ARVI is a common problem in the daily life of every person, especially during the off-season, when one feels unwell, has a runny nose and sore throat, which is often accompanied by an increase in temperature. Some women do not attach much importance to such symptoms, and sometimes even suffer from colds on their feet, continuing their active lifestyle and work activities. But when breastfeeding, treatment of ARVI becomes the number one problem, because in no case can you infect the child. In this case, the young mother has many questions about feeding the baby or medications allowed during lactation.
Should I stop breastfeeding?
Many mothers wonder whether it is necessary to stop breastfeeding if they have a cold. It should be noted that babies under the age of six months very rarely get ARVI. This is explained by the fact that in the womb they received special antibodies that protect them from the virus. They also continue to enter the child's body during feeding. Therefore, if a mother refuses to breastfeed, this will deprive her baby of natural protection.
How does the disease progress?
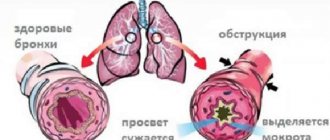
The increased load on the respiratory system of a nursing mother causes high vulnerability to viral infection, which is transmitted by airborne droplets. As for ARVI itself, this disease does not pose a particular danger to a nursing woman, but significant harm can be caused to the baby’s body. The course of ARVI during breastfeeding, the treatment of which we will examine below, is usually divided into three periods, which include:
- The virus enters the mother's body. From the moment it enters the body, as well as until the first signs appear, on average, about three days pass. Further symptoms of the disease include chills, fever, sore throat, and runny nose.
- Immune response. As a rule, this period begins three days after the onset of characteristic symptoms of the disease. The immune response is characterized by increased production of interferons, which are responsible for eliminating the virus.
- Full recovery. The time frame for recovery will vary for each person. On average, this takes about 10 days from the time the first symptoms of ARVI appeared. If there is no improvement in well-being, we can safely talk about the emergence of complications of this viral infection.
What to do to avoid infecting a child?
The fact that a cold is not transmitted through breast milk does not mean that the baby has no chance of acquiring the infection. If there is constant contact between a sick mother and baby, a protective mask alone will not help, and in order not to infect the newborn, you should follow certain rules:
- The most effective method is isolation of the sick person, but if it is the mother, then in the first months of the baby’s life this is excluded,
- The sleep of the child and the infected mother should definitely be separate; it is better to put the baby to sleep in a separate room or at least in his own crib,
- everything that the baby touches must be carefully treated and washed: sterilize nipples and bottles, feed from separate dishes, wash clothes separately from adult clothes, wash toys periodically,
- in the absence of a child in the room, be sure to ventilate the room, monitor the temperature and humidity,
- if the mother is ill, do not stop walking with the baby outside, dad or grandmother can walk with the child even in cloudy weather, moist air is also good for the baby,
- periodically wipe dust in places where the baby spends the most time,
- there is no need to wrap up the child, you need to dress the baby like yourself, so that it is comfortable, but not too hot,
- if possible, avoid staying in public places during a wave of diseases and do not invite guests to your home if someone is sick in the house,
- use a gauze bandage not only for the sick, but also for all family members,
- quartzing or spreading aromatic oils, for example, conifers, as well as the smell of onions and garlic, will not be superfluous, this will help kill microbes,
- It is worth monitoring the hygienic toilet of the baby and parents, washing hands and face more often,
- It is better to replace ordinary drinking water during illness with fruit drinks or drinks with beneficial additives, rose hips, honey, lemon or ginger,
- During an epidemic, it is recommended to use drugs to boost immunity, so before going for a walk, mom can use Oxolinic ointment,
- You need to constantly monitor the child’s health, and if a runny nose appears, take appropriate measures immediately.
