Why measure?
The frequency of respiratory movements, coupled with the determination of heart rate and type of breathing, is of critical diagnostic importance when examining a newborn and infant. Such children cannot tell their parents what exactly is bothering them, and only by the NPV indicators can one understand that something is wrong with the baby. Most diseases that are accompanied by rapid breathing in children can be successfully treated with timely treatment and proper medical care. The pediatrician, of course, will pay attention to the child’s respiratory rate at each scheduled visit to the clinic.
The rest of the time, parents are guarding children's health; they need to be able to distinguish normal breathing from abnormal breathing.
This is not difficult to do; the frequency of respiratory movements is a parameter that any mother, any father or grandmother of the baby can independently determine. The main thing is to do everything correctly and correctly evaluate the results obtained.
How to measure?
If parents feel that the child is breathing too quickly, the breathing rate should be measured. It is best to do this when the child is calm, for example, in a dream. When the baby is awake, playing, experiencing something, experiencing emotions, breathing becomes more frequent, and this is quite natural.
The mother should place her hand on the baby's chest or belly. The choice of measurement location is very important because it determines the baby's breathing pattern. In infants and children under 4-5 years of age, diaphragmatic breathing predominates (the child breathes with the stomach, the peritoneum methodically rises as you inhale, and descends as you exit).
At 4 years old, a child begins to master a new way of breathing - chest breathing (when the chest rises and falls when inhaling and exhaling). By the age of 10, a child develops the type that is more characteristic of him based on gender. Boys usually have abdominal breathing, while girls have diaphragmatic breathing. Thus, it is very simple to determine the place where to put your hand - you need to start from the age of the child.
The counting algorithm is quite simple. The “inhale-exhale” episodes are counted for 1 minute. One series of such movements is counted as one breathing movement. It is a big mistake to measure your breathing for 30 seconds and then multiply the resulting number by two. Breathing is not as rhythmic as, for example, the pulse, and therefore such a simplified method for measuring respiratory rate is not suitable. Parents will spend another minute measuring the heart rate (pulse) and it will be possible to assess the child’s condition based on age standards.
An electronic watch, a stopwatch or a clock with an arrow will be useful for measurements.
There are a lot of tables on the Internet that suggest comparing the data obtained from measuring the child’s breathing rate with the norms. It is difficult to assess the veracity of each. Pediatricians try to adhere to the data published in Berkowitz's Pediatrics: A Primary Care Approach. They are officially recognized:
- Newborns. Respiration rate - 30-60 times per minute. Pulse – from 100 to 160.
- Children at 1 year old. Respiration rate 20-40 times per minute. Pulse - from 90 to 120.
- Children at 3 years old. Respiration rate 20-30 times per minute. Pulse - from 80 to 120.
- Children aged 6 years. Respiration rate 12-25 times per minute. Pulse - from 70 to 110.
- Children at 10 years old. Respiration rate - 12-20 times per minute. Pulse - from 60 to 90.
Children at 6 months. Respiration rate - 25-40 times per minute. Pulse - from 90 to 120.
Attentive parents will be able to notice any deviation from the individual child's norm. We are talking about the frequency at which a child usually breathes, because one baby has 40 inhalations and exhalations in 60 seconds, while another baby at the same age has only 25. It is clear that in the second case, an increase in frequency to 40-45 will be considered a violation, and in the first case, in a baby with rapid breathing from birth, the same indicators will be the norm. Parents should not ignore their own observations. After all, mothers and fathers know the individual characteristics of their baby better than anyone, even a very good doctor who sees the child for the first time.
Features of frequency, depth of rhythm and type of breathing
Breathing frequency and depth . Children's breathing is frequent and shallow. This is due to the fact that the work spent on breathing in children compared to adults is greater, since, firstly, diaphragmatic breathing, which predominates in children under 3–7 years of age, requires overcoming the resistance of the abdominal organs (in children have a relatively large liver and frequent intestinal bloating); secondly, in children the elasticity of the lung tissue and significant bronchial resistance are high. The respiratory rate in children of different ages is presented in Table 14.
Table 14
Respiratory rate in children of different ages
| Age | Respiration rate in min. | Age | Respiration rate in min. |
| 1–2 months 1–3 years 4–6 years | 35–48 28–35 24–26 | 7–9 years 10–12 years 13–15 years | 21–23 18–20 17–18 |
The respiratory rate in children changes significantly during the day, and also changes significantly more than in adults under the influence of various influences (mental stimulation, physical activity, increased body and environmental temperature). This is explained by the slight excitability of the respiratory center in children.
Until the age of 8, the breathing rate in boys is slightly higher than in girls. By puberty, the respiratory rate in girls becomes higher, and this ratio persists throughout life.
