- Causes of the defect
- What does a cleft palate look like?
- Difficulties for children with cleft palate
- What does correction mean?
- Method of eliminating cleft palate
- Operation stages
- Rehabilitation period
- Reviews about the operation
The cleft palate is a congenital deformity in the form of a cleft (non-closure) of the tissues of the palate. In this regard, the child's oral and nasal cavities communicate. In addition to a noticeable cosmetic defect, children with such a malformation of the maxillofacial region have problems with breathing, nutrition, speech, etc. Correcting this defect is a complex surgical process that involves more than one reconstructive intervention, but this will allow the child to develop correctly and facilitate his socialization.
Who treats children with cleft palate and lip?
Considering that such deformation affects areas that are under the jurisdiction of various specialists, most often it is necessary to involve a whole team of doctors to combat these defects. And, as a rule, such a team includes the following doctors:
- Plastic surgeon. A specialist who performs lip or palate surgery;
- Otolaryngologist. A doctor whose specialization is the fight against diseases affecting hearing, who is able to select the most effective method for treating problems of this kind;
- Maxillofacial surgeon. This doctor is responsible for carrying out manipulations to move part of the upper jaw, designed to achieve normal functioning, as well as eliminate cosmetic defects and cleft gums;
- Orthodontist. A doctor who specializes in straightening and moving teeth;
- Dentist. A doctor who specializes in dental and oral health care;
- Prostodont. A doctor who produces artificial teeth and special dental devices that help restore the appearance and normal functioning of the speech apparatus. If necessary, these devices help make eating easier;
- Speech pathology specialist. A doctor who studies pathologies related to eating and speech;
- Speech therapist. A specialist who knows methods to improve speech quality;
- Audiologist. This physician's expertise includes the study of communication disorders associated with hearing loss or impairment.
- Attending doctor. A specialist who studies the general condition of the child;
- Social worker or psychologist. Provides planned assistance to the family and gives advice on overcoming any problems associated with adaptation;
- Specialist in the field of genetics. Both parents and adult patients are interested in the advice of this doctor, from which they can find out how high the likelihood of having children with similar defects is.
Treatment of a child involves drawing up a special program, involving the joint participation of each specialist and taking into account the individual needs of the patient. Most often, already in infancy, specialists prescribe and carry out the first measures to get rid of detected deformities. However, this process is quite lengthy and most often ends when the patient reaches early adulthood.
Cleft lip: surgical correction of the defect
Usually the first question that parents of a child with a similar pathology ask the doctor is the age at which surgery can be performed to correct this defect. The answer depends on the severity of the damage to the upper palate. If the pathology affects only the soft palate, surgery can be performed at the age of 12–24 months.
Correction of cleft palate is possible no earlier than 3–4 years. Otherwise, there is a high risk of impaired development of the facial skeleton. For bilateral lesions, two surgeries are necessary. They are carried out at intervals of 6 months.
Veloplasty is considered the most gentle surgical intervention, but it is only suitable for correcting cleft palate. To correct the defect, own areas of the mucous membrane from the nasopharynx and oral cavity are used. As a rule, the operation is well tolerated by young patients, and after a few days the child can return to their usual lifestyle and diet.
Correction of the hard palate (uranoplasty) is a much more complex surgical procedure. However, modern technologies make it possible not only to correct the defect, but also to completely restore the functions of the hard and soft palate. To exclude a rejection reaction, skin flaps are used from the lateral surface of the cheeks and upper palate.
Naturally, such an operation cannot be done without the use of anesthesia. The best option is inhaled drugs; their administration begins after tracheal intubation and connection of the device. In some cases, intravenous medications are used for general anesthesia; the most common today is Propofol. During the operation, the patient is under constant supervision of an anesthesiologist, who monitors the pulse, respiratory rhythm and other vital signs.
The rehabilitation period can last up to one and a half months. On the first day after surgery, swelling and bleeding may occur at the suture site. To prevent airway obstruction, the child should be kept in a lateral position.
Important
To prevent infection, broad-spectrum antibacterial drugs are prescribed, and analgesics are required.
Once a cleft lip has been operated on, the return to a normal diet should be gradual. In the first few days, the patient is given intravenous special nutritional solutions. To ensure proper formation of the upper palate, a custom-made plate is installed after the operation. It is left in place for 1 – 1.5 months and removed during meals and classes to develop correct speech.
After surgery, the child needs to consult an orthodontist and dentist. Classes with a speech therapist are also required. The specialist will write out a plan for independent study for parents. The simplest exercises are blowing bubbles in a glass of water through a cocktail straw, or inflating balloons.
