Normally, a child’s skin color is light pink without any foreign elements of rash or petechiae. In pathological conditions, the skin color of newborns may acquire slightly different shades. Thus, during an attack of suffocation, cyanosis develops - this is the coloring of the epidermis in the poisoned areas in a bluish and bluish tint. If such a symptom appears, you should immediately begin providing first aid to the baby. Any change in skin color in a child indicates the manifestation of clinical signs of a particular disease. Therefore, do not ignore such symptoms. This article describes what changes in the color of the skin can occur and how to properly respond to their appearance in a baby.
First of all, it is worth remembering that if the skin color of newborn babies changes, you should immediately report this to your local pediatrician, who monitors the condition and development of the child. In emergency cases, you should call an ambulance team.
A newborn's skin color may be different from what their parents imagined. Regardless of the baby's race, the typical color of a newborn baby ranges from dark red to purple. It may change several times over the next few days. It will take at least six months for the skin to achieve a permanent color.
Physiological peeling
If a newborn's skin peels, then this is a physiological phenomenon. Refers to the norm. This condition is observed a day or a day and a half after the baby is born, but mainly in post-term babies. Lasts for about three weeks.
Despite the fact that this phenomenon is considered normal, you should still see a doctor to rule out congenital ichthyosis.
For peeling, a good care product is an ointment called Bepanten. But you can also use ordinary baby cream (unscented).
Telangiectasia
This is the name of capillaries, or rather their dense network, appearing in the form of spots. The main location of such spots is the back of the newborn's head or forehead, sometimes they are located on the baby's eyebrows and eyelids. Telangiectasias disappear if you press on them, and become even brighter when the child starts screaming.
This phenomenon lasts much longer than erythema or physiological peeling. It goes away by the age of one and a half years. For the disappearance of telangiectasia, you do not need to make an effort or search for a treatment. The spots go away on their own, without any effort on the part of the mother.
Mongolian spots
This physiological formation is found only in babies belonging to the Mongoloid race, as well as in dark-skinned newborns. Location: lumbosacral region, shoulder blades, buttocks. The color of the spots is blue or purple, their shape is irregular, and their sizes vary. If you press on the “Mongolian” spot, it does not disappear. Basically, this is a solitary phenomenon, but there are exceptions.
Blue spots disappear by five, maximum six years.
Sebaceous ichthyosis
This phenomenon occurs due to the strong secretion of sebum, which dries out quite quickly. And the result: dry skin, even rough, its color becomes brown. Further, cracks may form on the crust. The whole process ends a week after it begins with peeling, or the newborn’s skin begins to peel off. Afterwards the cover takes on a normal appearance.
Despite its apparent complexity, this phenomenon is not considered a disease. The child’s condition is normal, without disorders or impairments; there is no need for therapy.
Skin care for a newborn during this period can be done as follows:
• warm baths.
• lubrication with cream (it is better to use lanolin or dexpanthenol).
Sebaceous ichthyosis must be distinguished from congenital. Therefore, you should never make a diagnosis yourself! You should definitely consult your pediatrician.
What color is the baby's skin
One of the important indicators of a child’s health is his skin and its color; healthy skin has a uniform color, a pale pink color and, depending on the temperature, due to the expansion of the skin, it can change its color from pale to quite bright, almost red. Skin color in children depends on many external and internal factors, and often depends very much on their state of health. An experienced doctor and an observant mother can suspect many diseases and health problems based on the color of the baby’s skin. Therefore, during examination, attention is paid first of all to the color of the skin, and then this is noted on the card. But which skin color changes should you be most concerned about? What should you pay attention to?
What if your skin is pale?
Skin color depends significantly on how actively the skin is supplied with blood thanks to a network of small vessels (capillaries). Color under normal conditions depends on the structure of the skin of each baby, as well as on physical activity and ambient temperature. In hot weather, the skin may turn red due to the expansion of the skin, and in cool weather there may be centralization of blood circulation to the area of internal organs. In addition, the skin usually turns pale when blood pressure decreases and its quantity decreases in the area of small skin capillaries.