Breathing rhythm. In newborns and infants, breathing is arrhythmic. Deep breathing is replaced by shallow breathing. The pauses between inhalation and exhalation are uneven. The duration of inhalation and exhalation in children is shorter than in adults: inhalation is 0.5–0.6 seconds. (in adults 0.98–2.82 sec.), and exhalation – 0.7–1 sec. (in adults 1.62–5.75 seconds). From the moment of birth, the same relationship between inhalation and exhalation as in adults is established: inhalation is shorter than exhalation.
Types of breathing . In a newborn, until the second half of the first year of life, the diaphragmatic type of breathing predominates. Chest breathing is difficult, since the chest has a pyramidal shape, the upper ribs, the manubrium of the sternum, the collarbone and the entire shoulder girdle are located high, the ribs lie almost horizontally, and the respiratory muscles of the chest are weak. From the moment the child begins to walk and increasingly takes a vertical position, breathing becomes abdominal. From 3 to 7 years of age, due to the development of the muscles of the shoulder girdle, the thoracic type of breathing begins to predominate over the diaphragmatic one. Gender differences in breathing type begin to emerge from the age of 7–8 years and end by the age of 14–17 years. By this time, girls develop thoracic breathing, and boys develop abdominal breathing.
Reasons for rejection
Exceeding the frequency of respiratory movements in medicine is called “tachypnea” . This is not a disease, but just a symptom that may indicate the development of a certain pathology. We can talk about tachypnea if the respiratory rate differs from the norm by at least 20%. Frequent baby breathing has understandable physiological and psychological reasons. When children are worried, worried, in a state of stress, fear, or in a nervous situation, they very often react to stress by increasing their breathing movements.
Such tachypnea does not require correction or treatment and usually goes away on its own as the delicate children’s nervous system strengthens. If the stress is very strong, then parents can consult a neurologist and child psychologist.
Pathological tachypnea is always quite a serious diagnosis:
- acute or chronic infectious respiratory disease;
- bronchial asthma;
- high temperature, heat;
- traumatic brain injuries, cerebral edema and cerebral hemorrhages;
- pneumonia;
- tuberculosis;
- tumors in some parts of the respiratory system;
- mechanical injuries of the chest (rib fractures, cracks and displacements);
- pathologies of the cardiovascular system, congenital heart defects.
With shortness of breath, shallow, shallow breathing in a child is observed only during periods of increased physical activity, at moments when the child is tired and trying to catch his breath. Shortness of breath is temporary and transient. Tachypnea is permanent. If the excess of the normal breathing rate does not disappear in the child even during sleep, this is certainly a reason to call a doctor and examine the baby for a possible disease.
Respiratory rate of a healthy newborn
A newborn may have an infection if he or she is breathing very quickly or slowly. A newborn should take 40-60 breaths per minute. A study of 953 healthy full-term newborns found that newborn breathing rates varied significantly. The mean respiratory rate was 46 breaths per minute 2 hours after birth. However, about 5% of children took more than 65 breaths per minute. This suggests that a fast breathing rhythm may be normal and healthy in some cases.
The breathing rate slows down as the child gets older. The typical breathing rate for a child aged 1 to 3 years is 24-40 breaths per minute. Rapid breathing, or tachypnea
, occurs more often than slow frequency -
bradypnea
. Tachypnea usually means that the child is not getting enough oxygen and is compensating by breathing quickly. Many conditions can cause breathing difficulties in newborns. Some common risk factors for respiratory distress include:
- premature birth
- birth of a child by caesarean section
- ingestion of meconium during labor
- low levels of amniotic fluid, which is a condition called oligohydramniosis
- infection in the membranes or amniotic fluid, called chorioamnionitis
- gestational diabetes in mother
What to do?
If you detect an increase in respiratory rate in newborns, it is best to call a doctor. If the baby has other symptoms - runny nose, cough, fever, breathing or exiting has become difficult, the best solution is to call an ambulance. For an older child, you can try to help yourself. A prerequisite is the absence of any additional painful signs.
To stop an attack of tachypnea, just take a paper bag, cut a small hole in it and invite the child to breathe through the bag in a playful way. This will help restore gas exchange in the cells, and breathing will stabilize.
Inhalation and exhalation should be done only through the bag; outside air should not be inhaled.
A sudden increase in breathing for no apparent reason (excitement, stress, fear) is always an alarming symptom that parents should not ignore. It is important to quickly pull yourself together, calm the baby, breathe through the bag, make sure that the child’s skin has a normal color, has not changed, has not turned pale or has turned blue. Treatment always involves treatment of the underlying disease that caused rapid breathing.
What can't you do?
Parents should not try to give medications to a child with rapid breathing. No pills or drops at this moment can affect an individual symptom of a probable hidden disease. But it is quite possible to worsen the baby’s condition with these drugs without permission. You should not try to give inhalation to a child with breathing problems. They are not able to help, but the burn of the respiratory tract that a baby can get from inhaling steam is a very real threat.
It is important for parents to learn to distinguish tachypnea from ordinary shortness of breath.
To learn what the child’s breathing rate is considered correct, see the following video.