Also recommended:
- stick out your tongue as much as possible, trying to reach your chin;
- puff out your cheeks, releasing air alternately through the right and left corners of your lips;
- pronounce consonants with your mouth tightly closed;
- various lip exercises;
- game of “horse” (clicking the tongue);
- drinking water in small portions;
- gargling.
But cleft lip cannot be corrected in some patients. Contraindications to surgical intervention are severe concomitant defects of intrauterine development, pathologies of the cardiovascular and respiratory systems, and intolerance to anesthesia drugs.
In some cases, surgery can lead to improper formation and development of the tissues of the soft palate. If such disorders interfere with speech and digestive function, repeated surgery is recommended. Other complications usually occur when the doctor's advice is not followed. Sutures may become separated and become infected, and rough scars may form.
In the vast majority of patients, the operation is well tolerated. Sometimes traces of the defect remain on the face, in which case it is necessary to contact a plastic surgeon who will eliminate them without a trace. After a complex of surgical measures, cleft lip and cleft palate do not affect the child’s future life.
https://youtube.com/watch?v=iBKTRH7InNw
Diagnostics
Adequate diagnosis of cleft palate or lip is not very difficult. As already noted, the diagnosis of “cleft palate” and “cleft lip” becomes obvious on ultrasound in the 1st – 2nd trimesters of pregnancy.
An external examination of the newborn allows an accurate diagnosis to be made. However, for a more complete examination, it is sometimes necessary to resort to certain research methods:
radiography of the maxillofacial area to assess bone defects;
audiometry or hearing test. It is assessed either with the help of special equipment or by careful observation of the baby (his reaction to auditory stimuli)
Necessary for large clefts with a high risk of hearing loss up to deafness;
examination of the sense of smell (the child’s facial expressions and behavioral reactions to certain categories of strong odors are assessed);
A general blood test is mandatory for all newborn babies, however, in babies with a defect, special attention should be paid to it. An increase in the level of white blood cells - leukocytes, specific inflammatory proteins (C-reactive protein, ceruloplasmin) and an acceleration of the erythrocyte sedimentation rate (ESR) indicate the addition of an infection, which can be quite difficult in weakened children.
Intrauterine facial development
This is a rather complex process of formation and fusion of tissues and bones, which begins by the end of the first month of intrauterine development.
At the fourth week of pregnancy, the embryo can already distinguish five processes (tubercles) that limit the oral cavity: the frontal, paired maxillary and paired mandibular. They participate in the intrauterine formation of the face and gradually grow, merging with each other.
The nasal process of the frontal tubercle and the processes of the maxillary tubercles take part in the formation of the upper jaw and upper lip. As a result of the convergence and growth of the tubercles, clefts are formed between the processes.
Fetal clefts:
- median - develops at the convergence of the mandibular or maxillary tubercles;
- transverse - formed by the mandibular and maxillary tubercles;
- oblique and lateral - formed at the convergence of the processes of the maxillary tuberosities and the nasal process of the frontal tuberosity.
Already by the beginning of the eighth week of embryonic development, the fusion of facial clefts is completed with the formation of the main lines of the face. If for some reason complete fusion of the processes of the embryonic tubercles does not occur, then such clefts persist in the future in the form of congenital anomalies. For example, if the transverse cleft does not heal, a pathologically large mouth is formed (macrostomia), and if the lateral cleft persists, a cleft lip is formed.
Something went wrong…
Around the 4th-6th week of fetal formation, the paired median nasal protrusions fuse. They fuse to form the incisive bone, the philtrum of the upper lip, and the tip of the nose. The lateral elements of the upper lip originate from the paired maxillary processes. If the tissues do not heal for some reason, a cleft lip appears. It usually originates at the junction between the central and lateral parts of the upper lip on both sides.
The secondary palate begins to develop around the eighth week of pregnancy, after development of the primary palate has completed. The paired palatal folds are initially separated by the developing tongue. As the mandible grows, the tongue moves forward and the palatine folds move downward and assume a more horizontal position. If something goes wrong, the paired palatal folds cannot move down and medially - a cleft appears in the palate.
The secondary palate usually develops before the 12th week. Therefore, diagnosis of congenital facial clefts using ultrasound (ultrasound) is optimally carried out at 11–12 weeks of pregnancy (this is when the formation of the baby’s face ends).
A cleft lip can be diagnosed by a specialist if the fetus's face is positioned correctly. Diagnosing the palate using ultrasound is more difficult. However, an experienced doctor can record an atypical movement of the fetal tongue in the lateral projection. In some cases, specialists cannot identify this defect until childbirth if the child covers his face with his arm or leg.