Often, quite pronounced pallor of the skin occurs in children with iron deficiency and other types of anemia, with swelling of the skin and with circulatory problems with problems with blood supply to small skin vessels. Disruption of blood microcirculation in small vessels can occur with heart failure or damage to the heart by diseases such as diphtheria, pneumonia, with heart defects or with infection of the heart itself (endocarditis or myocarditis). Also, pale skin can occur with kidney diseases, for example, glomerulonephritis, as well as with shock and collapse (a sharp drop in pressure to almost zero), with severe fear, pain or freezing.
Pallor of the skin spread throughout the entire body may indicate anemia (low blood hemoglobin), which may be due to disturbances in the formation of red blood cells due to deficiency of iron or other substances, due to impaired synthesis of red blood cells by the bone marrow (aplastic form of anemia), with excessive destruction of red blood cells due to hemolysis, with acute bleeding or with chronic small blood losses, with malformations of hemoglobin itself. With such anemia, the skin is waxy pale, with a slight yellowness, there may be other signs of hemoglobin deficiency, problems with nails and hair.
A child's skin may be pale due to thickening of its upper layers, which does not allow the capillaries to show through. This condition can occur with edema with a sharp decrease in the amount of proteins during glomerulonephritis, with nephrotic syndrome, with intestinal damage and impaired absorption of nutrients, and with severe burns. Also, pale skin due to swelling can occur with hypothyroidism, low thyroid function, or vitamin A deficiency. In rare cases, pale skin is caused by hereditary thickening of the skin or obesity. It is important to be able to distinguish the pallor of the skin due to anemia (due to a decrease in the level of hemoglobin or red blood cells) from the pallor that occurs with vascular spasms. In this case, you need to look at the area of the mucous membranes - gums or cheeks. With anemia they are also very pale, with vasospasm they are pink.
In special cases, pallor can have specific shades - yellowish with hemolysis, destruction of blood cells, waxy with impaired synthesis of blood cells in the bone marrow, with infections and heart damage, pallor can have a “coffee with milk” skin tone, with purulent damage to organs, pallor can be from earthy-gray to greenish with dehydration and toxicosis. A special form of pallor can occur when there is a deficiency of the melanin pigment in the skin due to a special disease - phenylketonuria or albinism, then the child will also have colorless nails, hair and eyebrows with eyelashes.
What if your skin has a yellow tint?
Sometimes the child’s skin color acquires various shades of yellow - from almost orange, ocher to yellow-green, olive. Yellow skin does not always mean that a child has jaundice; yellowness can occur even in healthy children - this is the so-called “carotene jaundice” when eating a large amount of yellow foods (carrots, pumpkin). Then the tip of the nose, feet, and palms become stained, but this is not dangerous and does not require treatment. But often jaundiced skin is a sign of serious pathologies - for example, during hemolytic processes, when red blood cells are actively destroyed in the bloodstream, a lemon-colored yellowness occurs; with jaundice caused by a violation of the outflow of bile from the liver (obstructive jaundice), the skin becomes light olive in color. With infectious and toxic jaundice with damage to the liver tissue itself and the accumulation of hemoglobin in the skin, an orange-yellow tint of the skin appears. In this case, yellowness will appear not only on the skin, but also on the mucous membranes of the mouth, in the area of the sclera of the eyes, and manifestations from the internal organs are also observed.
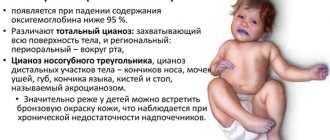
What if the skin turns blue?
Blueness of the skin or cyanosis is the color of the skin from bluish to plum and almost dark cherry colors, while both the skin and mucous membranes can turn blue. With cyanosis, blood stagnates in the area of the venous network with difficulty in its outflow from peripheral vessels. Skin cyanosis is visible to the eye if the amount of oxygen in the blood decreases to less than 15% of the required level. The severity of cyanosis depends on the number of capillaries under the skin, the thickness of the skin and the amount of pigment in the skin (degree of tanning). In children, cyanosis can be of two types - local (regional), in certain areas of the body, and total.
With local or regional cyanosis, blueness can be perioral, located around the mouth, near the nasolabial triangle, as well as on the tip of the nose, in the area of the earlobes, on the lips, on the tongue, in the area of the child’s feet or hands. Typically, cyanosis is detected in children with problems with breathing and heart and blood vessels. If the problem is in the lungs, cyanosis may result from the blood not being well oxygenated as it passes through the respiratory system. This disease often occurs with congenital heart defects - then venous and arterial blood partially mixes in the heart, and in this form enters the vessels.
