The appearance of purulent accumulations in the corners of the eyes in children occurs both after sleep and throughout the day. As a rule, purulent discharge in the morning, which is eliminated after the washing procedure, is not a sign of disease - pus in a child’s eyes appears as a natural reaction of the body to specks and dust that got under the eyelid during the day. It is during the night that the body removes such foreign particles. If the eyes do not fester during the day, there is no need to worry.
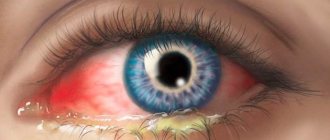
Another problem is if purulent discharge from the eyes is not only not eliminated with the help of daily hygiene, but it intensifies during the day, in addition to this, other unpleasant signs usually appear - lacrimation, photophobia, redness of the eyes, swelling. All these are characteristics of eye pathology, which will be determined by an ophthalmologist. The most common cause of eye infections is conjunctivitis.
Main reasons
The first question that parents have is why pus appeared in front of the baby’s eyes. There are factors that provoke the development of the disease.
Causes of suppuration:
- manifestation of an allergic reaction;
- the lacrimal glands have not fully developed;
- chlamydia in the child’s body;
- possible reaction to medications;
- dacryocystitis;
- conjunctivitis.
When a child is born in the maternity hospital, albucid is instilled into his eyes. Sometimes a reaction to this drug leads to suppuration. It is enough to wash it once, and everything goes away.
Perhaps the cause of suppuration is an allergy - for example, to milk or medications. Tears begin to be released in large quantities, and because of this, the eyes of a month-old baby turn red and sour.
Conjunctivitis is an infectious lesion of the mucous membrane. It is necessary to treat the disease only after consultation with a doctor. Drugs are selected based on the individual characteristics of the baby’s body.
Another common disease is dacryocystitis. The tubules become clogged, which leads to rapid inflammation of the lacrimal sac, and it turns sour. Most often, dacryocystitis occurs because the baby’s protective film is torn at birth. This leads to the rapid proliferation of microbes, and as a result, parents notice purulent formations on the mucous membrane. In this situation, an ophthalmologist can help based on the results of the examination and tests.
When a child cries frequently, tears begin to accumulate. A large number of them leads to the fact that the eye turns sour and pus appears.
To eliminate the disease, it is first necessary to identify the cause of the baby’s anxious state.
Classification of types of eye discharge
Discharge from the eyes of a child can be of a different nature and differ in the following characteristics:
- Clear, whitish or white discharge, similar to tears, forms in the eyes during allergic reactions. They may be accompanied by redness and swelling of the eye, severe itching and irritation. If they are not removed, they will dry out on the baby's eyelids and cheeks in thin, flaky films. Treatment is required immediately, so seeing a doctor is vital. He will identify the allergen and prescribe the necessary treatment. This mainly involves protecting the baby from the source of allergens (food, feather pillows, dust, animal hair, etc.) and taking special antihistamines.
- Mucopurulent discharge accompanies conjunctivitis of bacterial or viral origin. This is a common occurrence in young children. Treatment should be specialized, after analysis and identification of the cause of the disease.
- Greenish and yellow discharge in newborns or young children indicates the development of purulent conjunctivitis or dacryocystitis (inflammation or blockage of the tear duct and sac). The disease can have a protracted chronic form, therefore it requires quick and proper treatment, sometimes it is necessary to resort to minor surgical intervention.
- Crusts and scales in the baby's eyes should cause particular concern to parents, as they may indicate the presence of blepharitis. This inflammation of the eyelids can be provoked by various reasons and has a chronic course.
Blepharitis is difficult to treat in an advanced state, so you should not hope that you can cope with home remedies.
Any manifestation of eye health can threaten the quality of the child’s vision in the future, so a visit to the doctor cannot be postponed until the future. The sooner proper treatment is started, the faster the recovery process will take place, the lower the risk of complications and the disease becoming chronic.
