The development of a child up to one year occurs rapidly: every day brings something new. The baby sits down, begins to crawl, stands on his feet... finally takes the first step. There is no limit to the parents' delight and tenderness. However, sometimes, soon after this joyful event, it becomes clear that not everything is in order with the gait: the child places his legs in a strange way, or limps, or waddles when walking. What is this? And this is most likely a manifestation of hip dysplasia.
Hip dysplasia (DHS), or congenital subluxation of the hip joint, is the underdevelopment (or abnormal development) of the joint itself or its components: the acetabulum of the pelvic bone, cartilage, ligaments and muscles that hold the femur in the correct position.
When the joint is underdeveloped, the correct contact between the head of the femur and the notch for it (the acetabulum in the pelvic bone) is disrupted or absent. Manifestations of such pathology are sometimes difficult for parents to identify at a child’s early age. The initial diagnosis of this congenital pathology is carried out immediately after the birth of the baby, which helps prevent its serious consequences that develop with late detection.
In the absence of contact between the femur and pelvic bones, the femur can move freely outside the joint. This condition is called joint dislocation, or dislocation. There are 2 subtypes of dislocation: teratological and typical.
Teratological develops in utero due to genetic diseases or anomalies in the development of muscle tissue. It is rare. A typical dislocation is characterized by existing contact between two bones, but it is incomplete and unstable. This developmental pathology is the most common and can occur both in utero and after birth in healthy newborns.
Subluxation is a less severe condition: the contact between the bones is within normal limits, but the joint is unstable and the femur is easily separated from the acetabulum.
Reasons for the development of pathology
The hip joint or hip joint is large and mobile, its deformation leads to mobility impairments, but dysplasia is not a deformity, but a congenital dislocation, subluxation, pre-luxation of the joint.
The pathology is common, but can be corrected successfully if diagnosed in a timely manner. The causes of hip dysplasia in newborns are as follows:
- Difficult labor, breech presentation, large fetus.
- Low water intake, calcium deficiency in a pregnant woman, convulsions, kidney pathologies in the mother.
- Pathologies of the uterus, fibroids, adhesions - disrupt the motor activity of the fetus.
- Strong pressure on the fetus, leading to deformation changes.
- Hereditary factor, the presence among relatives of persons with a similar pathology.
- Maternal diabetes mellitus, high weight, edema, history of bone diseases.
- Birth trauma, improper care of the baby in the first days/months of life.
It is difficult to say why the disease developed, the reasons vary in specificity. The reason for this can be careless actions of doctors, difficult labor, or bad heredity.
Orthopedists do not determine the cause of dysplasia, since it does not affect the course of treatment. When a hereditary factor is to blame, the disease can occur in several children in the family.
There is nothing wrong with this, the condition is subject to correction, timely consultation with a doctor, and undergoing a routine examination will help identify DTS in the early stages of development. An orthopedist will help compensate for the baby’s condition and normalize motor activity.
Causes
The true cause of pathological development or underdevelopment of the joint is not fully known.
Predisposing factors are:
- genetic predisposition (usually in the female line);
- female gender of the baby (80% of all cases of dysplasia);
- hormonal levels: excess progesterone in a woman before childbirth can contribute to underdevelopment of the ligamentous-muscular system;
- incorrect position of the fetus in the uterine cavity, limiting the normal mobility of the child;
- large size of the fetus, which limits its movement and prevents the development of the joint;
- harmful factors, especially in the early stages of pregnancy (ecology, toxicosis, maternal illness, vitamin deficiency, etc.);
- prematurity: fetal tissue does not have time to mature.
Symptoms of the disease
Describing the clinical picture of DTS, it is worth saying that some manifestations can be observed in children in the first year of life. They are classified as developmental features, without indicating pathologies.
Description of the symptoms of the disease:
- the main feature is considered to be asymmetry of the folds and buttocks;
- pay attention to the limbs, with DTS one is shorter than the other;
- legs bent at the knees cannot be fully separated;
- movements are accompanied by silk, occurs in the knee, hip joint;
- an additional femoral fold appears.
The main signs of the disease are assessed collectively. The baby must have several symptoms; one is not considered a reason for making a diagnosis.
Symptoms are assessed during a routine examination. If the doctor cannot separate the legs of a small patient, he sees other manifestations of DTS and refers him for an ultrasound examination.
Diagnostic tests
Diagnostics takes place in several stages and has the following focus:
- Helps make a diagnosis.
- Classify pathology.
- Prescribe treatment and correct the patient’s condition.