D.Yu.Komelyagin : “We will soon open a consultation center for pregnant women in the St. Vladimir Children's City Clinical Hospital on the basis of the department for newborns, which, among other things, will see maxillofacial surgeons. And if, say, during an ultrasound examination the baby was diagnosed with a facial malformation, the mother will be able to come straight to us for a consultation. We will calm her down, tell her how this or that defect can be cured, explain what awaits her, and most importantly, we will prove that this is not a reason to abandon the child; with the right treatment tactics, you can live a full life even with facial defects.”
Tutankhamun had a cleft palate. This conclusion was reached two years ago by a group of scientists who examined his mummy. The research was led by the Secretary General of the Supreme Council of Antiquities of the Arab Republic of Egypt, Zahi Hawass. Tutankhamun is not the only person whose facial clefts did not prevent him from achieving success and fame.
The face of famous artist Joaquin Phoenix also seems to bear traces of a facial cleft. However, the artist’s biographers claim that the scar on his lip is not a mark from the operation, but a congenital “mark.” However, whether it is a hidden cleft or a cleft at all is not so important. More importantly, the scar from it did not prevent Joaquin from making a brilliant film career.
The same scar on his lip (also visually similar to an operated cleft) did not prevent Cheech Marin from becoming a popular American film artist, Denis Dorokhov from becoming a famous KVN player in Russia, and Denis Lebedev from becoming a world boxing champion.
How is a cleft palate or lip treated?
To completely remove the deformity, specialists have to perform one or two surgical operations. The final decision is made after studying the condition of the defect. The first time surgery is performed when the child reaches three months of age.
to eliminate such a defect
After the first operation, there is not only an improvement in the functioning of the palate, but also a decrease in the risk that fluid will enter the middle ear. Other positive effects include the creation of conditions for the proper formation of teeth and facial bones.
Treatment of pathology
The main treatment method for these pathologies is surgery.
Surgery for cleft lip is called cheiloplasty. Most often, it is performed closer to 6 months of age, however, in some cases, the baby may require urgent surgery (during the first month of life).
This is usually associated with extensive defects.
Depending on the affected tissues, perform:
- Isolated cheiloplasty – stitching of the skin, subcutaneous tissue, muscle layer and mucous membrane of the lips;
- Rhinocheiloplasty (Latin “rino” – nose) – additional correction of nasal cartilage;
- Rhinognathocheiloplasty – formation of the muscular frame of the mouth area.
Unfortunately, surgical intervention alone cannot be done. In the first 3 years of life, the baby will have to lie on the operating table 3-4 times.
The successes in the treatment of cheiloschisis are enormous. In most cases, the child is left with only slight lip asymmetry and a barely noticeable scar. And already in adulthood, a person will be able to contact a cosmetologist who will help eliminate minor defects.
Treatment for cleft palate is called uranoplasty. The timing of this operation differs from cheiloplasty - the optimal age is 3-4 years. Earlier surgery may harm the growth of the upper jaw.
For large through clefts, surgery is postponed until 5-6 years. However, by the beginning of the school period, most children receive all the necessary assistance and are no different from their peers.
Surgery is only one stage of treatment. The child will definitely need the help of a speech therapist who will form correct speech. And problems with bite and improper growth of teeth will be solved by an orthodontist by installing a braces system.
Technique for eliminating cleft palate
With the help of radical uranoplasty, it is possible to restore the child’s normal nutrition and improve the quality of his speech. Among such operations, the most common is plastic surgery using the Limberg method. If there is also a cleft lip, the upper lip is corrected (cheiloplasty).
The operation to correct the defect involves general anesthesia, which includes the following steps:
- induction anesthesia;
- tracheal intubation;
- anesthesia support;
- withdrawal from anesthesia.
The best time for such intervention is between 3 and 6 years of age. Up to 5 years of age, operations are performed on patients with non-through cleft palates, from 5 to 6 years – on patients with through (unilateral and bilateral) ones. If uranoplasty is performed earlier, there is a risk of delayed development of the upper jaw.
Before surgery, children are recommended to wear a “floating” obturator (a prosthesis to close the defect) to allow normal nutrition, breathing and speech development. This prosthesis is removed two weeks before surgery.
Postoperative period and recovery
In the postoperative period, the child continues to receive antibiotics, and analgesics are also prescribed. It will be possible to leave the hospital no earlier than the end of the first week after the intervention, and only if there are no adverse consequences and the person operated on is in good health.
Caring for a child who has undergone plastic surgery on the palate and lip must be careful and careful. Throughout the first week, the wound is covered with a napkin with an antiseptic, which prevents the proliferation of microflora and suppuration of the suture. The wipes can be removed after the stitches are removed. After each meal, the mouth should be rinsed or irrigated with an antiseptic spray. Tampons or special silicone tubes can be installed in the nose to prevent tissue stretching and deformation.