Treatment of ARVI during breastfeeding
The treatment technique for this disease in women during breastfeeding should be strictly selected by the treating specialist on an individual basis. The reason to consult a doctor is a persistent increase in temperature that does not subside for more than 3 days, as well as a general deterioration of the condition. After this, the specialist will tell you how to treat ARVI while breastfeeding. However, therapy must be comprehensive. To achieve a speedy recovery, it will not be enough to use only prescribed medications for ARVI while breastfeeding. A woman should adhere to other expert advice, which is as follows:
- Bed rest. Constant rest is considered a prerequisite for successful treatment of a viral disease, regardless of the severity of the disease. If you do not comply with bed rest during ARVI in a mother who is breastfeeding, this will only worsen the general condition and will also significantly prolong the period of the disease.
- Drinking regimen. The intake of fluid will stimulate the process of cleansing the sick body of the virus. In addition, drinking regime will help reduce body temperature, as well as improve overall well-being. In addition to medications for ARVI during breastfeeding, which the doctor will prescribe, you should also drink warm tea, berry juice, and fruit compote, which contain vitamin C.
- Diet. Please note that eating food for this disease should not be forced under any circumstances. If a woman develops ARVI while breastfeeding, then she needs to eat food when she wants it. At the initial stage of the disease, it is recommended to eat light foods, for example, chicken broth.
Is it possible to breastfeed during ARVI?
Leading pediatricians have long given an answer to this question; there is no need to stop feeding a child if he has a cold. This is due to the fact that the viral disease is transmitted only by airborne droplets, that is, only some particles of the virus enter the baby through breast milk, which are not capable of infecting the baby; rather, on the contrary, they will strengthen the baby’s immunity even better. But you shouldn’t kiss the baby, sneeze or cough in his presence during this period, as this increases the risk of microbes getting from the mother’s mucous membrane to the baby. Even in cases where the baby does get sick or catches the infection first, there is no need to stop breastfeeding; mother’s milk itself is a cure for all diseases for the baby; you can’t think of a better treatment.
Antiviral agent
How to treat ARVI while breastfeeding with antiviral drugs? Many people are faced with a difficult choice, as there are currently a huge number of antiviral drugs available on pharmacy shelves. During breastfeeding, it is strictly forbidden to use the following drugs: Arbidol, Remantadine, Ribavirin.
The use of medications such as Aflubin and Anaferon will not give the desired result, because these medicines are considered homeopathic and have increased allergic activity.
The best option for the treatment of ARVI in nursing mothers will be those products that are made on the basis of recombinant human interferon alpha. This group of substances usually includes the drugs “Grippferon”, “Viferon”. The frequency and dosage of taking these medications should be determined only by the attending physician.
Taking medications approved for breastfeeding
Pharmacies offer a wide selection of medications whose action is aimed at combating the influenza pathogen. But another question arises: how to treat flu while breastfeeding. You will need to consult a doctor who will draw up a treatment regimen and select safe medications.
During the flu, a nursing mother is prescribed the following medications:
- Immunomodulatory and antiviral medications. This group of drugs affects the cause and actively fights the pathogen. Immunomodulatory drugs increase the body's defenses.
- Antipyretic. Breastfeeding women are allowed to take paracetamol-based medications.
- For nasal congestion, use saline solutions.
It is important to correctly draw up a treatment regimen that will be completely safe for the child.
Antiviral and immunostimulating drugs
The list of medications that breastfeeding women are allowed to take is small. Let's consider how a nursing mother can be treated for the flu:
Grippferon. The drug is available in the form of a spray, ointment and drops. The active component is interferon alpha-2b. The medication fights the acute inflammatory process, has a positive effect on the immune system, and reduces the risk of progression of complications. Actively used to prevent influenza. Side effects manifest themselves in the form of allergic reactions. Do not take in case of hypersensitivity to the active components.
Viferon. The product is produced in the form of gel, ointment and suppositories. The active component is also interferon alpha-2b. The frequency of use and duration of drug therapy is determined only by the doctor. Do not use if you are hypersensitive to the components in the composition.
Aflubin
If the question arises of how to treat flu during lactation, then pay due attention to Aflubin. Produced in the form of tablets and drops
This is a homeopathic remedy with a completely natural composition. Characterized by immunomodulatory properties. Thanks to its unique composition, the product lowers temperature and eliminates inflammation from the mucous membranes. The drug actively fights intoxication of the body due to illness.