Diagnostics takes place in stages and consists of conducting an examination and procedures aimed at clarifying the extent of changes affecting the joint tissue:
| Inspection | Helps the doctor to correct the set of symptoms and identify violations. They are carried out as planned, if there are indications, they are done at 3,6,12 months. The earlier pathological changes can be identified, the easier it is to correct them. |
| Ultrasound | Ultrasound is considered a routine examination, a screening test that helps identify developmental disorders. An ultrasound is performed in the direction of an orthopedist or pediatrician. When there are no indications, the study is considered planned; if there is, it is considered diagnostic. The procedure is safe, painless, ultrasound is required to monitor the effectiveness of therapy when treatment is carried out. |
| Radiography | When an ultrasound shows changes in the joint, an x-ray is prescribed. The examination is informative because it visualizes the joint and changes. Based on the images, the doctor makes a diagnosis and prescribes treatment. X-rays are not prescribed for children in the first three months of life. |
The baby can be diagnosed in the maternity hospital if they do an ultrasound. A pediatrician who is present at the birth and examines the newborn after completion of labor or cesarean section can suspect DTS.
Ultrasound screening examination, carried out to exclude the presence of pathologies, is planned, prescribed, carried out without indications, harmless, painless. It does not cause any discomfort, the procedure lasts five to seven minutes.
An orthopedist can diagnose a patient without additional research, based on the totality of symptoms. Prescribe treatment, register the baby, making recommendations.
Parents will have to follow the instructions, not violate or interrupt treatment, otherwise the results will be poor.
DTS classification
There are three stages of disease development:
| Pre-luxation | It manifests itself as underdevelopment of the head of the femur, without displacement, relative to the glenoid cavity. |
| Subluxation | Underdevelopment of the head of the femur, with slight displacement relative to the socket of the joint. |
| Dislocation | Underdevelopment of the head of the femoral bone, occurring with complete displacement relative to the glenoid cavity. |
A congenital hip dislocation is considered severe. Changes more often affect one side; bilateral hip dysplasia is less common. In girls, DTS is diagnosed five times more often than in boys.
Diagnostics
To confirm a diagnosis suspected by a doctor during examination of a child, the following are used:
- Ultrasound (in the first half of the baby’s life);
- X-ray examination (after 6 months, since at an earlier age the skeletal system is underdeveloped and consists of cartilage, which is difficult to record on an x-ray).
Additional examination is necessary to identify DTS, since sometimes even an experienced doctor can make a mistake. So, according to statistics, pediatricians suspect this joint pathology in 8.6 cases out of 1000, orthopedic doctors - in 11.6 cases, and ultrasound reveals abnormalities in the structure of the joints in 25 children out of 1000.
Ultrasound is the prevailing method for diagnosing hip joint pathology in the first months of a baby’s life: it is more informative than a simple medical examination, painless, and does not expose to radiation. The study makes it possible to see the clear shape of the socket of the pelvic bone, which is of great importance in the development of dysplasia.
It makes no sense to conduct an ultrasound before 4 weeks of a newborn’s life, because some changes in the structure of the hip joint disappear on their own, without treatment, during the first month of life.
Symptoms of DTS that can be identified using additional examination methods:
- flattening or deformation of the acetabulum of the pelvic bone;
- underdevelopment of the head of the femur or cartilage;
- excessive stretching of the joint capsule or ligamentous apparatus;
- incorrect angle of the femur;
- partial (or complete) protrusion of the femur from the acetabulum.
Condition correction methods
Hip dysplasia in children is corrected as follows:
- treatment involves the use of devices;
- the orthopedist recommends massage and gymnastics;
- Physiotherapy is practiced.
Preference is given to an integrated approach, several correction methods are combined, and the dynamics are monitored.
| Adaptations | Pavlik's stirrups, Frank's pillow, splints are designed to hold the child's legs in a certain position, apart. Wide swaddling is practiced, the diaper is attached to the legs, it keeps the limbs apart. The choice of device is made by the doctor. Pavlik's stirrups are considered gentle. Children tolerate treatment well. The duration of therapy depends on the stage; the devices will have to be used for several months, up to a year. Splints help keep the legs apart; the selection of the device is carried out individually. |
| Massage, gymnastics | A set of procedures helps enhance the treatment chosen by the orthopedic surgeon. Massage is given as a course, and you can do gymnastics on your own. The doctor will show you what exercises to do. |
| Physiotherapy | Orthopedists prescribe a course of electrophoresis, with calcium, to the thigh area. |
When treatment does not produce results, the child is not provided with timely assistance and surgery is required. The intervention is performed under general anesthesia; after the operation, a recovery period begins, the duration of which is difficult to determine.
Attention!
The operation will help restore motor activity, the result is difficult to predict, and often surgical correction is the only way out of this situation.