In the second week after the intervention, under the supervision of a surgeon, a gentle finger massage of the palatal area is performed to improve regenerative processes and blood supply.
It is important that the baby himself does not damage the operation site and sutures with his movements, so his arms can be fixed for some time with a bandage or splints. If the surgeon has planned a two-stage treatment, then at least a year will have to pass between plastic surgery
During this entire period, it is imperative to use an obturator, which separates the oral cavity from the nasal cavity and prevents the reflux of food into the latter.
If the surgeon has planned a two-stage treatment, then at least a year will have to pass between plastic surgeries. During this entire period, it is imperative to use an obturator, which separates the oral cavity from the nasal cavity and prevents the reflux of food into the latter.
Some parents, for personal reasons, wanting to choose the best surgeon for their child and ensure maximum comfort during treatment, are ready to undergo a paid correction. Regardless of the financial side of the issue, the result will depend on the skill of the surgeon and the complexity of the defect.
Plastic surgeries for the described anomalies can be quite complex and time-consuming, but the result in the vast majority of cases serves as a reward for both the children and their parents for the patience and difficulties they overcame in the first months and years of life. With the skill and accuracy of the surgeon, it is possible to achieve a result when there are practically no traces left from the intervention, and those around you do not even suspect a serious defect, which once could have been a shock for the whole family.
before/after surgery
An example of successful treatment is not only photos of the defect before and after surgery, which can be found on the Internet, but also the faces of famous actors, show business stars, and athletes. These results can be reassuring, somewhat reassure parents and give strength to fight pathology and support the child.
How to feed a newborn baby with a cleft palate?
Rules for breastfeeding a child with a cleft palate defectbreastfeedingRules for feeding a newborn with a cleft palate are:
- It is necessary to keep the child in a semi-upright position;
- the baby's head should be above the level of the nipple;
- when breastfeeding or bottle-feeding, the mother should direct the nipple or pacifier to the part of the palate that is not damaged;
- The woman should support the breast with her palm, and hold the baby’s cheeks and chin with her thumb and forefinger;
- the baby's position must be changed frequently so that he can burp air;
- if the baby does not get enough to eat, breast milk should be expressed and the baby should be fed with a bottle;
- when breastfeeding, you should ensure that the breast does not cover the baby’s nose and does not interfere with his breathing;
- After eating, the oral cavity should be treated with a disinfectant.
Feeding equipment
Cleft palate - what to do?
Surgery is considered the only way to make the baby’s life easier and ensure normal development and future. Other options do not eliminate the cleft palate; treatment with conservative methods is not effective. Depending on the extent of the lesion, urano-, velo- and cheiloplasty are performed. If cleft palate syndrome in children is corrected in a timely manner and the rehabilitation period is carried out correctly, by the age of 10 it will be almost unnoticeable that the baby was born with an anomaly. On the eve of the operation, preparation is required:
- organizing the baby's nutrition;
- prevention of acute respiratory viral infections and acute respiratory infections;
- dental, speech therapy assistance;
- prevention of ear diseases;
- psychotherapy for parents.
How to feed a child with a cleft palate?
Eating with cheiloschisis can result in food and drinks getting into the nose, especially if complete or through cleavage is diagnosed. Before the cleft palate is surgically corrected, special nutritional arrangements will be needed. For infants, special breast shields or nipple covers are used to cover the cleft palate.
Children born with severe cleft palate must be fed through a feeding tube. A thin and soft tube is inserted through the nose and one end is inserted into the stomach. The probe is installed by a doctor and changed every 3 months. Parents of the baby are taught how to use such a device correctly. Additionally, an obturator is applied - a plate that covers the damage.
Cleft palate in children - surgery
Surgical intervention is carried out at the discretion of the doctor and within the time frame established by him. The diagnosis of cleft palate in a child requires several procedures, from 2 to 15, in accordance with the severity of the genetic pathology. There is no general consensus at what age it is advisable to perform the manipulation. Some doctors prefer to start therapy at 3-6 months, while other specialists focus on later dates. There are 3 types of surgical interventions that can be used to treat cleft palate; the operation is performed using the following techniques:
- uranoplasty – work on defects of the hard palate;
- cheiloplasty – suturing of the upper lip;
- Veloplasty – elimination of deformations of the soft palate.
Features of the pathology of cleft lip
This is called cheiloschisis or congenital cleft of the upper lip. It is a non-fused upper lip. The jaws and facial organs are formed before the 8th week of pregnancy, so it is at this time that signs of a cleft lip in children begin to appear. Such vices are not always independent. 20% of patients have a severe congenital syndrome.