These are the drugs that are allowed for breastfeeding and are as safe as possible for both mother and baby.
Antipyretics and painkillers
As soon as the first symptoms of the disease appear, women are faced with the question of what a nursing mother can do if she has the flu. Doctors recommend taking children's forms of drugs as antipyretics.
Let's look at how to treat the flu in a nursing mother:
- Nurofen for children. The drug is based on ibuprofen. Helps quickly normalize temperature, eliminates the acute inflammatory process, and is also characterized by an analgesic effect. But this medication is prohibited for use for stomach ulcers, heart, liver and kidney diseases.
- Panadol for children. The active ingredient is paracetamol. The medication fights fever and eliminates pain. Do not use in case of hypersensitivity to the components in the composition, as well as in case of pathological changes in the kidneys and liver.
- Efferalgan. It also contains paracetamol, which quickly brings down the temperature. The frequency of administration and dosage is determined by the doctor.
- Antigrippin. The drug is produced in the form of effervescent tablets and powder to obtain a solution. It is characterized by a complex effect, as it lowers temperature, relieves pain from the flu, reduces nasal congestion, and fights lacrimation. Do not take if you have a stomach ulcer.
These are the most effective and approved drugs for hepatitis B.
Medicines for nasal congestion
Women are also interested in the question of what to do if a nursing mother gets sick with the flu, how to cope with congestion. Doctors prescribe medications based on a solution of natural sea salt.
The best permitted means are:
- Aqua Maris. The product is available in the form of a spray for irrigation of the nasal passages. Sea water from the Adriatic Sea is used. The drug greatly facilitates breathing when you have a runny nose, fights swelling of the mucous membrane, and removes viruses and bacteria. Do not use for nosebleeds.
- Aqualor. Another good drug that contains sea water from the Atlantic Ocean. Available in the form of a spray for irrigation of the nasal cavity. Side effects occur extremely rarely in the form of a local allergic reaction.
Even before using such safe products, you should consult your doctor.
Treatment of a runny nose
To relieve swelling of the mucous membrane in the nasal passages, as well as normalize nasal breathing, special sprays and drops are used, which contain a vasoconstrictor component. The use of such drops is considered harmless for both mother and baby. Among the most common means of this action are:
- "Naphthyzin", "Sanorin". The active ingredient in these medications is the substance naphazoline, which has a very short duration of action.
- "Galazolin", "Otrivin", "Xymelin". The main active ingredient in these drugs is xylometazoline, which has an average duration of decongestant effect.
- "Noxprey", "Nazol". The active ingredient in these medications is oxymetazoline. This substance has a long period of active action and is also capable of maintaining it for about 12 hours.
Antipyretic medications
The use of antipyretics is advisable if the body temperature rises above 38 degrees. The lowest rates are considered an adequate response of the human body to a cold virus, and therefore do not require any medical intervention. While breastfeeding, women are advised to use antipyretic drugs that contain paracetamol or ibuprofen.
The use of these drugs is considered safe if the conditions for use are met. Combined-action medications, for example, Teraflu or Flukold, contain additional components that can have a very unpredictable effect on the child’s body.
The use of antipyretic medications is permitted only in the dosage recommended by the attending physician.
Homeopathy
Nowadays, many mothers are still afraid to treat diseases with medications, trusting more in folk remedies or homeopathic ones. There is no official confirmation of the positive effects of such drugs; many doctors talk about a woman’s psychological mood and her beliefs, which are much stronger in homeopathy than any medicine.
Negative factors include possible allergies to components of homeopathic remedies and the use of alcohol for herbal tinctures,
which impairs milk production in a nursing woman. As a rule, the composition of the drugs is completely natural, and the most recognizable is Anaferon. Aflubin is similar in action; a well-advertised product promises to help nursing mothers in the fight against viruses. Traditional therapists are reluctant to prescribe homeopathy, but such drugs are sold in pharmacies without a prescription, so a woman’s desire to improve her health will be enough to purchase.
