Every expectant mother dreams of breastfeeding her baby, because breast milk is much healthier than formula milk. But, faced with reality, many refuse this. The main motivation is pain during and after feeding. But this can be eliminated and you can continue to feed the baby with healthy mother’s milk.
It is important to learn what to do if your breasts hurt after feeding and find out whether you need to see a doctor. You may be able to help yourself on your own. Often, pain during feeding occurs only as a result of improper attachment of the baby. But there are also more compelling reasons when medical attention is required. In order to prevent this kind of trouble in time, you should study everything related to breastfeeding. Pain in the mammary glands will be discussed in more detail later in the article.
Types of pain syndrome
Breasts can hurt in different ways during and after feeding. A nursing woman needs to listen to her feelings and figure out how dangerous the presented pathology is.
Characteristic features of painful sensations include:
- In the first few days after birth, the uterus contracts to its normal size. This process is influenced by the production of the hormone oxytocin, which is produced by the woman’s body. The hormone production mechanism begins to work after the baby is put to the breast and continues for some time after the end of each feeding. At this time, the woman feels a tingling sensation in her chest, and this will continue for 4-5 days.
- When feeding, pain first occurs in the nipples, and then spreads to the entire breast and continues after. The sensation of pain is quite strong and the reasons for this may be: the presence of abrasions and cracks on the nipples or the presence of a non-standard nipple shape.
- If the breasts are hard and painful, and the skin is pale in appearance and has an uncharacteristic shine, then this may be stagnation of milk (lactostasis). The pain occurs due to the rapid presence of milk, which compresses the ducts with its mass.
- If measures are not taken, lactostasis can develop into mastitis. In this case, the skin becomes red, the mammary gland is swollen and very painful. If you have additional chills, malaise and high fever, you should consult a doctor.
This is important: These causes of chest pain can be prevented, and some can be easily tolerated. If mastitis occurs, only a doctor can help. Under no circumstances should you self-medicate. Until you receive qualified help, you can carefully express milk and apply ice in between feedings.
Preventing pain during breastfeeding
Of course, when talking about the causes of chest pain during breastfeeding: how to treat such manifestations, it is necessary to dwell on the prevention of chest pain during breastfeeding.
Let us remind you that a slight tingling sensation in the mammary glands is considered normal. To avoid pain in the mammary glands during lactation, you need to remember that:
- During pregnancy and lactation, you need to abandon the usual perfumed personal hygiene products in favor of baby soap, for example, or other natural-based products;
- Maintain reasonable hygiene, shower no more than twice a day and do not fanatically wash the mammary glands before feeding. The fact is that there are special glands on the skin that not only moisturize the nipples, but also disinfect them;
- You need to remember about the correct application of the baby to the breast: it must be completely turned towards the mother and capture the entire areola;
- If the baby is full, but does not release the breast, the little finger is inserted into his mouth and the mouth opens. If you pull out the nipple by force, this will lead to cracks;
- You need to walk topless for some time every day, so to speak, take air baths;
- It is good to follow the feeding schedule and not be late with it, then there will be no stagnation of milk in the mammary glands and you will avoid unpleasant sensations and even pain during feeding;
- Monitor the weather outside and dress accordingly to avoid hypothermia;
- After giving birth, you should not be embarrassed to ask medical staff for help feeding your baby. This way you will quickly learn how to feed your baby correctly;
- You also need to remember to express milk if there is a lot of it;
- When temporarily or partially transferring the baby to feeding from a nipple, you need to again monitor how he will attach to the breast;
Cracks in the nipples are not only a source of pain, and often unbearable, but also a gateway for infection, and there is not far to an inflammatory process, so they need to be treated; If any discomfort occurs, you should contact a doctor, remembering that now not only your health, but also the life of your baby depends on you.
Incorrect attachment to the breast
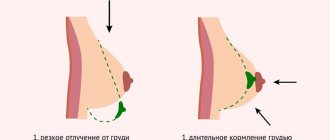
The most common cause of pain is considered to be improper attachment of the child to it. An inexperienced mother who practices breastfeeding cannot quickly learn how to do it correctly. Sometimes in the first days so much milk is produced that the newborn is not able to suck it all out. Then the body adjusts to the child’s needs. In the first days, so that the baby does not choke on the pressure of milk and there is no stagnation, it is necessary to partially express it before feeding.
Video
When there is a sudden production of milk, a woman feels colitis and aching in her chest - this is due to the fact that the hormone oxytocin causes the muscle cells around the milk sacs to contract and release it out. After a few days, the body adjusts to breastfeeding. You also need to learn how to properly attach your baby to the breast to avoid cracked nipples, stagnation of milk and mastitis.