The presence of a cleft lip in a child gives grounds for a number of surgical interventions. Specialists from the fields of pediatrics, dentistry, surgery and speech therapy take part in the treatment of this pathology.
Causes of pathology
The formation of a cleft lip in all newborns occurs during the first trimester of pregnancy at the genetic level. Under the influence of various factors, a mutation of the TBX22 gene occurs with the formation of a cleft lip. The causes of this pathology are the following factors.
- Severe toxicosis in the first trimester of pregnancy.
- Abuse of alcoholic beverages, antibiotics, as well as smoking and drugs.
- Excessive stress during pregnancy.
- The influence of aggressive chemicals and radiation.
- Late pregnancy after 35 years of age.
- In some cases, the cause of a cleft lip in newborns may be abdominal injuries received by the mother during pregnancy.
- It is believed that the pathology is inherited. Therefore, if one child in the family already had this anomaly, then at the planning stage of the next pregnancy it is advisable to conduct a medical genetic examination.
Consequences of the development of pathology
Children with cleft lips and their parents face serious problems until surgery is performed to correct the defect. This will be a difficult test for any person. The development of a cleft lip is usually noted away from the midline of the upper lip. There are also more severe cases when the defect is present on both sides. It is associated with various functional disorders.
- Violation of the processes of sucking and swallowing. For particularly complex clefts, feeding through a special nasal tube is practiced.
- With the appearance of teeth, people are faced with malocclusion. These may be additional or missing teeth, or an incorrect angle of their growth. In turn, malocclusion leads to poor quality of chewing food and problems with the digestive tract.
- Parents may also be concerned about the appearance of speech dysfunctions. The resulting speech defect is characterized by difficulty pronouncing consonant sounds, nasal sound, and unclearness.
To eliminate a cleft lip, treatment is primarily surgical. But, as a rule, other specialists whom we have already mentioned earlier also participate in the process.
Treatment methods
After surgery, the cleft lip is completely eliminated - all impaired functions are restored, and the child’s appearance improves. There are three types of plastic surgery aimed at eliminating congenital pathology.
- The most well-known concept is cheiloplasty. This is the simplest surgery for cleft lip, which does not require correction of other tissues. It is performed for moderately severe defects not accompanied by a cleft palate.
- Rhinocheiloplasty is a more complex operation. During its implementation, in addition to the lips, the muscular frame of the facial region is also affected. It helps not only improve the child’s appearance, but also restore essential functions such as breathing and swallowing.
- The most difficult type of operation is rhinocheilognatoplasty. It includes both types of operations described and additionally correction of the pulmonary canals. It is prescribed in the most severe cases.
Now you know why pathologies associated with cleft palate and lip develop, and what treatment methods exist. If you want to learn about them in more detail and hear the opinions of experts, we offer you a very useful and informative video.
What is a cleft lip?
This is a defect of the upper lip (a bilateral form of the disease is extremely rare), as a result of which it bifurcates right up to the nose. This pathology does not pose any danger to the lives of children. But you can’t leave it, because a cleft lip prevents children from eating normally and forming speech. In addition, a child with a similar pathology may have an incorrectly formed dental system. And most importantly, children with such a deviation necessarily require special teeth care products. That is why doctors advise not to delay in taking appropriate measures when such pathologies are identified. After all, this unpleasant cosmetic defect can always be leveled out with the help of modern plastic surgery and forgotten about it forever.
“Why did this happen to me?!”
Dmitry Yuryevich Komelyagin
- Dmitry Yuryevich, there is a myth that facial clefts are a problem for children from disadvantaged families.
- No! We have many families with prosperous, beautiful parents whose children are faced with such a problem. The risk factor, rather, will be the fact that the parent himself was a carrier of this pathology in childhood. We have such families. Let's say we once operated on a girl with a cleft lip, she got married and gave birth to a child with exactly the same pathology, they came to us again. We had families in which the second and even third child was born with a similar pathology. And we successfully operated on all of them.
— How many years have you been operating?
— The department was founded 26 years ago. We have been operating for 26 years now. Facial clefts are a multifactorial problem, and it is still difficult to identify specific causes. It is known that the cause may be intrauterine fetal hypoxia. What caused this hypoxia? Anything. Stress? Maybe. Mother's infection? Taking medications? Yes, it's possible. But no one can tell you what exactly.
Today, the most substantiated theory is considered to be that the cause of facial clefts is a combination of hereditary factors and adverse environmental influences.
Mutation of several genes entails increased sensitivity to bacteria in the environment. In this case, the cleft may be caused by factors such as medications, x-rays, infections, and even stress and noise. As a result of their exposure, the fetus experiences a lack of oxygen during the few hours it takes for the face to form, and then the fused tissues suffer.