Sore throat
To treat signs of inflammation of the oropharynx, it is recommended to use topical medications. For breastfeeding women, the safest options are rinse solutions that contain antiseptic components. Solutions of Hexoral, Chlorhexidine, and Iodinol have the most pronounced effect.
You can also make your own gargling solution at home. To do this, dissolve one teaspoon of table or sea salt in one glass of boiled warm water, add three drops of iodine. You need to gargle with the prepared solution 4 times a day.
To relieve pain, experts recommend sucking special lozenges, for example, Strepsils or Sebidin. Another very safe method of treating sore throat is considered to be irrigating the oropharynx with special antiseptic sprays, for example, “Kameton”, “Chlorophyllipt”, “Camphomen”.
Before using any drug, be sure to consult your doctor. The fact is that self-medication can cause the development of the most unpredictable complications for the health of the child and mother.
Development of allergies during lactation
Despite the severe stress on the body endured by a woman during childbirth, the causes of allergies remain the same as in a normal period of life.
Causes and symptoms
The main reasons include the following categories:
Household factors. A common category of allergens found in everyday life. Animal hair, dust, fragrances, detergents, and cosmetic products act as irritants. Food and drinks. Absolutely every ingredient can cause a rash on the body, redness or itching during the postpartum period. You should not introduce unknown foods into your diet during the guard period, or eat or drink potentially dangerous foods - seafood, chocolate, citrus fruits, honey. Medicines. If a nursing woman uses new drugs during lactation, it is not known whether she will develop an allergy to them. It is necessary to read the composition of the medicines and, if unnecessary components are identified, postpone such a medicine until cessation of lactation
Take all appropriate medications after consulting a doctor and with extreme caution. Biological group of allergens. A woman’s immunity during hepatitis B, affected by infectious diseases or a virus, develops protective functions by killing dead cells
At this time, allergies may become more active. Physical influence from outside. The scorching sun, dry air, and cold are potential sources of danger for a person suffering from allergies.
The symptoms of allergies during lactation are also not very different from the symptoms of any allergy sufferer. They can be divided into several groups:
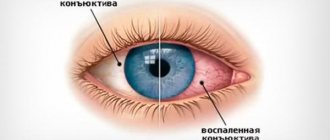
- Respiratory symptoms - allergens include pollen and dust. Unpleasant itching in the nasopharynx, runny nose, frequent sneezing, dry cough. Sudden onset of symptoms is usually seasonal. With constant anxiety, asthma or chronic rhinitis may develop, in which there is no fever, but if complications occur, Quincke's syndrome may develop and resuscitation will be required.
- Symptoms of gastrointestinal disorder - arise from an allergic reaction to foods. Stomach cramps, intestinal disorders, nausea and vomiting.
- Manifestations on the skin - a rash all over the body, and can be detected in both the mother and the baby. If an allergenic ingredient is consumed in excess, the particles penetrate into the mother's milk, and with it the baby, which, in turn, can cause a rash, diaper rash or seborrhea on the scalp. The most serious consequences occur with atopic dermatitis in a baby. In this case, allergies can be treated at home, but with a diet without carbohydrates and the use of antihistamines.
The causes and symptoms of allergies in a nursing mother are not very different from those for any allergy sufferer.
Specifics of allergies during the period of guarding
Women during pregnancy and lactation are already considered to be at risk, and mothers with high blood pressure, concomitant kidney diseases and edema during pregnancy are the first to suffer. When breastfeeding, all reactions that occurred before childbirth intensify several times, just as the list of allergens increases. If the allergy takes the mother by surprise, then a similar reaction will obviously appear in the child. Considering the specificity of allergic reactions during hepatitis B, it is possible to treat the disease only with certain approved medications.