Milia
This is the name given to small cysts that develop from the sebaceous glands. They appear in more than half of newborns right from the moment of birth and are white in color. Their size is small, the area of distribution is the forehead, nose and cheeks. In babies born prematurely, papules may appear on the arms, legs or torso.
They go away on their own approximately a month after the baby is born, without any treatment.
The color of a child's skin is often an indicator of the presence or absence of health problems. If your newborn has a yellowish or blue tint that does not go away, this is a reason to contact your pediatrician.
Increase in yellow color
More than half of newborns develop jaundice during the first week. This is usually a short-term condition that goes away fairly quickly, but it can be a sign of a more serious illness.
Jaundice is caused by the breakdown of red blood cells. When old cells are destroyed, hemoglobin turns into bilirubin and is usually removed by the liver. In a newborn child, this process is not fully developed. Because bilirubin is colored, it causes the baby's eyes, skin, and tissues to turn yellow. As liver function matures, jaundice goes away.
A premature baby is more likely to develop jaundice. A yellow tint to the skin can often be seen by lightly pressing on your baby's forehead or chest.
There are several types of jaundice:
- Physiological jaundice. Occurs as a “normal” reaction to the body’s limited ability to secrete bilirubin in the first days of life.
- Breast milk jaundice. A very small number of breastfed babies develop jaundice between 2 and 12 weeks of age.
- Jaundice from poor breastfeeding. Babies born early may have problems breastfeeding and may also develop jaundice.
- Jaundice from hemolysis. Jaundice can occur when red blood cells break down due to hemolytic disease of the newborn, too many red blood cells, or internal bleeding.
- Jaundice associated with poor liver function. The disease may be due to poor liver function due to infection or other factors.
Treatment for jaundice depends on the cause and extent of the disease and includes phototherapy. Babies with severe forms may require hospitalization and blood transfusions.
Children suffering from jaundice may have problems feeding or become lethargic and irritable. Call the doctor if your baby has any of these signs.
The blue color that doesn't go anywhere
When a baby is born, its skin has a dark red or purple hue. As soon as the baby begins to breathe oxygen, the color changes to red. This redness usually begins to fade within the first day.
A baby's hands and feet, due to the newborn's immature circulation, may remain bluish for several days, and this is normal. But if other parts of the body are blue, it is a cause for concern.
Sometimes a baby's face or lips and mouth may turn purple from very intense crying. But as soon as the baby calms down, the skin should turn pink again.
If the color does not turn pink again, or has an overall blue tint, this may signal a problem and is called cyanosis. This condition is often seen in children with heart defects due to the heart's inability to pump oxygenated blood to the rest of the body.
Difficulty breathing can also cause cyanosis. If your baby has a blue tint to his skin, consult a doctor immediately.
Reference - stlouischildrens.org/conditions-treatments/skin-color-changes-newborns
On Vikids you can:
Find a doctor and make an appointment
Find a clinic and make an appointment
Go to Forum
Read similar articles
Physiological jaundice
Yellow skin occurs in 2/3 of newborns. It definitely goes away and is not a pathology. Care for jaundice is needed as follows:
• bathing with a series.
• compliance with temperature conditions.
• washing (preferably without using soap).
• taking air baths.
• use of moisturizers for newborns, which will reduce itching and dryness.
But the very first step a mother should take is to contact her pediatrician for recommendations.
Rules of care
The skin of a newborn in the first months of life is thin and vulnerable. Care must be taken to ensure that its integrity is not compromised. To do this, you should carefully trim your baby's nails - this way he won't be able to scratch himself. You also need to protect the baby from contact with sharp objects. The child needs to be bathed regularly. The optimal frequency of water procedures is 1-2 times a day. Particular attention should be paid to the folds, washing them thoroughly. This way you can prevent the appearance of diaper rash and wounds. If dryness appears on the body, these areas of the skin should be lubricated with rich baby cream or special oil. It is important that the components of cosmetic products are safe for the baby.
For urticaria and minor inflammations, you can bathe the child in a decoction of chamomile, sage or a weak solution of potassium permanganate. For marbled skin, the doctor may prescribe massages to speed up blood circulation. A balanced diet appropriate for your age is also important. It is imperative to observe the temperature and humidity conditions. It is advisable to leave the child without diapers and diapers as often as possible - air should flow freely to the body.