The operation is performed if there are indications; the feasibility of the procedure is determined by the orthopedist monitoring the patient.
How is dysplasia determined in newborns?
Only a doctor can make an accurate diagnosis, but there are certain symptoms that should prompt parents to immediately consult a specialist and understand what it is. Symptoms appear either all together or separately in newborns.
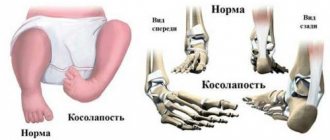
Photo of joint dysplasia
- Asymmetrical folds - lying on its back with straight legs, the cub should have symmetrical folds on the inside of the thigh, and lying on its stomach - symmetrical folds on the bottom.
- The abduction of the legs in a bent state is less than 85-90°; only one of the legs can be abducted with limitation, or both can be. Moreover, no effort is required; the flexibility of healthy joints in newborns allows this procedure to be easily performed.
- A crunching sound is heard when the hips are spread apart or when they are brought together.
If you detect any suspicion of developmental discrepancy in newborns, you should not postpone a visit to an orthopedist, especially when you know what hip dysplasia in children is. If necessary, the doctor prescribes an ultrasound or x-ray, and then he will accurately indicate the presence or absence of pathology.
Treatment of dysplasia in newborns
If the diagnosis is confirmed after examination and examination by a specialist, treatment measures are prescribed depending on the stage of hip dysplasia. This can be wide swaddling, gymnastics, massage, swimming on the stomach, electrophoresis with calcium, in more pronounced forms - wearing Pavlik stirrups, Freik pillows. If the first procedures do not cause any particular difficulties, then orthopedic devices worry both parents and children.
Photos of treatment of hip dysplasia in newborns
It must be remembered that small children quickly get used to such devices, although at first, of course, they cause a little discomfort, and if used correctly they will give a quick positive effect. Some mothers remove splints without the doctor’s knowledge, thereby reducing the effectiveness of treatment. In addition, with dysplasia, it is under no circumstances allowed to stand the baby on its legs; this can only aggravate the dislocation.
Also read: Foot fungus in children, causes and treatment
Prevention of dysplasia in newborns
It is known that in areas where there is no tight swaddling of babies, the percentage of hip dysplasia is much lower, so for the normal development of babies, doctors recommend either not swaddling them at all, or using wide swaddling. And in a calm state, the child should be in a natural position, i.e. with legs bent at the knees and in a spread position.
Photo of a child
The main thing that parents should remember is that dysplasia is not a death sentence, or even a disease, but for a healthy and happy life for the child in the future, it is necessary to identify the pathology in time, leave aside your fears and correctly correct the development of the baby. Knowing what hip dysplasia is in a newborn, you can contact a specialist in a timely manner and take action. The health of children's feet directly depends on the attentiveness of parents.
Complications of DTS
The consequences of hip dysplasia depend on the stage of development of the disease; orthopedists talk about the following complications:
- Gait disturbance caused by shortening of one limb.
- A decrease in motor activity occurs against the background of problems with movement associated with underdevelopment of the vehicle.
- Severe cases of dysplasia are characterized by impaired movement. The child cannot stand up or walk without crutches. It is difficult to tolerate hiking over short distances.
Babies with this diagnosis begin to walk later. But there is no need to rush; the diligence of parents and the desire to put the child “on his feet” will lead to consequences. The deformity will begin to progress and complications will arise.
Timely treatment, following the recommendations of an orthopedist, and conducting routine examinations will help you avoid the consequences.
Prevention
There are no measures that can prevent the development of the disease. There are measures that will help diagnose DTS at an early stage of development:
- after discharge from the maternity hospital, it is worth undergoing an examination, visiting an orthopedist who will examine the patient and diagnose pathological changes;
- during pregnancy, take vitamins, calcium supplements, under the supervision of a gynecologist, you can use complex vitamins;
- during the first year of life, do an ultrasound of the vehicle, show the results to the doctor, ultrasound will help identify changes;
- study diseases of the genus, identifying the tendency to pathologies in the unborn;
- Throughout your life you will have to monitor the condition of the head of the vehicle, periodically visiting an orthopedist and doing an ultrasound.
Mothers should examine the baby and monitor the stages of development. When the folds on the legs are asymmetrical, it is worth showing the baby to an orthopedist. Often parents notice a problem when the baby begins to crawl and walk. Noting movement disorders, problems with coordination.
A consultation with an orthopedist will help solve the problem and compensate for the condition. It is more difficult to treat a child of this age. The correction will be incomplete because the head of the femur is deformed.