Traditional medicine recipes
Many mothers who breastfeed their babies do not want to use pharmaceutical drugs to treat ARVI, but the viral disease provokes poor health. How to relieve symptoms in this case? To do this, you can use folk remedies therapy. For inhalations, you can use decoctions made from chamomile and calendula. But please note that under no circumstances should you inhale if a nursing mother has a fever.
The use of herbal teas and decoctions allows you to continue breastfeeding. Experts give the following recommendations for the treatment of ARVI in nursing mothers at home using traditional methods:
- Be sure to use herbal infusions. Licorice, sage, and St. John's wort can thin phlegm, soften the throat, and also have an excellent expectorant effect.
- Natural honey is a universal antibacterial agent. Before using it for therapy, you should make sure that there is no allergic reaction to bee products. Butter, boiled milk, a teaspoon of natural honey and a pinch of soda will be an effective remedy for a sore throat and dry cough.
- Use essential oils for inhalation. It will be especially useful to breathe in steam that contains notes of juniper and eucalyptus.
- Garlic has a good general strengthening effect.
- To bring down the heat, you can use raspberry jam.
- Tea with the addition of viburnum is very effective for coughs.
Before choosing traditional medicine recipes for ARVI treatment, be sure to ask your doctor for recommendations, as there may be contraindications to the use of such methods.
Folk remedies
Komarovsky believes that the most harmless and simple methods of treating colds in women while breastfeeding are folk recipes. The following remedies can be prepared at home:
- It is necessary to cut the radish into slices, sprinkle with sugar and bake in the oven for 2 hours. The resulting juice should be taken 10 ml every 3 hours and before bedtime. This remedy has an anti-inflammatory effect and helps to quickly cope with the disease.
- It is necessary to pour a tablespoon of thyme into 200 ml of boiling water and leave for several hours to infuse. This product is recommended for gargling a sore throat.
- If you have a strong cough, it is recommended to breathe over boiled potatoes for 15-20 minutes, adding a little baking soda. To do this, bend over the pan and cover your head with a towel, after mashing the potatoes.
- You can first chop the onion or garlic and mix it with honey. This remedy should be taken 1-2 teaspoons after each meal during a cold. However, it should be remembered that such products have a specific odor and can cause allergies in infants.
You can get rid of a sore throat with:
- curd compress;
- warm milk with honey and butter;
- rinsing with fresh beet juice and vinegar.
If a cold is accompanied by profuse nasal discharge, it is recommended:
- instill aloe juice mixed with a drop of honey or a mummy tablet into the nasal passages;
- lubricate the nasal cavity with lemon juice;
- breathe over a plate of freshly chopped onions;
- instill a mixture of onion or garlic juice with honey into the nose in a 1:1 ratio.
Essential oils that can be used for inhalation are considered a good assistant in the fight against colds. It is necessary to drop a few drops of eucalyptus into boiling water and insert a cardboard funnel into the spout of the kettle. With the help of such inhalations, it is possible to clear the airways of accumulated mucus, cope with a runny nose and eliminate pain in the throat.
Preventing your baby from the cold virus
ARVI is a common condition characterized by the entry of pathogens into the human body, that is, adenoviruses, as a result of which swelling of the nasal mucosa begins to develop, a sore throat, general weakness, malaise, and an increase in body temperature.
ARVI during breastfeeding in a woman is considered a problem of significant importance, which is explained by the high risk of infecting the child. In this case, there is no single panacea to protect the baby, but any nursing mother can use a number of measures for these purposes that can reduce the risk of possible infection. These baby precautions against ARVI while breastfeeding include:
- Under no circumstances should you stop breastfeeding your baby. This condition is mandatory, because along with breast milk, immunoglobulins enter the child’s body, which form the immune system and also act as a barrier to infection.
- Regular hand washing. The fact is that the spread of infection can occur not only through airborne droplets, but also through contact. Particles of mucus from the nose can get onto a nursing mother's hands through a handkerchief. These secretions contain a huge number of ARVI pathogens. An important condition for preventing infection with this disease is mandatory hand washing before contacting a child.