Normal respiratory rate (RR) in children by age
The work of a baby’s heart is a very important criterion for the functioning of his body. Pulse rate, respiratory rate and blood pressure are the main medical indicators of cardiac function.
Doctors advise that when a child is ill, together with the temperature, count the child’s pulse and breathing rate once a day. In order to correctly measure the pulse and breathing, it is very important that the child is in a calm state.
You can read what the standards should be and what deviations are possible in this article.
Pulse measurement in children
Keep the child calm.
The best place to detect the pulse in a child under one year old is the brachial artery. You need to look for it on the inside of the upper limb in the middle between the elbow and shoulder. Apply gentle pressure with two fingers towards the bone while supporting the outer part of the hand with your thumb.
In children older than one year, the pulse can be looked for in the carotid artery. Feel for the Adam's apple (the protuberance in the middle of the larynx) with two fingers. Move your fingers away from the Adam's apple towards the depression between it and the neck muscles. Press on your neck to feel your pulse
Most often, the pulse is measured at the radial artery. Using the tips of 2-3-4 fingers of your right hand, feel the pulse on the radial artery in the wrist area.
The pulse count in children is carried out strictly in one minute, since it is arrhythmic in children.
Result assessment: newborn - 120 - 140 per minute; infancy - 110 - 120 per minute; older age - 70 - 100 per minute.
What are heart rate and respiratory rate?
Heart rate is a count of the number of times the heart beats per minute. Respiratory rate is the number of inhalations and exhalations per minute.
These indicators make it possible to determine how deep and rhythmic breathing is, as well as the ability to analyze the performance of the chest. Heartbeat characteristics differ during different periods of growth.
Important! A biomarker such as respiratory rate has been known since ancient times. The doctors of the ancient world noticed that this indicator changes in a sick person.
Today, respiratory rate (respiratory rate) does not lose its relevance in the diagnosis of a wide variety of childhood and adult diseases. One series of “inhalation-exhalation” is considered to be one movement. The number of such movements over a specific period of time is assessed - usually 1 minute.
It should be noted that NPV in children is not at all similar to that in adults. Children, due to their anatomical features, breathe somewhat differently - their breathing is shallow, superficial, and the frequency of inhalation and exhalation is much higher.
Important! The oxygen needs of a growing child's body are extremely high, and the volume of the lungs and the size of the chest are small. This is why the baby needs intense breathing.
However, there are certain norms for different ages. And if the breathing rate exceeds these norms, it may indicate that the child has oxygen starvation (hypoxia). Rapid breathing accompanies a wide variety of pathologies in children.
Scientists have conducted a number of studies and found that the younger the person, the higher the pulsation. Doctors came up with approximate requirements for numbers by age.
When a baby is born, the heartbeat can reach 140 beats per minute, and as it gets closer to one year it becomes lower - up to 110 beats.
During adolescence, the pulse is already in the range of the normal pulse rate of an adult. The normal respiratory rate is the main criterion in assessing the state of circulatory performance.
In infancy, these indicators are normal if the ratio of respiratory rate to heart rate is 1:2. The respiratory-pulse coefficient is approximate and can have various types of fluctuations. In children over 1 year of age, the ratio of respiratory rate to heart rate is 1:3.
Respiratory rate in children
Breathing is the most natural process of all physiological processes. We are so accustomed to it that we don’t even notice it, especially since no one thinks about whether this process is happening normally for us or our child.
It should be emphasized that breathing is a very important phenomenon, both for the growth of the baby and for his health and development in general.
You need to pay attention to how often your child breathes, because it is this indicator that determines how often and seriously the child will get sick.
It should be noted that even the development of a child’s speech depends on whether he breathes normally. Therefore, parents should be very careful about how correctly their child is breathing. Unfortunately, it often happens that the normal breathing process of a child bothers parents, but improper breathing may not bother them at all.
- Blood pressure in children
- Pulse in children
Child's breathing rate
The normal respiratory rate in children, like other physiological processes, depends on their age. The normal breathing rate in newborns, first hours after birth, is considered to be in the range from 20 to 80 breaths per minute, the average frequency of this indicator is approximately 30-40 breaths per minute.
At the age of 2 to 3 years, the norm is 20-30 breaths per minute, but for a teenager, the norm is 12-20 breaths per minute. The normal situation is that the baby breathes completely from the diaphragm, and very often their breathing is shallow and not constant. It should be emphasized that in premature babies, breathing may be periodic (i.e.
periodically decreases and increases), which is then replaced by a pause in breathing for 10-15 seconds.
In babies born at term, periodic breathing is quite rare, but this is also considered a normal indicator. But it should be borne in mind that apnea (pause in breathing) that lasts more than 20 seconds, or apnea after which cyanosis or pallor occurs, is always considered as a defect (apnea of infants).
What is the norm?
Breathing is considered normal when the child first takes a deep breath and then exhales smoothly.
The baby's breathing rate should be measured to see how well his lungs are ventilated.
If a child’s breathing is more deviated from the norm, this means that the breathing is shallow. Shallow breathing creates favorable conditions for pathogens.