A baby's skin is very vulnerable in the first months and therefore requires special care and attention. Any changes in it should be discussed with your pediatrician. In addition, it is important to be able to maintain its normal condition. This does not require much effort - you just need to regularly carry out all the necessary hygiene procedures.
Rate this article: 4.8 4.8 out of 5 (5 votes)
Marbled skin in a newborn
This phenomenon can be attributed to both normal and pathological conditions. There is no need to be scared, you just need to consult your pediatrician. Normally, this condition is explained by the fact that the development of the vascular system is still ongoing, the skin of infants is very thin, and therefore reacts to every impact. Especially the cold. According to observations, the marbled color of a newborn’s skin is most pronounced when the room is cool. As soon as you dress your baby warmly, the skin will return to its normal shade.
Pathological manifestations of marbling are intrauterine hypoxia, anemia, etc. The norm or pathology in a baby with marbled skin coloring must be determined by a doctor.
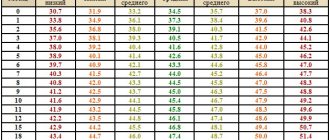
Norm of bilirubin by day in newborns
A newborn baby's blood is taken for analysis. This is necessary in order to keep all the most important indicators under control. The doctor pays special attention to the level of bilirubin in the blood.
Bilirubin norms in infants:
- day from birth – up to 85 µmol/l;
- 2 days from birth – up to 180 µmol/l;
- 3 -5 days – maximum value 256 µmol/l;
- 6 - 7 days - maximum value 145 µmol/l;
- 8 - 9 days - maximum value 110 µmol/l;
- 10 - 11 days - maximum value 80 µmol/l;
- 12 - 13 days - maximum value 45 µmol/l;
Prickly heat
The baby's body reacts to overheating because his sweat glands are still clogged. The phenomenon of heat rash occurs in 15% of children.
The emergence is promoted by:
• high room temperature.
• high humidity in the room.
Therefore, it is worth paying great attention to the room for a newborn. There is no need to assume that the room where the baby is located should be hot. This is far from true. Moreover, it is worth controlling the humidity. Warm and dry conditions must be created in the room and it must be ventilated frequently.
Miliaria is localized anywhere, but most often: on the skin in the groin, torso, and armpit. With heavy sweating, rashes on the skin of newborns can also appear on the face, neck, and scalp.
Although such a phenomenon as prickly heat is considered a borderline state between normal and pathological, lack of care can lead to infection.
The treatment here is:
• baths with potassium permanganate.
• products that have a drying effect (powder).
But the best thing is prevention: ensuring a normal temperature in the room, ventilating it, bathing the baby every day, and systematically taking air baths.
Newborn acne
Appear 2 weeks after birth. Boys are mostly affected, especially those who are breastfed. Most often, rashes appear on the scalp. There are suggestions that this phenomenon is associated with hormonal changes that occur after childbirth in the mother’s body.
In this borderline case, treatment is required, or rather treatment:
• 30% alcohol solution.
• powder.
• zinc-based paste.
All procedures should be carried out only after consultation with a doctor.
Additionally, the nutrition of a nursing mother is adjusted: the volume of fluid she drinks increases, a diet based on dairy and plant products is recommended.
In especially severe cases, antibacterial treatment is prescribed.
Features of newborn skin
After birth, the baby encounters the outside world for the first time, and his body immediately begins to adapt to his new environment.
In this adaptation process, the skin of a newborn is especially vulnerable. This is due to two components: its anatomical and physiological characteristics and the influence of aggressive factors.
What you should know about baby skin is that it:
- is easily injured due to its structural features: its stratum corneum is thin and loose, the epidermis is loosely connected to the dermis.
- easily infected: immunity is not fully formed, there is insufficient protective acidic environment on the surface of the skin.
One of the most common reactions of a baby's skin to aggressive external irritants is diaper rash.
What does diaper rash look like?
Typically, these are pink and red areas of varying sizes or rough red patches. Most often, diaper rash appears in the perineum, groin, axillary and cervical folds, between the buttocks and behind the ears 1.
This may seem unusual, but diaper rash appears on the baby’s skin even due to his movements, since this causes the destruction of the natural protective layer of lipids on the surface of the skin.
