucolytic activity, but can reduce the surface tension of sputum in the bronchi and, due to its cholinergic effect, stimulate sputum secretion. The expected effect of guaifenesin is to facilitate the passage of thick and thin sputum. The mucoregulator carbocysteine has evidence of clinical effectiveness in COPD. The mucolytic acetylcysteine reduces the viscosity of sputum; in addition, it is an antioxidant and antidote for paracetamol intoxication. The related drug erdocyteine has a similar symptomatic effect on cough. The mucokinetic agent ambroxol stimulates the secretion of sputum and surfactant. Studies on its clinical effectiveness provide conflicting results. But a subjective effect is quite possible. There is evidence that ambroxol promotes the accumulation of the antibiotic amoxicillin in the lungs. [12] Separately, it should be noted herbal medicines that have some evidence base for acute bronchitis: pelargonium (Pelargonium sidoides), thyme, ivy. [13,14]
Features of the treatment of acute bronchitis in children. The general principles of treatment of OB in children and adults are similar. It should be especially noted that it is inadmissible to prescribe expectorants to children under 2 years of age and the inappropriateness of prescribing to children under 5 years of age. The RS virus that causes OB in adults often causes acute bronchiolitis in infants with severe bronchial obstruction syndrome. There is evidence of the effectiveness of ribavirin against RS viral infection in children. [15] However, a meta-analysis of studies does not allow us to conclude that the effect of ribavirin in MS infection is convincingly proven. [16] Interferon preparations, when applied topically, reduced the replication of rhinoviruses and slightly reduced the symptoms of rhinovirus infection in one experiment. This is not a reason to treat OB with interferon, even though rhinovirus can cause OB. [17] A meta-analysis of studies on the use of acetylcysteine and carbocysteine in children showed a controversial and extremely limited positive effect. [18] A systematic analysis [19] of the use of over-the-counter drugs used for acute cough in children and adults did not exclude or confirm the clinical effectiveness of these drugs. Data from different studies are inconsistent, and the quality of most studies is low. And this is not surprising. Most cough medications are purely commercial products that sell well anyway. It is not profitable for manufacturers to invest in research that is likely to fail. It is more profitable to invest money in advertising aimed at the end consumer - the patient.
Prevention of OB. Influenza vaccination, relevant for groups at risk of complications (people over 65 years of age, patients suffering from diabetes, chronic diseases of the respiratory and cardiovascular systems). General measures to prevent ARVI (separation from the source of infection, frequent hand washing, healthy lifestyle).
Summary. OB is a self-limiting disease for which symptomatic therapy under medical supervision is usually sufficient. An obsessive dry cough can be relieved by an antitussive and a wet expectorant. However, in most cases, drinking plenty of fluids and keeping the air humid will be very effective in relieving your cough. In the presence of bronchospasm, salbutamol is appropriate. A diagnosis of OB is not a reason to prescribe antibiotics and turn the patient’s stomach into a pharmaceutical warehouse. Nobody needs multi-component drugs and multi-stage treatment regimens. One or two medications are enough to relieve the most severe symptoms. The main thing, with the participation of a doctor, is to exclude complications and diseases other than banal viral bronchitis.
Bibliography.
- Gonzales, R, Sande, M (2000) Uncomplicated acute bronchitis. Ann Intern Med133,981-991
- Bent S, Saint S, Vittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. Am J Med 1999;107:62-7.
- Smith SM, Fahey T, Smucny J, Becker LA Antibiotics for acute bronchitis (Review) Cochrane review, prepared and maintained by The Cochrane Collaboration and published in The Cochrane Library 2012, Issue 4
- Braman, S.S. "Chronic Cough Due to Acute Bronchitis: ACCP Evidence-based Clinical Practice Guidelines." Chest 129 1 (2006):
- Becker LA, Hom J, Villasis-Keever M, van der Wouden JC. Beta2-agonists for acute bronchitis. Cochrane Database Syst Rev. 2011 Jul 6;(7):CD001726.