Table of normal respiratory rate in children
The correct breathing rate in children is the following per minute:
- for newborn babies – 40-60 breaths;
- for children aged 1-2 months – 35-48 breaths;
- for children under 3 years of age – 28-35 breaths;
- for children aged 4-6 years – 24-26 breaths;
- for children aged 7-10 years – 31-23 breaths;
- for children aged 10-12 years – 18-20 breaths;
- for children aged 13-15 years – 16-18 breaths.
Respiratory rate in newborns
New parents should know that the breathing of newborn babies is different from the breathing of older children. The reason for this is believed to be that the baby’s nasal passages are still poorly developed, as is, in general, the entire respiratory system.
Babies breathe abruptly, sometimes speeding up the pace of breathing, sometimes slowing it down. Often, one deep breath is replaced by several short ones.
This type of breathing is considered normal for infants, especially for premature babies, and is called Cheyne-Stokes breathing.
Such breathing flows into a more uniform one within one month, and by the end of the baby’s first year of life, breathing becomes calm and even. It is necessary to take into account that the nasal passages of infants are very narrow, so they can be filled with lint and dust, which can cause wheezing, wheezing and sniffling. In order to avoid this, the baby should systematically clean his nose.
You can measure the baby's breathing rate only when he is calm. In infants, frequency can be measured visually by watching the movement of the baby's chest.
Doctors measure this indicator with a special device - a phonendoscope. But you can do without it; to do this, you need to place your hand on the baby’s chest and count the breaths.
In order for the child not to interfere with the counting and not to get scared, you need to distract him with a toy.
Causes of increased breathing
Often, rapid breathing is accompanied by other symptoms of respiratory system disorders. For example, your baby may make gurgling, wheezing, or whistling sounds when breathing.
If your child exhibits such signs, then you should definitely consult a doctor, as this may be the cause of various infections.
An increase in breathing rate may be a symptom of pneumonia, which occurs asymptomatically in babies.
If, in addition, the child experiences shortness of breath, this may be a sign of both cardiac pathology and pulmonary pathology; this condition of the child requires immediate hospitalization. Also, rapid breathing can be a symptom of bronchitis and false croup. With false croup, the baby's breathing is frequent and noisy; in addition, the child is tormented by severe coughing attacks.
Reduced breathing rates are much less common in children than in adults. Decreased breathing may be a symptom of meningitis, a serious brain injury. Rapid breathing is normal during physical activity and outdoor games. Also, rapid breathing is a manifestation of violent emotions when the child is overexcited or interested in something.
Source: https://nedeli-beremennosti.com/chastota-dyxaniya-u-detej/
Table by age for children: norms
Pulse studies have shown that in newborns it is 140 beats per minute. The pulse rate in children in the first 12 months of life decreases to 110-130, and over 12 years of age the pulse rate reaches approximately the adult norm.
The norm of respiratory rate in children is important for assessing the condition of the respiratory tract, heart, circulatory system and health in general. The ratio of respiratory rate to heart rate is the respiratory-pulse coefficient in infants 1:2.5, in children under 12 months - 1:3, older - 1:4. The following table presents the norms of respiratory rate and heart rate in children by age.
NPV in children: norm, table and doctors’ recommendations
We think you don't often pay attention to how many breaths you take per minute. For healthy adults, such a value as respiratory rate is not very relevant.
What cannot be said about newborns: it is not for nothing that the respiratory rate in children is one of the most important indicators of well-being and development, allowing one to monitor and respond in a timely manner to various diseases and pathologies.
How and why should NPV be calculated?
Let's start with the fact that during any therapeutic examination, doctors check the newborn's respiratory rate along with the pulse: that's how important this value is in assessing the condition of babies.
The fact is that the baby will not be able to tell you that something is wrong with him, and sometimes a deviation in the breathing rate is the only sign of a developing disease.
But before you draw any conclusions about the health of your baby, you need to learn how to collect this information.
When calculating the respiratory rate of an infant, it is important to observe several points so that the data is reliable, but otherwise the procedure is elementary and will take literally a minute.
- Count your breathing rate only at rest. If the child is actively spinning, crawling or walking, breathing will be rapid. If the baby is nervous, overexcited or crying, the breathing rate will also increase. It will be easiest to determine the value in a dream, when nothing will distort the information.
- Count the number of breaths per minute. If you count the breaths over 30 seconds and multiply by 2, the information may be incorrect due to the arrhythmic breathing characteristic of newborns.
- When counting, you do not need to use any additional devices. In infants, the movements of the chest and diaphragm are clearly visible, so you can calculate the respiratory rate in a newborn without even touching him.
Having received the data, you may panic: there are unrealistic numbers, arrhythmia, and incomprehensible delays in breathing! Should I sound the alarm and go to the doctor or is the situation developing within normal limits?
Ideal layout
Of course, there is a certain established norm of breathing rate for different ages, which we will present below in the form of a table, and it is from this information that you can build on when assessing the baby’s condition.