But still, such areas are primarily found on the skin under diapers
What to do if diaper rash appears?
There are mild and severe forms of diaper rash. If diaper rash is mild, which means that there is little redness on the skin, then the main attention should be paid to hygiene procedures and regular air baths. In such cases, the damaged areas of the skin will be lubricated quite often, especially after bathing the child, with special external agents, for example, Bepanten ointment containing provitamin B5 and lanolin.
If bright red spots, microcracks, erosions and ulcers appear on the skin, then this may be a sign of a severe form of diaper dermatitis. Important: if diaper dermatitis (diaper rash) is not treated, deep skin damage may occur with the addition of bacterial and fungal infections1.
Prevention of diaper rash
The best way to combat diaper dermatitis is to prevent it. It consists primarily of observing basic hygiene standards. This means:
1) timely replacement of diapers. For example, it is necessary to change the diaper immediately after a night's sleep, without delaying it until later, because it is easy to imagine how much discharge has accumulated there during the night. Be sure to put on a clean diaper before bed and after feeding your baby. In general, the diaper should be changed at least every three to four hours;
2) carry out so-called air baths, during which the child remains without a diaper for some time so that his skin can breathe;
3) to prevent diaper rash, you can introduce daytime bathing into your child’s daily routine, it certainly won’t be unnecessary;
4) it is strictly not recommended to treat a child’s healthy skin with antibiotics. This can lead to a significant disruption of the skin microbiocenosis and contribute to the development of fungal infection1;
5) barrier protective ointment must be used every time you change a diaper. Such products form a lipid film on the surface of the skin, thereby protecting it from irritation upon contact with feces. The ideal barrier drug for children is considered to be the one that has proven effectiveness in use. The ointment must be hypoallergenic and free of preservatives, flavors and dyes1. It is strictly not recommended to use creams and ointments for adults. They often contain components that can harm the baby’s sensitive skin.
More about medicines
The mentioned ointment “Bepanten” protects the child’s skin from irritants1, has an anti-inflammatory, softening and regenerating effect. The high effectiveness profile of the ointment has been confirmed by numerous clinical studies, and the ointment does not contain any preservatives or dyes.
The effect of Bepanten ointment is due to the presence of an active component in it - provitamin B5. It enhances the protective properties of the inner layers of the skin, stimulates the development and formation of the stratum corneum of the epidermis.
Another important auxiliary component of the ointment is lanolin in high concentration. This substance penetrates the stratum corneum of the skin and provides softening and moisturizing to the skin. Lanolin protects the skin from adverse external factors, forming a thin, breathable film on its surface, and (this is important!) prevents skin friction in folds, which is one of the causes of diaper dermatitis1.
In conclusion, it is worth recalling that it is easier to prevent any disease than to treat it for a long time and persistently. It is better, even in the absence of signs of diaper dermatitis, to apply ointment to the baby’s skin at each diaper change - then your child will not be afraid of any diaper rash.
1 Vasilevsky I.V. Optimization of skin care in newborns and infants // International reviews: clinical practice and health. - 2015. - No. 1. — p.5-18.
2 Ebner F., Heller A., Rippke F., Tausch I. Topical use of dexpanthenol in skin disorders. Am J Clin Dermatol. 2002; 3(6):427−33.
3 In a comparative randomized study involving 62 newborns, none of the children who were prescribed Bepanten ointment for prophylactic purposes (n=40) developed diaper dermatitis during their hospital stay, and no adverse reactions were observed. Yatsyk G.V., Akoev Yu.S. Clinical effectiveness of various skin care products for newborns based on Consilium medicum D-panthenol. Appendix // Pediatrics. − 2004. − No. 6 (2).
Erythema toxicum of the newborn
Almost 50% of newborns suffer from erythema toxicum. It appears around the 3rd day of life. The cause is not entirely clear, but it is believed that this phenomenon is an overreaction of the immune system. And also a factor influencing the appearance of erythema is the mother’s diet, which contains pronounced allergens (chocolate, citrus fruits).
The disease begins with allergic manifestations: dry skin, red cheeks. But at the same time, the child’s condition is normal and does not cause alarm. Sometimes treatment with antiallergic drugs is prescribed.
Toxic erythema is treated:
• diet for mother (hypoallergenic).
• treating rashes with brilliant green.
After a few days, with proper care, the skin clears up.