- Holmes PW, Barter CE, Pierce RJ. Chronic persistent cough: use of ipratropium bromide in undiagnosed cases following upper respiratory tract infection. Respir Med 1992;86:425–9
- Parvez L, Vaidya M, Sakhardande A, et al. Evaluation of antitussive agents in man. Pulm Pharmacol 1996; 9:299–308
- Manap RA, Wright CE, Gregory A, et al. The antitussive effect of dextromethorphan in relation to CYP2D6 activity. Br J Clin Pharmacol 1999; 48:382–7
- Morice AH, Marshall AE, Higgins KS, et al. Effect of inhaled menthol on citric acid induced cough in normal subjects. Thorax 1994; 49:1024–6
- Robinson RE, Cummings WB, Deffenbaugh ER. Effectiveness of guaifenesin as an expectorant: a cooperative double-blind study. Current Therapeutic Research1977;22 (2):284–96.
- R. Balsamo*, L. Lanata* and CG Egan Mucoactive drugs REVIEW Eur Respir Rev 2010; 19: 116, 127–133
- Gené R, Poderoso JJ, Corazza C, Lasala MB, Wiemeyer JC, Fernández M, Guerreiro RB. Influence of ambroxol on amoxicillin levels in bronchoalveolar lavage fluid. Arzneimittelforschung. 1987 Aug;37(8):967-8.
- Kemmerich B, Eberhardt R, Stammer H. Efficacy and tolerability of a fluid extract combination of thyme herb and ivy leaves and matched placebo in adults suffering from acute bronchitis with productive cough. A prospective, double-blind, placebo-controlled clinical trial. Arzneimittel-Forschung 2006;56:652–660.
- Timmer A, Günther J, Rücker G, Motschall E, Antes G, Kern WV. Pelargonium sidoides extract for acute respiratory tract infections. Cochrane Database Syst Rev. 2008 Jul 16;(3):CD006323.
- SMITH DW, FRANKEL LR, MATHERS LH et al. : A controlled trial of aerosolized ribavirin in infants receiving mechanical ventilation for severe respiratory syncytial virus infection. N.Engl. J. Med. 325 (1):24-29.
- VENTRE K, RANDOLPH A: Ribavirin for respiratory syncytial virus infection of the lower respiratory tract in infants and young children. Cochrane Database Syst. Rev. (2004) 4 :CD000181.
- ROTBART HA,: Treatment of picornavirus infections. Antiviral Res. (2002) 53(2):83-98.
- Chalumeau M, Duijvestijn YC. Acetylcysteine and carbocysteine for acute upper and lower respiratory tract infections in pediatric patients without chronic broncho-pulmonary disease. Cochrane Database Syst Rev. 2013 May 31;5:CD003124.
- Over-the-counter (OTC) medications for acute cough in children and adults in ambulatory settings. Cochrane Database Syst Rev. 2012 Aug 15;8:CD001831. doi: 10.1002/14651858.CD001831.pub4.
Consultations of Alexander Ryltsov in ClubCom
published 02/17/2014 10:41 updated 12/12/2018 — Respiratory diseases, Pulmonology
Folk remedies in the fight against bronchial diseases
Folk remedies have long helped fight various diseases. Their indisputable advantages include naturalness and a minimum number of possible side effects. For bronchitis in children, traditional medicine helps reduce inflammation of the bronchi and make the cough less intense. Moreover, such drugs can be used as an auxiliary rather than primary therapy.
Thus, children can benefit from cabbage and honey cakes, compresses with sunflower oil and honey to warm the chest, bear or badger fat, as well as baked onions as rubs. But such procedures can only be carried out if the child has a cough against the background of normal body temperature. A child can soak their feet in an infusion of St. John's wort, chamomile sage, mint or mustard solution. In this case, the water temperature should be no more than 40 degrees.
It should be remembered that badger fat, milk and many herbal remedies help not only cure the current disease, but also strengthen the immune system, and, therefore, reduce the risk of diseases in the future. If there is no allergy, a 2-year-old child can be given herbal decoctions (linden, mint, chamomile, coltsfoot, calendula) to drink. Pharmacy breast milk and warm milk with honey and soda are also effective.
If bronchitis is accompanied by a very severe cough, then the child should be given carrot or cabbage juice, garlic juice added to water or milk in the amount of 1 drop, as well as onion or black radish juice with sugar. It is recommended to put aloe juice in your nose. For the obstructive form of the disease, lingonberry juice with sugar or honey, warming compresses with potatoes, salt or buckwheat porridge are used.