So, if a newborn up to one year old has a respiratory rate of 50 breaths per minute, then there is no need to worry, but if we are talking about a two-year-old child at rest, then this is no longer normal.
But proper breathing includes not only a quantitative, but also a qualitative factor, which is usually not included in the table.
It is believed that optimal breathing is mixed: this is when a child can switch from chest to abdominal type and back. This way the lungs are ventilated as much as possible, which prevents the establishment of an environment favorable for the proliferation of harmful microorganisms.
It’s just worth considering that for newborns, breathing with the diaphragm is more typical than breathing with the chest, so panic in case of insufficient manifestation of the latter will be unjustified.
In addition, we are accustomed to the fact that breathing correctly means taking a deep, smooth breath and exhaling measuredly, and, of course, this arrangement is ideal for babies. But due to the peculiarities of the body of newborns, such a picture is quite rare, and deviations from the norm “deep inhalation - smooth exhalation” make parents worry and worry. But is it worth it?
Advice
The nasal passages in newborns are narrow and easily clogged, and babies cannot breathe through their mouths, which leads to shortness of breath, sniffling and wheezing, especially during sleep. This is why it is so important to clean babies’ noses from dust and dirt and to prevent severe swelling of the mucous membrane.
Is periodic breathing dangerous?
Cheyne-Stokes syndrome, or periodic breathing, is typical for premature babies, although it is also common in those born at term.
With this respiratory process, the baby breathes rarely and shallowly, then moves on to more frequent and deep breaths, after reaching peak inhalation, he again breathes less frequently and shallowly, and then there is a short delay.
From the outside it may seem that this is some kind of attack, and the child urgently needs help, but if you move away from the concept of the “adult” norm, it turns out that there is nothing terrible here. Usually this type of breathing levels out somewhat by the month, and by the year there is no trace left of it. But how many nerves periodic breathing takes away from unprepared parents!
Advice
Even when there is no health problem, rapid breathing in a newborn means that the baby is breathing shallowly, which means that the lungs are not ventilated thoroughly enough.
Risks of rapid, infrequent breathing and pauses
If frequent, abdominal and even arrhythmic breathing in children is the norm, then how can you understand that a problem has arisen and not miss the moment?
Rapid breathing (tachypnea) will be considered critical if it deviates from the age norm by 20%.
This condition may indicate a number of diseases: from colds, flu, false croup and bronchitis to serious infections, as well as pulmonary and cardiac pathologies.
In most cases, the rapid breathing that you should be concerned about will be accompanied by shortness of breath or wheezing from your baby.
Slow breathing (bradypnea) is unusual for infants. If you count fewer breaths than normal, this may be a sign of developing meningitis, but most likely your baby is growing and the baby's breathing rate is decreasing because of this. Again, we can talk about a slowdown only if the indicators are 20% below the age norm.
Holding your breath (apnea) is an absolutely normal phenomenon, especially when it comes to periodic breathing, but it should not exceed 10-15 seconds.
If the baby does not breathe for more than 20 seconds and the attack is accompanied by pallor, an arrhythmic pulse and blue discoloration of the fingertips and lips, then you should immediately call an ambulance: this situation is far from normal, and the child needs an examination.
Advice If a child was born premature, it is better to immediately learn how to act in case of apnea, so as not to fall into a stupor when he stops breathing for a while. If you do not place your baby on his back during sleep and know basic techniques for provoking inhalation, such as a simple massage or sprinkling with cold water, such moments will not cause much trouble for either the baby or you.
How many breaths your baby takes per minute should definitely be monitored on a regular basis. Of course, only you will have to decide whether you can handle it yourself or call a doctor, but we hope the information in the article will help you make the right decision.
Source: https://TheRebenok.ru/zdorove/chdd-u-detej-norma-tablica.html
Features of the child's respiratory system
The first thing an expectant mother has been waiting for for so long is the baby’s first cry. It is with this sound that his first breath occurs. By the time of birth, the organs that ensure the child’s breathing are not yet fully developed, and only with the growth of the body itself do they mature (both functionally and morphologically).
The nasal passages (which are the upper respiratory tract) in newborns have their own characteristics: • They are quite narrow. • Relatively short. • Their inner surface is delicate, with a huge number of vessels (blood, lymphatic).
Lung tissue in young children also has its own characteristics. Unlike adults, their lung tissue is poorly developed, and the lungs themselves have a small volume with a huge number of blood vessels.
Rules for counting breathing rate
Measuring respiratory rate does not require any special skills or equipment. All you need is a stopwatch (or a watch with a second hand) and following simple rules.
The person should be calm and in a comfortable position. If we are talking about children, especially young children, then it is better to count respiratory movements during sleep. If this is not possible, the subject should be distracted from the manipulation as much as possible. To do this, just grab your wrist (where the pulse is usually detected) and meanwhile count your breathing rate. It should be noted that the pulse in children under one year of age (about 130-125 beats per minute) should not cause concern - this is the norm.