Do not swaddle the baby tightly, stretching his legs and securing him with a diaper. Tight swaddling increases the risk of developing dysplasia, research has proven.
The best prevention of DTS is monitoring the condition of the newborn, tracking the stages of development, timely visits to doctors, even in the absence of complaints.
A disease such as hip dysplasia is considered common, is often diagnosed in children, and can be successfully corrected without the use of medications. The treatment is long, not always pleasant, but brings results. Timely treatment helps to completely eliminate defects and normalize the child’s motor activity.
Hip dysplasia
According to statistics, parents of three out of a hundred newborn babies face a similar problem. Doctors use the term “dysplasia” to mean congenital underdevelopment of a joint, which leads to disruption of its function and, in the most severe cases, can cause chronic hip dislocation.
Such a disease, if left untreated, does not end well. Impaired function of the lower limb, gait, pain in the hip joints and a high risk of disability are the consequences of advanced dysplasia. Therefore, all parents need to know the first symptoms of this disease and understand the importance of timely visits to an orthopedist. Early diagnosis and proper treatment will help avoid complications. Remember, the earlier the diagnosis is made, the more favorable the prognosis will be!
There is still no consensus among experts regarding the development of hip dysplasia in children. According to one version, the main reason is a malformation of articular tissues in the early stages of pregnancy (the first 2-3 months). This is predisposed by unfavorable ecology, exposure to toxic substances and some infectious diseases.
According to another theory, the development of joints is affected by high levels of oxytocin, the hormone that causes the onset of labor. Accumulating towards the third trimester, oxytocin increases the tone of the fetal femoral muscles, as a result of which subluxation of the hip joints gradually develops. Perhaps this is the reason for the greater prevalence of dysplasia among girls (5 times more often than boys), who are more susceptible to the influence of the mother’s hormonal levels.
The risk is also increased by incorrect intrauterine position of the fetus and prolonged difficult labor (in the breech position).
The tendency to dysplasia is often inherited, so if one of your relatives has already had such cases, you need to think about early diagnosis in advance.
Parents themselves may suspect something is wrong, even before consulting an orthopedist. Most often this occurs in severe forms of the disease, when the head of the femur completely comes out of the socket. In milder cases, only a specialist can determine the presence of dysplasia, since subluxation and pre-luxation of the hip joint practically do not manifest themselves externally. However, there are main signs:
- limited mobility (spreading) of the hips; often the baby begins to cry when trying to move the leg to the side;
- asymmetry (mismatch) of the inguinal and gluteal folds, which become more pronounced on the damaged side.
But the presence of only these symptoms in hip dysplasia in a child is not an absolute sign of the disease and may be a consequence of impaired muscle tone.
In the event of a dislocation, the hip joint practically loses its function, and the affected leg is shortened. A “clicking symptom” occurs - the head of the femur slips from the surface of the joint when the child’s legs are bent at the knee and hip joints, as well as its reduction when they are separated.
If dysplasia was not diagnosed in the first 6 months of life after childbirth, then the damage to the joint progresses - the limb shortens even more, a pathological (“duck”) gait or intermittent claudication (with bilateral dislocation) is formed.
Diagnosis of dysplasia is often carried out in the maternity hospital. If this does not happen (recently, ultrasounds are done only if there are problems), then parents can ask the pediatrician to conduct an examination themselves. It is safe for the baby’s health and guarantees high accuracy of diagnosis.
However, if a single ultrasound showed normal development of the joints, still do not forget about constant monitoring by an orthopedist. Routine examinations will help your child avoid possible problems.
The first visit to the orthopedist should take place no later than 1 month, at which time a mandatory ultrasound of the hip joint is performed. This is an indispensable condition for the early diagnosis of dysplasia. A repeat examination is carried out at the end of the 3rd, beginning of the 4th month, at which time the doctor may recommend taking an x-ray. The most difficult to diagnose is subluxation of the hip joint, which practically does not manifest itself at all and can only be seen on an x-ray.
Take preventive observation with an orthopedist seriously - the timing of the examination is not appointed by chance, each of them is associated with an important stage in child development. So, if dysplasia was detected in the first 3 months of the baby’s life, then after a course of treatment the functionality of the joint is completely restored (usually by 6-8 months), and there are no long-term consequences.