Please note: Feeding a newborn is a serious and responsible process. Therefore, it must be made comfortable and pleasant for mother and baby, and this is only possible with proper attachment to the breast.
There are certain rules for this:
- The nipple should be grasped deeply; the entire areola should be in the mouth, not just the nipple, but if the areola is too large, then only part of it. The nipple should almost touch the soft palate. If everything turned out correctly, then the lower lip should be turned out, the tongue should be placed under the chest, but not protruded, and the cheeks should be puffed out. To perform the presented maneuver, you should force the baby to open his mouth wide. To do this, you need to pass the nipple along the baby's lower lip - this will trigger the feeding reflex, and he will open his mouth.
- Place the breast in the baby's mouth - you need to aim the nipple at the top of the open mouth and pull it closer to you.
- During the process, the baby's nose should touch the breast with its tip, and the chin should rest against the mother. If this does not work, then the breast will slip out of the baby’s mouth, and only the nipple will remain in it. This is not suitable for feeding - the baby will not get enough this way. There is no need to be afraid that the child will not be able to breathe, since the nose is pressed to the chest - if the nostrils are open, then everything is in order.
In order to learn how to properly feed a baby, it is worth inviting a woman experienced in breastfeeding or consulting with a specialist. Basically, a woman is taught to feed a newborn in the maternity hospital.
Possible causes of pain
Breastfeeding experts identify several factors that provoke discomfort when breastfeeding a child. Some of them can be combined, increasing the already severe pain syndrome.
So, a possible cause of pain in the mammary gland may be:
- incorrect grip of the nipple by the child;
- cracked nipples;
- breast candidiasis (thrush);
- lactostasis (milk stagnates);
- inflammation of the mammary gland (mastitis);
- vasospasm.
It is necessary to more carefully consider all these provoking factors in order to understand how to relieve a woman of pain.
Wrong grip
Some experts in matters of feeding believe that it is the child’s incorrect grasp of the nipple that is the main prerequisite for the occurrence of painful sensations in the mammary gland during lactation.
It is this kind of erroneous capture that often leads to other undesirable consequences: cracks, mastitis.
If the baby does not grasp the nipples correctly, the woman may feel severe pain when feeding. In this case, you must immediately stop feeding and wait until the baby takes the nipple correctly.
Only after this a pleasant feeling will appear, and the baby will begin to drink the milk completely.
The procedure for optimal latching of the nipple by the baby should be accompanied by certain maternal actions:
- First you need to wait until the child opens his mouth wide. If this does not happen, you should run the papilla along the lower lip. Usually, after such an action, the sucking reflex, which is innate, is “triggered.”
- The next step is to pull the baby's head towards the bust. The mother needs to “hook” the child’s mouth onto the papilla in such a way that the small breast areola remains visible. If the nipples are grasped correctly, they are located at the same level with the lingual spine, which means that the child cannot damage them in any way.
- If the child’s grasping fails, the woman needs to tighten the areola. To do this, the thumb is located on top of the areola, and the index finger is located below. The skin tightens, forming a kind of “fold”, then it is placed in the child’s mouth and lowered. After the voiced actions, the areola straightens, thereby providing the necessary grip.
The order of the mother's steps should not depend on the position during feeding. If the child develops normally, he will very soon “understand” what is required of him, and the mammary gland will no longer suffer.
What can interfere? First of all, milk will begin to reach the baby with great difficulty if he has a shortened frenulum or a violation of the structure of the upper palate.
In such situations, you need to contact facial surgeons (for cleft palates) or dentists to trim the frenulum. Such operations are now quite common and are performed only by qualified specialists.
Cracked nipples
During lactation, the mammary glands can also hurt due to cracked nipples. There are several factors that provoke damage to the skin of the nipple. Sometimes they occur in combination, increasing the pain.
- Incorrect latch on of the breast. The child grasps only the edge of the nipple, lowering the area around the nipple, resulting in mechanical damage and, accordingly, cracks.
- Infectious lesion. Due to a violation of the integrity of the skin, an infectious agent - a fungus or bacterial particles - penetrates into the chest. In such a situation, unpleasant symptoms begin to disturb the nursing mother constantly.
- Incorrect breast hygiene. Some inexperienced mothers wash the mammary glands after every meal with a soap solution or disinfect them with alcohol. Such hygienic procedures only help to dry out the skin of the nipple; in addition, the lubricating layer produced by special glands is washed away. As a result, nipples are defenseless against damage and pathogens.