Considering that breathing has its own rhythmic cycle, it is necessary to observe the duration of its counting. Be sure to measure your respiratory rate over the course of a full minute, rather than multiplying the result obtained in just 15 seconds by four. It is recommended to carry out three counts and calculate the average.
Normal respiratory rate in children: table. Respiratory rate
One of the actions carried out during examination by a pediatrician is counting respiratory movements. This seemingly simple indicator carries important information about the state of health in general and about the functioning of the respiratory organs and cardiovascular system in particular.
How to correctly calculate the respiratory rate (RR) per minute? This is not particularly difficult. But certain difficulties arise with the interpretation of the data.
This is more true for young parents, because, having received a result from a child that is several times higher than their own, they panic.
Therefore, in this article we propose to figure out what the normal respiratory rate is for children. The table will help us with this.
The first thing an expectant mother has been waiting for for so long is the baby’s first cry. It is with this sound that his first breath occurs. By the time of birth, the organs that ensure the child’s breathing are not yet fully developed, and only with the growth of the body itself do they mature (both functionally and morphologically).
The nasal passages (which are the upper respiratory tract) in newborns have their own characteristics:• They are quite narrow.• Relatively short.
• Their inner surface is delicate, with a huge number of vessels (blood, lymphatic).
Therefore, even with minor catarrhal symptoms, the child’s nasal mucosa quickly swells, the already small lumen decreases, and as a result, breathing becomes difficult and shortness of breath develops: small children cannot yet breathe through their mouths. The younger the child, the more dangerous the consequences can be, and the faster it is necessary to eliminate the pathological condition.
Lung tissue in young children also has its own characteristics. Unlike adults, their lung tissue is poorly developed, and the lungs themselves have a small volume with a huge number of blood vessels.
Rules for counting breathing rate
Measuring respiratory rate does not require any special skills or equipment. All you need is a stopwatch (or a watch with a second hand) and following simple rules.
The person should be calm and in a comfortable position. If we are talking about children, especially young children, then it is better to count respiratory movements during sleep.
If this is not possible, the subject should be distracted from the manipulation as much as possible. To do this, just grab your wrist (where the pulse is usually detected) and meanwhile count your breathing rate.
It should be noted that the pulse in children under one year of age (about 130-125 beats per minute) should not cause concern - this is the norm.
In infants, it is strongly recommended to count the respiratory rate during sleep, since crying can significantly affect the result and give deliberately false numbers. By placing your hand on the anterior abdominal wall (or just visually), you can easily carry out this study.
Considering that breathing has its own rhythmic cycle, it is necessary to observe the duration of its counting. Be sure to measure your respiratory rate over the course of a full minute, rather than multiplying the result obtained in just 15 seconds by four. It is recommended to carry out three counts and calculate the average.
Normal respiratory rate in children
The table shows the normal respiratory rate. Data are presented for children of different age groups.
As we can see from the table, the frequency of respiratory movements per minute is higher, the younger the child. Gradually, as they grow older, their number decreases, and by puberty, when the child turns 14-15 years old, the respiratory rate becomes equal to that of a healthy adult. No differences by gender are observed.
Types of breathing
There are three main types of breathing in both adults and children: chest, abdominal and mixed.
The breast type is more typical for females. With it, inhalation/exhalation is ensured to a greater extent due to movements of the chest. The disadvantage of this type of breathing movement is poor ventilation of the lower parts of the lung tissue.
Whereas in the abdominal type, when the diaphragm is more involved (and the anterior abdominal wall visually moves during breathing), the upper sections of the lungs experience a lack of ventilation. This type of breathing movement is more common for men.
But with a mixed type of breathing, a uniform (identical) expansion of the chest occurs with an increase in the volume of its cavity in all four directions (upper-lower, lateral). This is the most correct type of breathing, which ensures optimal ventilation of the entire lung tissue.
Normally, the respiratory rate in a healthy adult is 16-21 per minute, in newborns - up to 60 per minute. Above, the norm of respiratory rate in children is given in more detail (table with age norms).
Rapid breathing
The first sign of damage to the respiratory system, especially in infectious diseases, is increased breathing. In this case, there will definitely be other signs of a cold (cough, runny nose, wheezing, etc.). Quite often, when body temperature rises, the respiratory rate increases and the pulse quickens in children.
Holding your breath during sleep
Quite often, young children (especially infants) experience short-term pauses in breathing during sleep. This is a physiological feature.
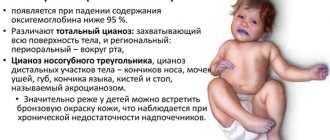
But if you notice that such episodes become more frequent, their duration becomes longer, or other symptoms arise, such as blue lips or nasolabial triangle, loss of consciousness, you must immediately call an ambulance to prevent irreversible consequences.
Conclusion
The respiratory organs of young children have a number of features that contribute to their frequent damage and rapid decompensation of the condition.