Why is a child born with a cleft lip?
At the end of the first month of pregnancy, the baby's mouth forms from two separate halves that grow next to each other.
Around the sixth to eighth week, they fuse together to form the upper jaw. Next, the seam goes back and forth to seal the lips with the tongue.
By the tenth week of pregnancy, the mouth is fully formed and the nose has acquired its familiar structure and location.
A cleft lip is a congenital defect in which a child's upper lip is completely formed and has a hole. A cleft palate is a similar congenital anomaly in which the palate of the unborn child is not fully formed, but has a hole.
Some children with a cleft lip have only a small indentation in their upper lip. Others have a full open opening that extends through the upper jaw to the bottom of the nose. The abnormality may appear on one or both sides of the child's mouth.
This birth defect is called an oral cleft, or cleft lip. In children, the causes of its occurrence are still unknown.
Defects and the conditions for their development vary in severity and degree with variations:
- Cleft lip (lip defect).
- Cleft palate (defect of the roof of the mouth).
- Cleft lip and palate (both defects).
- Microform of a cleft (crack or scar).
- Unilateral cleft (one side of the lip and palate).
- Bilateral cleft (both sides of the lip and palate).
Cleft lip and cleft palate: causes
The causes of cleft lip, cleft palate and other facial abnormalities are not well understood, but they are directly related to changes in the child's genes.
It is believed that 25% of cases are due to heredity, up to 15% are chromosomal abnormalities and 60% are external causes of the birth of children with cleft lip. The tendency to become deformed may be inherited from one or both parents.
The potential for developing the disease increases when it occurs among close members of the same family.
Recent studies have identified smoking and drinking alcohol during pregnancy as risk factors for the development of cleft lip and palate, as well as other birth defects.
In addition, having diabetes significantly increases the risk of having a baby with a cleft lip or without a palate. Drug use and intoxication of the body can also cause these birth defects. Cleft lip and palate can occur along with other congenital anomalies.
This can lead to a number of difficulties in everyday life. Babies are often born with a cleft lip or palate if they have a family member with the condition or a history of other birth defects.
Genetics and heredity
To this day, the true causes of cleft palate and lip development are unknown, but doctors believe that the defects arise due to genetic and environmental factors. Genetics may play a role in the development of a condition such as cleft lip.
The causes may combine several factors. If one or both parents had this deviation, this significantly increases the manifestation of the anomaly in the child.
The lifestyle you lead during pregnancy may also increase your baby's chance of developing an abnormality.
So, why does a disease such as cleft lip develop? Photos, causes and treatment methods will help you learn better about this pathology.
- Exposure to phenytoin or drug use during pregnancy increases the risk of developing the abnormality by 10 times or more.
- Smoking during pregnancy increases the chance of developing a defect by 2 times.
- Use of alcohol, anti-seizure medications, or retinolic acid has been linked to birth defects that include cleft lip and palate.
- During pregnancy, a deficiency of vitamins, and especially folic acid, can also cause the development of craniofacial anomalies.
There are many factors that cause cleft lip in children. The reasons and photos of this disease make it clear the seriousness of the situation. Cleft palate can develop as an isolated birth defect or as part of a larger genetic syndrome that can lead to more severe defects.
Environment
During pregnancy, what a mother takes, eats and drinks is critical to the development of her unborn child. Vitamins and nutrients enter the growing body through the mother's blood.
But between a woman and her unborn baby there is a strong protective shell called the placenta. It does not allow some toxic substances to pass through and reliably protects the baby in the womb.
While the placenta is really good at filtering out toxins, other dangerous chemicals can pass through this barrier and enter the fetal blood stream.
Causes of the defect and development factors
Many experts argue that the cause of the defect is not one factor, but several. There are certain factors that increase the risk of a fetus developing cleft palate :
- the woman has had abortions in the past;
- smoking and drinking alcohol even in early pregnancy;
- heredity - if one of the parents in the family had children with a cleft palate, then the risk of gene transfer is 7-10%;
- excess body weight;
- increased body temperature (overheating in the sun, in a bathhouse, working in a hot room);
- presence of vibration at work of the expectant mother;
- mother's age is over 35 years.
Causes of the defect:
- poor nutrition;
- mechanical damage to the fetus (blows to the abdomen, operations in the lower abdomen);
- psychological disorders, stress;
- poisoning with chemicals (hair dye, pesticides, arsenic, etc.);
- exacerbation of infectious and viral diseases (measles, herpes, rubella, malaria and others);
- taking certain medications;
- attempt to provoke a miscarriage;
- uterine fibroids;
- exposure to radiation from x-rays or ultrasound;
- insufficient activity of germ cells of one or both parents.