- Abrupt end of feeding. The baby sucks milk until he is satisfied. However, some mothers themselves pull out the nipples from the baby’s mouth in order to end a prolonged feeding. Such actions provoke the occurrence of cracks, which is why experts recommend waiting until the baby loosens his grip and refuses the nipple. If the baby falls asleep and does not loosen his grip, you need to carefully push your little finger into the mouth so that you can easily remove the breast.
- Failure to follow instructions when using a breast pump. Another provoking factor is that milk is expressed with a special device at high speeds or too often. In this situation, cracks appear gradually, but over time they can turn into deep “grooves.”
If shallow cracks form, you just need to exclude all of the above factors: teach the child to grasp correctly, forget about frequent washing of the breast and stop taking the breast from the baby.
However, if the mammary gland is damaged too severely or infectious inflammation is involved, you must consult a doctor for appropriate therapy.
- The doctor will select medications aimed at combating the fungus or bacterial pathogen, if any. Milk remains in the child’s diet, since many drugs do not necessarily require cessation of natural feeding.
- Most likely, you will need to select special ointments and gels designed to heal wounds. This should also be done by a professional. The most popular products are Bepanten, Actovegin, Sudocrem, Zinc ointment. Sometimes folk recipes help - the mammary gland is smeared with sea buckthorn or cedar oil.
- Experts recommend walking bare-breasted more often during lactation (before and after feeding). If this advice is not feasible, use loose underwear made from natural materials. To prevent nipples from rubbing against things, you need to use special breast pads.
When connecting various infectious pathogens to cracks, it is not recommended to deal with this problem on your own. If a fungus is involved, thrush may develop, if bacteria are present, mastitis may develop.
Thrush
Cracked nipples and other damage to the skin of the mammary gland often lead to fungal infections. The first symptom is a whitish coating covering the nipples, spreading to the baby’s gums and cheeks after feeding.
It is painful for a woman to breastfeed, the pain syndrome persists even during rest, this happens when pathogens penetrate deep into the milk ducts. Thrush occurs when the immune system is weak, hormonal imbalance or due to poor breast hygiene.
In a child, the symptoms of candidiasis are as follows:
- in addition to the whitish coating, redness, swelling of the oral cavity appears, and blisters appear;
- after a certain period of time, plaque begins to cover the entire surface of the cheeks, tongue, penetrates the larynx, as a result of which erosive damage to the throat mucosa can develop;
- the child is worried, constantly cries, does not drink milk, begins to lose weight;
- with the development of candidiasis in the corners of the lips, the painful sensations only intensify as bleeding cracks form;
- high temperature, and there are no other reasons for its increase (a cold or teething).
A nursing mother should consult a doctor who will select the necessary medications to fight the fungal infection. If treatment is successful, the mammary gland will soon recover, and treatment can be continued.
The doctor will also recommend medications to treat candidiasis in the child.
Lactostasis
Milk can stagnate in the breast for various reasons - for example, the mother’s refusal to breastfeed on demand. Due to lactostasis, the mammary gland noticeably hurts when the child eats food.
Breastfeeding experts recommend that mothers remember that not only the baby may demand to eat, but also the woman can freely put the baby to the breast after she feels fullness in the breast. This must be done regularly, otherwise the milk will stagnate, which will lead to lactostasis.
If, however, one or the other mammary gland becomes ill and the woman suspects lactostasis, you should pay attention to the following signs: stagnation is accompanied by hardening of individual areas of the breast, swelling, and elevated temperature.
The main methods against milk stagnation are:
- resorption of a certain mammary gland by the child;
- massaging hard areas in the damaged breast.
Most often, the mammary gland stops hurting after a few days, but with severe lactostasis, unpleasant sensations during feeding can be observed for another week.
Mastitis
Inflammatory processes occurring in the mammary gland are called mastitis. Inflammation develops as a result of severe congestion in the chest. Another reason may be damage to the breast (cracked nipples) after the penetration of infectious pathogens.
Experts include the following manifestations as the main symptoms of lactation mastitis:
- obvious swelling of the affected tissues;
- mammary glands are painful;
- the skin color of the affected area is red or bluish;
- heat;
- chills reminiscent of flu fever;
- after expressing, the milk has purulent inclusions (in severe cases of the disease).
At the initial stage of the inflammatory process, it will be enough to apply cold to the mammary glands and completely empty the breasts (feed the baby more often or express milk).
If pus comes out with milk, we are no longer talking about breastfeeding. What should a nursing mother do? Doctors prescribe antibacterial drugs, and in particularly advanced cases, surgery. If mammary glands affected by mastitis are not treated, their deformation, blood poisoning, and even the death of the woman are possible.