Traditional treatment
You cannot start treatment on your own, because if you choose the wrong medications, you will only harm your baby. All medications and procedures for the child must be prescribed by an ophthalmologist and pediatrician. Doctors identify the root cause why the pus appeared, and only after that they select the optimal medications. However, there are several recommendations that parents can follow regardless of whether the milk gave suppuration or other factors contributed to this. The recommendations presented are safe and suitable for children of any age.
Hygiene procedures
If the eye is covered with pus, you need to try to eliminate it as quickly as possible. It is recommended to pay attention to hygiene procedures:
- washing the mucous membrane of the child;
- removing crusts from eyelashes and eyelids with a cotton swab;
- rubbing with herbal solutions (chamomile, calendula).
Before using medicinal herbs, you need to make sure that the baby is not allergic to them.
If you have completed all of the above procedures, you can proceed to the next stage - massage. It must be done with clean hands and light movements. The main area of stimulation is near the nose and the inner corners of the eyes. This promotes more efficient functioning of the sebaceous glands. Purulent formations are eliminated through the tubules over time. How do you know if you started doing massage correctly? If at the end of the procedure a yellow substance is released, it means you are doing everything well. Further treatment depends on the individual characteristics of the child’s illness.
Allergy treatment
Allergies in a baby usually manifest themselves to mother's milk or pharmaceutical infant formula. If the child is bottle-fed, you should try a different formula, changing the manufacturer.
If the newborn does not accept breast milk and the mucous membrane festers, there may be a problem in the mother’s diet: the diet should be reconsidered, the allergen should be identified and eliminated.
Treatment for conjunctivitis
If a child has been diagnosed with conjunctivitis, a different approach to solving the problem is necessary. The first step is to eliminate the infection, and then the doctor identifies the factors that caused the development of the disease.
When there is an infection, the eye turns sour, so you need to remove the pus quickly, otherwise the disease will progress quickly. To do this, the doctor prescribes a solution of furatsilin. If the infection is serious, then the baby will have to be treated with antibiotics.
Medical procedures
If there is slight suppuration, the doctor prescribes the following medications that can be used to wash the eye:
- chloramphenicol;
- antibacterial ointments;
- furatsilin solution.
If after treatment the tear duct does not uncork, doctors are forced to do probing.
This procedure is done under local anesthesia, so the newborn does not feel pain. Using a probe, the doctor carefully removes the film that is blocking the tear duct.
After the procedure, parents need to follow all hygiene rules, because infections very quickly affect the eye and sour back.
Nursing mothers need to reconsider their diet. Everything that is consumed ends up in the milk, and this can trigger an allergic reaction.
Traditional methods of treatment
If desired, parents can resort to traditional methods of treatment to rid the child’s eye of accumulated purulent formation. Let's look at the most popular methods.
- The easiest option is to treat the eye with chamomile decoction. For this, regular tea is used, which is absolutely safe. Take a cotton swab, soak it in the resulting liquid, then gently wipe the baby’s mucous membrane. If the child is sleeping, you can put an already used chamomile tea bag on the eyelids. This method relieves inflammation and removes purulent formations.
- Breast milk has long been considered the best cure for many diseases. Surprisingly, it also helps with conjunctivitis. Milk should be used in the same way as tea. It is sterile and cannot harm the baby.
If parents notice that the baby’s eyes are very festering, under no circumstances should they hesitate. It is necessary to do several of the above procedures at home as quickly as possible (for example, use breast milk) and make an appointment with your doctor. After receiving the test results, the factor causing the eyes to fester is identified, and complex treatment can begin.
→ Very useful! about why babies' eyes fester! what to do, what is this, etc.!!!
A newborn's eyes are festering. Eye diseases are quite common in infants. We'll talk about dacryocystitis. Under this strange name lies a disease that is quite common in newborns, but fortunately it is quite easily curable if measures are taken in time. A symptom of this disease is pustular discharge from the eye. As a rule, these discharges are present only in one eye and are caused by underdevelopment of the lacrimal canal, in contrast to conjunctivitis, which is caused by viruses and bacteria.