The younger the child, the easier it is to treat dysplasia. For example, in babies up to 3 months old, the joint can recover on its own, provided that the children's legs are always in the right position. That is why the main method of treatment in the early stages of the disease is free swaddling, in which the baby’s legs are spread apart. At the age of 3 months, the abducted position of the legs is achieved by using the Freik pillow (Photo 1), selected according to the child’s size. The later treatment is started, the more serious orthopedic devices are used; at 6 months the Mirzoeva splint (Photo 2) or Pavlik stirrups (Photo 3) are already used.
| Photo 1. Freyka's pillow | Photo 2. Shina Mirzoeva | Photo 3. Pavlik stirrups |
In this regard, the experience of Asian and African countries is interesting, where mothers traditionally carry their babies on their stomachs or behind their backs most of the time and do not swaddle them. Cases of dysplasia are rare here, because the joints are provided with ideal conditions for normal development. On the other hand, in European countries it is customary to swaddle newborns quite tightly (pressing the legs together) - in this position, even the mildest forms of joint underdevelopment can lead to the formation of dysplasia.
Doctors believe that loose swaddling not only allows the dislocation to correct itself at an early stage, but also stimulates further development of the joints, preventing the occurrence of complications. The point of free swaddling is that the baby's legs should be in an open position at all times, but at the same time have sufficient freedom of movement. The easiest way to achieve this is with a wide diaper and disposable diapers: after putting a clean diaper on the child, a thick diaper is placed on top of it, folded into a wide ribbon - so that the baby cannot move his legs together. The small patient should be in this position 24 hours a day. Often, the doctor adds to this a course of therapeutic massage and daily gymnastics (including abductor-circular movements in the hip joints). In most cases of mild forms (subluxation, preluxation with slight displacement of the femoral head), such treatment is sufficient.
But if treatment and prevention were not carried out in the first 3 months of life, then more serious and long-term treatment will be required for a complete recovery. The danger of unrecognized dysplasia is that the baby’s bones, due to age, are very flexible and susceptible to various deformations. The baby’s skeleton is constantly growing, but this same factor also explains his greater tendency to developmental defects. Most joints (including the hip) in the first months of life consist mainly of cartilage tissue, and any disturbances in the connection of the bones lead to the formation of serious deformities. To stop the progression of the disease, it is necessary to return all parts of the joint to their normal position. For this, various types of abductor splints (listed above) are usually used; they hold the baby’s legs in the desired position. After some time, the joint gradually “fixes” and begins to develop correctly.
At the age of 2-3 months, small patients with suspected dysplasia are usually not given x-rays, since even with an unconfirmed diagnosis it is customary to prescribe a preventive course of treatment: the use of soft spreading splints, a course of therapeutic exercises (with abductor-circular movements) and massage of the gluteal muscles . Splinting and massage work well with physical therapy techniques to speed up recovery.
When using spreading splints, remember that their design should not interfere with the free movements of the baby’s legs, otherwise the effectiveness of treatment will be reduced. The retaining structure cannot be removed without the doctor’s permission; the fixed position of the joints must be maintained at all times. In case of mild forms of the disease, the spreading splint is put on the baby only while sleeping. The decision to stop treatment is made by the doctor based on the results of several x-ray studies and the disappearance of symptoms.
If, after 2-4 weeks of treatment, spontaneous reduction of the dislocation does not occur, but complete relaxation of the femoral muscles is achieved, a more rigid fixation is prescribed in combination with constant traction. To do this, apply a plaster cast, which allows you to keep the child’s hip joints completely apart and bent at a right angle. This treatment is resorted to in cases of severe forms or late diagnosis of dysplasia, when milder methods are no longer effective. Therefore, once again I would like to draw the attention of parents to the importance of early examination: if dysplasia is detected in the first 3 months, complete restoration of the hip joints in 95% of children is achieved within 3-6 months of treatment.
For many, such long-term treatment seems difficult and tiring; often parents try to find more effective methods and... make a mistake. Gentle step-by-step treatment for an infant turns out to be much more effective and, of course, more gentle than the use of one-stage closed reduction of a dislocation under anesthesia, which can sometimes lead to severe complications.
By the end of the first year of life, all babies again undergo a routine examination by an orthopedist. Then several groups are conventionally distinguished:
- children with dysplasia who have not received any treatment;
- children with severe, poorly correctable forms of dysplasia;
- babies with residual symptoms of dysplasia.
Each child, if necessary, is prescribed further treatment - conservative (massage, gymnastics, physiotherapy) or surgical intervention. If the diagnosis of “irreducible dislocation” is confirmed, then surgery is necessary - open reduction of the joint under anesthesia.
If the dislocation can be corrected using conservative methods, surgery is not performed on the joint, but sometimes extra-articular surgery is required to help secure (stabilize) the joint. Most often, such interventions are carried out in children over 3 years old, when the child’s body tolerates anesthesia more easily. But surgical treatment of the joint itself should be carried out as early as possible! Therefore, the formation of the joint is considered optimal by 12-13 months, when the baby begins to walk.