- Using a protective mask. Using a protective cellulose or gauze bandage will not provide a 100% chance of protecting your baby from infection, but this method can significantly help reduce the concentration of the virus in the surrounding air.
- When ARVI develops in a mother while breastfeeding, her general condition can significantly worsen. As a rule, this is accompanied by increased body temperature, weakness, and increased drowsiness. In such situations, women should involve their loved ones as well as relatives in the process of caring for the child, thus reducing the risk of infection.
How to treat a cold for a nursing mother
When breastfeeding, a woman is selected for medications that do not contain harmful components.
Antiviral drugs
Antiviral drugs can be used to combat acute respiratory infections, however, many of them do not cope with their task due to only the psychological impact on a person. The following drugs are prohibited during lactation:
- Ribavirin;
- Arbidol;
- Remantadine.
For colds, homeopathic medicines can be prescribed, but their effectiveness is questionable. Among the medications in this group, names such as Aflubin, Anaferon and Oscillococcinum can be distinguished. Some medications contain alcohol, which can negatively affect the quality of mother's milk. In addition, homeopathic preparations contain herbal components, so they can cause allergies in the child.
For viral colds, medications that contain human interferon alpha are often prescribed. The most effective medications of this group are Viferon and Grippferon. Antiviral drugs are recommended to be used at the very beginning of the pathology, when viruses are on the mucous membranes. When the virus enters the mouth, antiviral drugs become ineffective and can interfere with recovery.
Antipyretics
With an increase in body temperature and fever, women during breastfeeding are allowed to take Paracetamol. If the baby is already 3 months old, then it is possible to bring down the temperature with the help of Nurofen. Such medicines help not only get rid of fever, but also eliminate headaches.
Important! During lactation it is not recommended to use analgesics, as they have a negative effect on the functioning of the child’s central nervous system. Acetylsalicylic acid, which can cause metabolic disorders in the female body, is also prohibited.
In addition, it affects the liver cells of the child’s body and increases the permeability of the vascular walls.
Remedies for runny nose
When you have a cold, it is best to treat a runny nose with plant-based drops, for example, Pinosol. In addition, sprays containing sea water are also suitable for this purpose. If a woman has severe congestion, she can use drops that have a vasoconstrictor effect. During breastfeeding, the following medications can be used to treat a runny nose:
- Salin;
- Nazivin;
- Tizin;
- Farmazolin.
It should be remembered that such drugs can cause addiction, so under no circumstances should they be used for a long time. Medicines such as Pinosol and Vitaon not only help get rid of a runny nose, but also have an antimicrobial effect. You can speed up the flow of mucus from the nasal passages using a product such as Aquamaris.
Throat treatment
It is possible to cope with painful sensations in the throat during breastfeeding with the help of local antiseptics. At home, it is recommended to rinse with pharmaceutical products or solutions prepared independently. A solution of furatsilin or soda, as well as Iodinol, Hexoral and Ingalipt, have a good effect in fighting the disease. A solution of sea salt with the addition of a few drops of iodine has a positive effect on the throat.
It is possible to temporarily reduce a sore throat with the help of lozenges such as Sebidin and Strepsils. Medicines in the form of sprays have a local effect and do not pass into breast milk. When treating a throat during breastfeeding, you can use drugs such as Cameton, Camphomen and Chlorophyllipt.
Cough medicines
The choice of one or another cough medicine depends on its type. In order to thin and remove mucus from the respiratory tract, products based on herbal components may be prescribed. The most effective are syrups containing ivy, thyme, licorice and marshmallow.
During lactation, inhalations with a drug such as Ambroxol can be performed. It affects only the mucous membrane of the respiratory tract and does not enter the systemic circulation. The following medications will help your mother’s cough:
- Bronchicum;
- Ambroxol;
- Gedelix;
- Overslept.
If a cold causes the development of various complications, the woman may be prescribed antibacterial drugs. During breastfeeding, medications from the penicillin group, macrolides and cephalosporins are allowed.