This is primarily due to their immaturity at the time of birth, certain anatomical and physiological characteristics, incomplete differentiation of the structures of the central nervous system and their direct influence on the respiratory center and respiratory organs.
The younger the child, the less lung capacity he has, and therefore he will need to make a greater number of respiratory movements (inhalation/exhalation) to provide the body with the necessary volume of oxygen.
Summing up
It should be remembered that respiratory arrhythmia is quite common in children in the first months of life. Most often, this is not a pathological condition, but only indicates age-related characteristics.
So, now you know what the normal respiratory rate is for children. The table of averages should be taken into account, but small deviations should not panic. And be sure to consult your doctor before jumping to conclusions!
Source: https://2qm.ru/dom-i-semja/deti/norma-chdd-y-detei-tablica-chastota-dyhatelnyh-dvijenii.html
Types of breathing
There are three main types of breathing in both adults and children: chest, abdominal and mixed.
The breast type is more typical for females. With it, inhalation/exhalation is ensured to a greater extent due to movements of the chest. The disadvantage of this type of breathing movement is poor ventilation of the lower parts of the lung tissue. Whereas in the abdominal type, when the diaphragm is more involved (and the anterior abdominal wall visually moves during breathing), the upper sections of the lungs experience a lack of ventilation. This type of breathing movement is more common for men.
But with a mixed type of breathing, a uniform (identical) expansion of the chest occurs with an increase in the volume of its cavity in all four directions (upper-lower, lateral). This is the most correct type of breathing, which ensures optimal ventilation of the entire lung tissue.
Normally, the respiratory rate in a healthy adult is 16-21 per minute, in newborns - up to 60 per minute. Above, the norm of respiratory rate in children is given in more detail (table with age norms).
Ideal layout
Of course, there is a certain established norm of breathing rate for different ages, which we will present below in the form of a table, and it is from this information that you can build on when assessing the baby’s condition. So, if a newborn up to one year old has a respiratory rate of 50 breaths per minute, then there is no need to worry, but if we are talking about a two-year-old child at rest, then this is no longer normal.
But proper breathing includes not only a quantitative, but also a qualitative factor, which is usually not included in the table. It is believed that optimal breathing is mixed: this is when a child can switch from chest to abdominal type and back. This way the lungs are ventilated as much as possible, which prevents the establishment of an environment favorable for the proliferation of harmful microorganisms. It’s just worth considering that for newborns, breathing with the diaphragm is more typical than breathing with the chest, so panic in case of insufficient manifestation of the latter will be unjustified.
In addition, we are accustomed to the fact that breathing correctly means taking a deep, smooth breath and exhaling measuredly, and, of course, this arrangement is ideal for babies. But due to the peculiarities of the body of newborns, such a picture is quite rare, and deviations from the norm “deep inhalation - smooth exhalation” make parents worry and worry. But is it worth it?
Advice
The nasal passages in newborns are narrow and easily clogged, and babies cannot breathe through their mouths, which leads to shortness of breath, sniffling and wheezing, especially during sleep. This is why it is so important to clean babies’ noses from dust and dirt and to prevent severe swelling of the mucous membrane.
Holding your breath during sleep
Quite often, young children (especially infants) experience short-term pauses in breathing during sleep. This is a physiological feature. But if you notice that such episodes become more frequent, their duration becomes longer, or other symptoms occur, such as blue lips or nasolabial triangle, loss of consciousness, you must immediately call an ambulance to prevent irreversible consequences.
The respiratory organs of young children have a number of features that contribute to their frequent damage and rapid decompensation of the condition. This is primarily due to their immaturity at the time of birth, certain anatomical and physiological characteristics, incomplete differentiation of the structures of the central nervous system and their direct influence on the respiratory center and respiratory organs. The younger the child, the less lung capacity he has, and therefore he will need to make a greater number of respiratory movements (inhalation/exhalation) to provide the body with the necessary volume of oxygen.
Respiratory rate in children: norm by age
In infancy and childhood, almost all body systems differ markedly from those of an adult.
When a baby is born, his lungs and chest have different proportions than those of an adult. The baby's chest grows faster than the lungs, and only in an adult does it acquire the size at which fully expanded lungs fit into a relaxed chest.
In children, the lungs do not fully expand even when the chest is fully raised during inhalation. In order for the child’s body to receive the required amount of oxygen, the body is forced to breathe at an increased frequency. Therefore, the respiratory rate in newborns is the highest among all age groups.
Another feature of infants’ breathing: about 70% of them, up to the age of 3-6 weeks, breathe only through the nose. And only 30% immediately breathe through their nose and mouth. This doesn't mean that children who breathe through their noses can't breathe through their mouths, just that they don't do it in their normal, calm state.
In the first months of a baby’s life, his nasal passages are anatomically narrow, and the mucous surfaces of the respiratory tract are supplied with blood to a much greater extent than in adults. This property of the mucous membrane is very useful for the baby, because it allows cold and dry air to enter the lungs already warmed and moistened, cleared of dust and harmful microbes.