Despite the large number of possible causes for the development of the defect, in 20-30% of cases the source remains unknown .
According to statistics, about 20% of cases are provoked by chemical poisoning, 8-10% by stress and psychological disorders, 5-7% by mechanical damage to the fetus, 4-6% by exacerbation of diseases, 2-3% by physical impact on the baby.
What is the causative agent of vesiculopustulosis in infants? Find out the answer right now.
Diagnostics
It is not difficult to make a diagnosis after the birth of a child; all that is required is a visual examination of the newborn.
In this case, the child will also need consultations with an ENT doctor.
This is necessary in order to determine whether there are any other problems (for example, cleft palate, abnormalities in the structure of the nasal cavity).
Signs of a cleft lip can be recognized in the prenatal period. This can be done using an ultrasound as early as 14 weeks of pregnancy. However, in order to finally confirm the diagnosis, you will need to gather a medical consultation.
This is very important, since this pathology is the basis for termination of pregnancy. Of course, the decision in this case is made only by the woman herself, but at the legislative level, abortions at this stage in the presence of pathology are permitted (in normal cases, artificial termination of pregnancy is prohibited after 12 weeks)
Of course, the decision in this case is made only by the woman herself, but at the legislative level, abortions at this stage in the presence of pathology are permitted (in normal cases, artificial termination of pregnancy is prohibited after 12 weeks).
Anatomy of the upper palate
left and right side
Anatomy of the hard palate
on each side, the zones of the hard palate are:
- The palatal suture zone runs along the midline of the palate. In this zone, all tissues (mucous, submucosal) are firmly fused with the periosteum. In this place, the mucosal epithelium forms palatal ridges, which are very pronounced in children.
- The marginal zone corresponds to the junction of the palate and the gum of the upper jaw.
- The glandular zone occupies the posterior part of the hard palate. In this part, between the periosteum and the mucous membrane, there are numerous small glands.
- The fatty zone occupies the anterior part of the hard palate. There is a well-developed fat layer here.
Anatomy of the soft palate
due to which it got its name uvula tonsils. The following muscles are involved in the formation of the soft palate:
- uvula muscle;
- velopharyngeal muscle;
- palatoglossus muscle;
- muscle that lifts the velum palatine;
- muscle that strains the velum palatine.
both muscles and mucous membrane
Types of defects ↑
In most cases, newborns have a cleft on the upper lip and very rarely you can find a defect on the lower lip.
There are several types:
1. One-sided splitting:
- Incomplete - part of the lip tissue remains untouched in the upper part.
- Complete is a complete cleft of the upper lip.
- Hidden - only the muscles of the lip are split, and the skin and mucous membrane are intact.
2. Bilateral splitting:
- Symmetrical - incomplete or complete cleft on both sides.
- Asymmetrical - incomplete or hidden on one side, complete on the other (and other options).
A split on one side is a depression on the upper lip. In this case, the middle nasal and right maxillary processes do not have fusion. The defect can have different configurations, for example, in one case it affects only the soft tissues of the lip, and in another it can also affect the bones of the upper jaw.
Cleft palate disease: symptoms of various forms of pathology
According to the clinical picture, all forms of pathology have similar features.
Cleft palate disease is accompanied by the following disorders:
- Digestive disorders. A newborn is not able to eat normally; with severe damage to the upper palate, it is almost impossible to establish breastfeeding. Doctors recommend using special nipples, but even with their use, the child gains weight more slowly and does not receive enough necessary vitamins and nutrients.
- Breathing disorders. Such disorders begin immediately after birth. Breathing movements become shallow and superficial, so the child often suffers from hypoxia, anemia and other disorders associated with lack of oxygen.
- Delayed speech development. The upper palate is involved in the pronunciation of many sounds, so its splitting is accompanied by severe speech therapy disorders.
- Predisposition to inflammation of the middle and inner ear. A change in the passage of air through the nasopharynx and the entry of food into the nasal cavity leads to the development of an inflammatory process and a decrease in the activity of local immunity. Chronic pathology can cause permanent hearing loss.
A cleft of the soft palate can be hidden, when the gap is covered with an epithelial membrane, and open, when the pathology covers all the tissues of this structure. In addition, such a disease is classified into complete, in which the cleft reaches the border of the hard palate and is accompanied by its insufficient development, and incomplete, affecting only the muscle tissue of the soft palate. Cleft palate disease is usually accompanied by severe breathing and swallowing disorders and speech disorders.
Unilateral or bilateral cleft of the soft and part of the hard palate can be hidden under the epithelial membrane, however, the pathologies accompanying such a congenital defect manifest themselves from the first days of the child’s life.