Vasospasm
If a breastfeeding mother has pain in her mammary glands while feeding her baby or after it, the discomfort manifests itself in the form of painful pulsation, the nipples begin to turn white after the procedure, she is probably suffering from vasospasm. It is diagnosed quite rarely.
The Canadian scientist Newman was the first to describe this condition in detail. The symptoms described above, he believed, arise due to spasms of small vessels located next to the breast nipples.
The reason for the development of spastic phenomena is the temperature difference between the environment and the warm oral cavity of the child. The baby releases the nipples, due to spasms, blood flow to them stops, this leads to a painful syndrome.
If such symptoms constantly occur during breastfeeding, when the baby lets go of the nipple, it is better for the mother to consult a doctor to rule out various autoimmune diseases that also provoke vasospasm.
Experts recommend doing the following to prevent spastic reactions:
- keep the mammary glands warm all the time, immediately covering them after feeding;
- avoid drinking coffee drinks and strong black tea;
- visit a massage therapist and perform breast massage.
Lactostasis
In the first weeks after the start of lactation, the baby does not eat the offered volume of milk, so stagnation in the ducts may form - lactostasis.
Important! If you do not take any measures to eliminate it, mastitis may develop - inflammation of the mammary gland.
If your breasts ache after feeding and lumps are felt in it, and the area becomes bluish, burns or burns, then stagnation has formed. It is also provoked by constant pumping of milk after feeding, hypothermia and squeezing the breasts with tight underwear or sleeping on the stomach.
You can eliminate it yourself by doing the following:
- Carefully express a noticeable amount of milk.
- In order for the stagnation to resolve, you should put the baby on your chest more often, pressing his chin to the place of compaction. If you cannot feel the seal, apply it to the sore spot.
- Make a cold lotion by wetting and wrung out a towel and applying it to the sore spot for 5-7 minutes.
- You can apply a cabbage leaf to the sore area to relieve inflammation and swelling.
This should be done immediately so that stagnation does not turn into mastitis.
Video
Chest pain: when is there nothing to worry about, and when do you need to see a doctor urgently?
Chest pain can signal the occurrence of lactostasis. To reduce pain and reduce the risk of developing mastitis, it is recommended to take Lactanza - the first probiotic for the breast, helping to maintain healthy breastfeeding.
Lactobacillus Lc40, which is part of Lactanza, is absolutely safe and allows you to regulate the number of pathogens in the gland. Reception can be started at any period of breastfeeding.
It is important to remember that measures to prevent lactostasis are effective provided that breastfeeding is properly organized.
Consult your doctor before use
One of the most common reasons for transferring a baby to artificial feeding is the painful sensations in the breasts that a woman experiences during feeding. Let's talk further about why chest pain occurs, how dangerous it is and whether it can be avoided.
Reasons not to worry about
There is no need to curtail feeding or urgently go to the doctor if breast pain during breastfeeding is associated with sudden flows of milk. It is not difficult to recognize this process - the woman experiences a feeling of heaviness and fullness in the mammary gland, at the same time unpleasant sensations appear in the lower abdomen, similar to the sensations during menstruation, and leakage from the nipples may begin.
Over time, when the feeding regime improves, the body will learn to produce milk in accordance with the schedule proposed to it and the pain will go away. And at first, the way out of the situation will be more frequent feeding or pumping.
They should not be neglected, otherwise in the future the mother can expect lactostasis - stagnation of milk in the breast with accompanying discomfort and soreness of the mammary gland.
Another completely natural reason is that the skin of the nipples is too delicate, on which microcracks form when the baby actively sucks. Their appearance is accompanied by sharp pain during GV with a hint of burning.
Here, perhaps, we should digress and talk about how to avoid microcracks in the nipples.
Firstly, it is important to teach your baby to latch on to the breast correctly. The baby should grasp not only the nipple, but also part of the areola with his lips. The nipple should rest against the baby's palate. In the process of mastering this science by mother and newborn, most women experience nipple pain to one degree or another during breastfeeding, but with the right approach, the discomfort goes away within a few days.
Secondly, it is necessary to establish competent breast care. The most common mistakes to avoid are:
- washing too often;
- too hot water;
- use of aggressive hygiene products.
Cool washing with baby soap or delicate gel will help reduce discomfort. In addition, you can lubricate your breasts after feeding with vitamin B cream or ointment.
Read more about cracked nipples here.
Thrush while breastfeeding
If cracked nipples are not treated in a timely manner, they become a real incubator for pathogenic bacteria: high temperature, humidity and the presence of a nutrient medium in the form of microparticles of milk allow them to multiply at high speed.