To understand the essence of the disease, consider the structure of the eye and the function of tears. As you know, a tear, washing the eyeball, protects it from drying out, and also protects it from various viruses and bacteria. Tears are produced by the lacrimal glands, wash the eyeball and then accumulate in the inner corner of the eye. There are two lacrimal openings, one on the lower and one on the upper eyelid. They are easy to see with the naked eye if you move the edge of the eyelid. Through these points, tears enter the nasolacrimal duct and from there into the nasal cavity, which is why when we cry, it seems that we have a runny nose. We can pass through a normally functioning tear duct, but if for some reason it is closed, then the tear accumulates and overflows over the edge of the eyelid. First, there is profuse lacrimation, the bactericidal function of the tear fails, the eye becomes inflamed, turns red and then begins to fester. A newborn's eyes fester. The most common cause of obstruction of the lacrimal canal in infants under 2 months is the formation of a so-called “gelatinous plug” in the canal. Other causes of obstruction are much less common. This disease is quite common and occurs in approximately 5% of newborns. Inflammation of the eye caused by impaired tear flow is called neonatal dacryocystitis. The gelatinous film is formed from mucus and embryonic cells of the child. After birth, along with the first respiratory movements, it is pushed out, and the lacrimal canal breaks through on its own. If for some reason, and there may be several of them, the channel does not break through on its own, then a pathology is formed that leads to inflammation. Sometimes lacrimation and inflammation begin almost from the first days after birth, sometimes by the end of the first month. Usually, first the eye becomes inflamed, becomes red, after about 8-10 days purulent discharge appears; if you press the area of the lacrimal sac with your finger, then pus will be released from the lacrimal opening. Most often, the gelatinous plug separates on its own 2 weeks after birth, but it happens that this does not happen. In any case, before making a diagnosis and starting treatment, you need to show the child to a specialist. Most often, the doctor will first prescribe you conservative treatment, and only if this does not help, will you have to perform a rinse in the hospital. Conservative treatment consists of washing the eye with a solution of furatsilin, chamomile or tea leaves, performing a special massage and instilling antimicrobial drops (albucid, collargol 2%, Vitobact) or an antibiotic (levomycytin, penicillin). Do not rinse or instill the eye with breast milk. After all, inflammation occurs as a result of the proliferation of microbes, and milk is a breeding ground for them; it turns out that this can only increase their number, and not cure the child. This method helps only those children whose gelatinous plug comes off on its own on the 14th day, that is, it would come off without putting milk in the eyes. After each daily feeding, the mother should massage the lacrimal sac; it is located at the inner corner of the palpebral fissure. Mom presses on this place and makes up and down movements (6-10 times). If during a massage the pus begins to flow more strongly, then you are doing everything right. The massage must be carried out with sufficient force; a light touch will not bring any effect. The younger the child, the better the effectiveness of treatment. After 6 months, conservative treatment makes no sense at all. Treatment without massage, only by rinsing and instilling an antibiotic, will relieve inflammation, but after stopping treatment, the problem may recur, since it will only kill the germs, and the canal will remain clogged, which will again lead to illness. Most often, the disease goes away after 2 weeks of treatment. If the situation has not changed, then the doctor rinses the lacrimal canal. To do this, the child is given local anesthesia with special drops, then the ophthalmologist inserts a special probe and cleans the tear duct, after which he rinses with an antibiotic. Antibiotic therapy of the eye is carried out for some time after the procedure at home. Re-piercing the channel is usually not required. But if you delay treatment for up to 6 months, then you may even need surgical intervention, since after six months the gelatinous film becomes connective tissue with cartilaginous elements, that is, removing the plug with a probe will be problematic. Most often, dacryocystitis resolves after conservative treatment, and even cleaning the lacrimal canal with a probe is rarely required. Your calmness and compliance with the doctor’s instructions and prescriptions will quickly relieve your baby of this problem.