A unilateral cleft of the hard upper palate is accompanied by a violation of the tightness between the oral and nasal cavities, which leads to a disorder of respiratory and digestive function. In addition, the child cannot pronounce all sounds in the pronunciation of which the upper palate is involved. Often a similar disease, cleft palate, is combined with cleft lip. Bilateral cleft palate is always accompanied by a cleft lip, is severe and requires surgical intervention as early as possible.
Cleft palate disease is diagnosed towards the end of the second trimester of pregnancy. However, ultrasound examination is not always informative. The baby may cover his face with his hands, or his position in the uterus does not allow the doctor to conduct a detailed examination. Therefore, if doubt arises, a repeat ultrasound using Doppler is recommended.
Early diagnosis will allow parents to prepare for appropriate care for the newborn and consult with specialists. From the moment of birth, a child with a cleft palate requires close supervision by pediatricians and monitoring of respiratory function. However, the first surgical intervention (in some cases several will be needed) is carried out no earlier than one year of age.
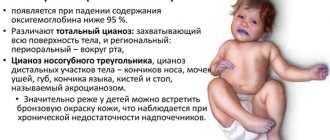
What does a cleft palate look like in a child?
A cleft palate is an unpleasant sight, especially if the disease is combined with a cleft lip. The cleft palate got its name due to the similarity of the pathological structure of the baby’s upper jaw with the oral cavity of a dog. The severity of the signs of cheiloschisis and the appearance of sick children depend on the form of the defect and its severity. A typical deformation is shown in the photo.
Cleft palate - classification
There are 4 main types of this disease. They are differentiated by the degree of clefting of the upper palate. Cleft palate in a newborn child can be diagnosed in the following forms:
- Latent cheiloschisis.
The integrity of the mucous membrane of the soft palate is preserved; only the muscles are split. - Cleft palate. In the soft palate, both membranes and muscles are damaged, the hard palate is partially affected.
- Complete splitting.
The pathology affects both the soft and hard palate up to the incisive foramen. - Through cheiloschisis.
The most severe cleft palate is in children; photographs show that not only the palate is cleft, but also the gums and upper lip. May be present on one or both sides.
How does a cleft palate appear together with a cleft lip?
External manifestations of the cleft palate and cleft lip are the hole located in the lower wall of the nasal cavity the part of the jaw on which teeth grow Physiological manifestations of the anomaly Manifestations of the cleft palate and cleft lip include:
- Anomalies of facial development. If left untreated, cleft palate and lip can cause blemishes to form on the face.
- Speech impairment. Violation of the integrity of the soft palate causes problems with the normal formation of sounds. Air currents passing from the mouth to the nose provoke unpleasant sounds heard during a conversation. A cleft lip also creates acoustic interference. Common manifestations of these congenital anomalies are speech defects such as dyslalia, rhinolalia, and nasality.
- Inflammatory diseases. A cleft palate allows fluids a child drinks to enter the sinuses and eustachian tubes. This anomaly also leads to respiratory problems. All this leads to the fact that such patients often suffer from colds, otitis media, and sinusitis.
- Developmental disorders of the dentition. Patients with cleft lip experience problems such as missing teeth, extra teeth, and incorrect angles of tooth growth. Malocclusion is also common.
- Dental problems. Children with these pathologies often suffer from caries and other oral diseases.
- Digestive disorders. From the moment of birth, children with cleft palate and lip experience difficulties during feeding, since the vacuum required for proper sucking is not created in the oral cavity. In adulthood, problems with digesting food arise due to malocclusion.
- Hearing problems. In patients with a palate defect, fluid often stagnates in the middle ear, which causes the development of ear infections. As a result of frequent illnesses, patients' hearing deteriorates.
- Retarded physical development. Difficulties with feeding prevent patients with such defects from receiving sufficient amounts of nutrients. This is the reason why such patients have difficulty gaining weight and are developmentally delayed.
Psychological manifestations of facial development defects
What does the pathology of the upper lip and palate look like?
Cleft lip is a physiological abnormality affecting the upper lip. The cleft looks like a gap in the skin. Cheiloschisis can spread to the nasal area and affect the gums and jaw. Pathology of the soft and hard palate manifests itself in the form of a hole in its tissues. According to statistics, out of a thousand people born, only one has this developmental defect.
It is not uncommon for a child to be born with a cleft lip and cleft palate at the same time. The presented photographs will allow us to assess the seriousness of the situation and fully convey the psychological state of parents faced with the problem of the absence of the upper palate in their children. At the moment, geneticists have identified three genes that, as a result of mutation, can lead to deviations in the maxillofacial area. Scientists do not stop there, since the defective gene in patients with anomalies in the development of the palate and lips is detected only in 5% of cases.