This is how candidiasis occurs, commonly called thrush. The disease not only causes severe pain during breastfeeding, but also provokes the development of stomatitis in the baby. And this is already a reason to see a doctor and receive drug treatment.
Lactostasis, mastitis
Lactostasis, which has already been written about above, is also accompanied by unpleasant sensations. If you do not pay attention to them and do not take corrective measures, the next stage is uninfected mastitis.
With this disease, the gland becomes hot and painful, and the woman’s overall body temperature rises. By the way, in this case you need to measure the temperature not under the armpit, but in the elbow bend - the result will be more correct.
In addition, a mammologist or the woman herself may detect small lumps in the breast - one of the most striking signs of the disease.
In the early stages, as a rule, it helps to apply cold water or serum compresses, massage and, of course, the correct position of the breast during feeding, which will ensure maximum emptying of the gland.
If the disease has reached a significant development, the doctor may prescribe physiotherapeutic procedures, treatment with antibiotics compatible with breastfeeding, or even recommend a surgical method to solve the problem.
Vasospasm
Let us note another, not very common, but still quite common pathology - vasospasm, that is, an instant narrowing of the vessels located in the mammary gland. It can be recognized by a specific symptom: a sharp stabbing pain during breastfeeding occurs at the moment when the baby releases the nipple, that is, the gland comes under the influence of a sharp temperature change.
If such symptoms appear, a woman should immediately consult a specialist, since vasospasm can be a consequence of other, more dangerous diseases, including autoimmune diseases.
In addition, it is recommended to keep the “problem” organ warm and not to consume foods that can cause vasoconstriction (mainly coffee and black tea).
There is no need to stop breastfeeding until the causes of cramps are determined.
Mastitis
Mastitis develops if an infection penetrates into the milk lobules. It is very difficult or almost impossible to strain out the resulting compactions yourself. Purulent mastitis is considered the most dangerous. Its symptoms are severe throbbing pain in the mammary gland, purulent discharge from the nipple, weakness and high fever. Doctors do not recommend self-medication - in this case, the patient needs qualified medical care, and quite often, surgical intervention.
Candidiasis
Candidiasis (thrush) very often appears in a pregnant woman and remains after the birth of the baby, “settled” in the mammary ducts and nipples. It also enters the child’s mouth. Symptoms of the lesion in question are itching and burning during the baby’s meal, which intensify towards the end of the meal. In this case, both mother and child should undergo a course of therapy with medications prescribed by the doctor.
This is important: To avoid such problems when breastfeeding, you should wash your breasts with warm water before each feeding and take a shower every day. While washing, you can massage the mammary glands in a circular motion. After each feeding, take air baths for at least 15 minutes.
The article provides detailed answers to the question of why breasts hurt after feeding. It is important to remember that breastfeeding is not only about feeding the baby, but also about communication between mother and baby. Therefore, breastfeeding should be handled responsibly so that both mother and baby feel comfortable.
Pathologies during breastfeeding: treatment
Having felt unpleasant phenomena in the mammary glands, the mother’s first thought is to stop feeding, however, this will only worsen the situation. You need to know about the causes of chest pain during breastfeeding: how to treat it in order to reduce pain as much as possible.
With lactostasis and mastitis, you need to continue feeding; during the process you can get rid of stagnation of milk, while doing this:
- Before feeding, you need to pump, otherwise the baby will not be able to suck milk;
- When feeding, you need to try to ensure that the baby sucks on the sore mammary gland more often and longer;
- To relieve pain, take a cabbage leaf and crush it, then apply it to the breast; such a compress is effective both before and after feeding;
- Before you start feeding, you need to take a warm shower, this will reduce swelling and reduce pain;
- You also need to remember about massage.
Usually, lactostasis is cured in a couple of days; if the pain only increases and does not go away, you need to consult a doctor.
If the pain is associated with infection, then antibiotics are taken according to a doctor’s prescription. If the doctor has prescribed antibiotics, then breastfeeding is postponed for a long period, during which mandatory pumping is carried out.
When treating vasospasm, massage will help if the disease is in the early stages. To do this, lubricate the nipple with oil and massage it; short-term compression of the nipple also helps, but if such actions do not help, this is a reason to consult a doctor.
If you have thrush, you will have to take antifungal medications; if the symptoms are noticeable in the baby, he also needs to lubricate his mouth. You should ask your doctor about what medications are needed to treat thrush; self-medication can lead to prolonged cessation of lactation and worsening thrush.