But besides the advantages, breathing through the nose also has its disadvantages. The narrowness of the nasal passages due to inflammation, swelling of the mucous membranes or nasal congestion does not allow the child to take a full breath.
Any speck that gets into the nose can cause sneezing and mucus accumulation. The baby's breathing becomes difficult, becomes shallow and frequent, and his sleep and feeding are disrupted.
The baby becomes restless and begins to scream, thereby ensuring the required amount of air enters the lungs.
The functioning of a newborn's pulmonary system largely depends on the functioning of its diaphragm. This muscle separates the chest cavity from the abdominal cavity and, due to its contractions, ensures the respiratory movements of the lungs. Therefore, problems with the gastrointestinal tract, as well as tight swaddling of the baby, which limits the mobility of his diaphragm, affect the frequency of his respiratory movements.
At an older age, children already breathe largely due to the intercostal muscles and abdominal muscles.
Sometimes infants have a type of breathing in which regular inhalations and exhalations alternate with irregular ones. This is the norm for this age.
A baby's unusual breathing in itself should not be a cause for concern. Shallow, jerky breaths with wheezing or an unstable rhythm are a fairly common phenomenon, although they are some deviation.
We recommend Causes and methods of treating cough in a child
2 Normal frequency
Knowing the child's breathing standards, parents can pay closer attention to his health. The normal respiratory rate in children gradually decreases by age as the baby grows.
Below is a table showing what the normal breathing rate is for children of different ages.
| Child's age | Normal frequency of inhalation-exhalation cycles per minute |
| Newborns | 30-50 |
| From birth to 5 months | 25-40 |
| From 6 to 12 months | 20-30 |
| From 1 year to 5 years | 20-30 |
| From 6 to 12 years | 12-30 |
| From 12 to 18 years old | 12-16 |
For comparison, in adults the breathing rate is approximately 12-20 breaths per minute.
If your child's breathing rate falls within the range noted above, there is no reason to worry. If breathing becomes faster, this may be an indication of problems and is a reason to immediately consult a doctor.
Possible causes of problems with the respiratory system:
- 1. Infection;
- 2. Respiratory distress syndrome;
- 3. Transient tachypnea of newborns;
- 4. Other problems (pneumonia, lung malformation, etc.).
We recommend Classification and symptoms of respiratory failure
3 Dependence on body temperature
Research shows that the heart rate of babies 2 months and older increases by approximately 10 beats per minute for every degree Celsius increase in body temperature. In children under 2 months of age, this does not occur due to insufficient activation of nervous system regulators to adequately respond to elevated temperature.
Increased temperature stimulates the respiratory muscles and causes increased work of the pulmonary system. Frequent inhalations and exhalations allow heat to be more actively removed through pulmonary gas exchange.
The breathing rate of children under 12 months of age increases by 7-11 breaths per minute for every degree Celsius increase in body temperature. For children under 2 years of age, this figure decreases and is already 5-7 breaths per minute per 1 degree Celsius.
It should be noted that body temperature has a moderate, albeit significant effect on respiratory status, regardless of age group. The application of the obtained data in clinical practice is limited, since the nature of the relationship between respiratory rate and body temperature is not linear.
We recommend Spirography as a method for studying pulmonary function
Heart rate norms in children
Normal heart rate values in childhood differ significantly from those in adults. The heartbeat in children has its own characteristics and varies at different ages.
The younger the child, the higher the heart rate. Gradually, with age, the value of this indicator decreases
The average heart rate values for children by age are presented in the table below.
| Age | Average normal heart rate in beats per minute |
| first month of life | 110-170 |
| from 1 month to a year | 102-162 |
| from one to two years | 94-154 |
| from 2 to 4 years | 90-140 |
| from 4 to 6 years | 86-126 |
| from 6 to 8 years | 78-118 |
| from 8 to 10 years | 68-108 |
| from 10 to 12 years | 60-100 |
| from 12 to 15 years | 55-95 |
If your pulse is too fast
We recommend reading: When does the fetal heartbeat begin?
If the heart rate exceeds the norm, the reasons may be as follows:
- hot weather;
- exercise stress;
- stressful situation.
In these cases, the pulse may increase three times, but this is not a pathology. A child may have a rapid heartbeat even at rest. Main reasons:
- prostration;
- overwork;
- heart diseases;
- endocrine diseases;
- respiratory diseases;
- anemia;
- infectious lesions.
If the pulse is too low
If you feel normal and no pathologies are found, a rare pulse indicates good training.
Low heart rate values are typical for children involved in sports, especially those that require the development of endurance.
But bradycardia can be associated with pathologies and be accompanied by unpleasant symptoms. If your baby complains of dizziness, weakness, loss of strength, and has high or low blood pressure, you need to show him to a doctor as soon as possible.
Source: https://zdorovo.live/krov/chastota-dyhaniya-u-detej-norma-po-vozrastam.html