Causes
The main reasons why the disease can develop are identified:
- congenital pathology associated with the inheritance of a pathological gene formed in an autosomal dominant manner;
- pathology of the cornea - a thorn, malnutrition through blood vessels, erosions, ulcers, inflammatory process;
- pathology of the lens - clouding of the internal structure, coloboma;
- postoperative complications that cause various pathologies of the cornea and lens (most often, astigmatism develops due to improper suturing);
- mechanical damage to the eyeball, which leads to its deformation (penetrating injury, scar formation), this results in improper passage of the beam through the internal structures of the eye.
The doctor must not only identify the disease, but also establish the root cause. If this is not done, relapse is possible after treatment.
Factors predisposing to farsightedness
Farsightedness in a child can be caused by one or several factors, which, in combination with the individual characteristics of the structure and functioning of the visual analyzer, lead to this disorder.
Heredity
If at least one of the parents has a so-called refractive error (farsightedness, nearsightedness, astigmatism), then most likely the child has all the prerequisites for its development.
Presbyopia (age-related farsightedness), which appears after 45 years, cannot be considered a hereditary factor, since its appearance is associated with age-related weakening of the muscles that change the shape and position of the lens, and initial changes in the structure - clouding, changes in density, and the appearance of a vacuole.
Ecology and medications used during pregnancy
Any chemical compounds directly or indirectly affect the development of a child in the prenatal period. This does not mean that you should stop taking your medications to maintain your health or immediately move to another place.
It’s just that in some cases we don’t always know what kind of water flows from our tap and what kind of air we breathe. Therefore, we cannot predict how this will affect the child.
High visual load
In cases of mild farsightedness, the body is able to try to cope on its own by changing the position of the main lens of the eye - the crystalline lens. However, increased visual stress causes muscle fatigue and leads to the progression of hypermetropia.
Risk group
Most often, the disease develops in children who have been exposed to the following factors:
- born prematurely;
- children whose one or both parents suffer from an ophthalmological disease, especially astigmatism;
- infants who, during the mother's pregnancy, were exposed to intrauterine infection, lack of nutrients, and hypoxia;
- children who have undergone surgery or mechanical damage to the eyes;
- patients who have a history of inflammatory disease of any structure of the eyeball.
Parents of children who have been exposed should undergo periodic examinations by an ophthalmologist to ensure early detection of the disease and treatment.
Classification
Depending on the age at which the disease manifested itself, it is divided into:
- congenital form;
- acquired form.
Depending on the degree of visual distortion and changes in the shape of the eyeball, 3 degrees of the disease are distinguished:
- weak up to 3 diopters;
- average from 3 to 6 diopters;
- high from 6 and above diopters.
Depending on the clinical manifestations, the disease is divided into 3 categories:
- Simple form. A ray of light, refracted in optical media, is partially projected on the retina and partially scattered on it. One meridian is preserved, astigmatism is poorly developed.
- Complex shape. Two meridians passing through optical media have impaired refraction, but their severity is different. The scattering of light is in front of the retina.
- Mixed form. This is the most complex disease that is difficult to treat. The patient has several focal lines, one of which is projected in front of the retina, and the second behind it. Therefore, one meridian is myopic, and the second is hypermetropic.
To classify the disease, the doctor needs to perform a series of diagnostic tests.
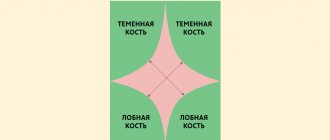
Types of astigmatism
Children's astigmatism is divided into several types, which reflect the nature of the manifestation, refractive changes, and the location of the focusing elements.
The main types are divided according to the damage to the meridians into:
- Simple.
- Difficult.
- Mixed.
Simple and complex astigmatism is divided into:
- Hypermetropic. It is characterized by a predominance of farsightedness, in which the focus of the object is formed outside the retina.
- Myopic. The opposite of hypermetropic. Occurs with myopia.
According to the nature of the damage, astigmatism is divided into two types:
- Corneal: Caused by defects in the corneal structures. It greatly affects the child’s visual acuity, since the cornea has a greater refractive power than the lens.
- Lens: occurs when the shape of the lens body changes.
Recommends reading the article about the classification of astigmatism.
Symptoms
A patient with the disease develops characteristic clinical symptoms:
- manifestation of symptoms in early childhood;
- farsightedness, that is, the child sees well in the distance, but poorly near;
- if the child has astigmatism of no more than 0.5 diopters, there is no discomfort for the visual organs;
- children complain of insufficient vision function;
- there is a feeling of a foreign body under the eyelids;
- if a child strains his eyes, he develops a headache and severe fatigue;
- impaired perception of the shape of objects;
- Double vision is less common.
If the diagnosis based on clinical symptoms is not made correctly, the child will experience increased eye pain and headaches when wearing an optical device.
Gymnastics for the eyes
Daily eye exercises are another component of health. The task of looking at distant and close objects with both eyes, one eye at a time, will become a method of training the brain to receive a normal image, as well as a game. This will help with astigmatism in a child aged one and a half years or more. But if the child is older, additional measures are necessary.
Diagnostics
To determine the child’s condition, you need to contact an ophthalmologist who will conduct a series of studies. Parents can determine the presence of astigmatism at home, but the true cause can only be identified after examination by a doctor using special devices.
Research in the clinic
Diagnostics include:
- Parent survey. The doctor will find out how often the child falls and whether he orients himself normally in space. If the child is over 4-5 years old, he may complain of a headache.
- Examination of the child. Visually no changes can appear. However, when examining nearby objects, the child may squint to see them better.
- The use of diagnostic tables that depict pictures or letters. The doctor sequentially points to each symbol, the child must identify it. The more he sees them, the better the quality of his vision.
- Duochrome study. The child must view the diagnostic table using lenses of different colors. If astigmatism is present, viewing in the green spectrum will impair his vision function.
- Biomicroscopy. This is an intravital study of the cellular composition of the surface layer of the eye. The doctor can determine or rule out the possibility of a disorder in the cellular composition of the anterior pole of the eye. The patient may develop scales on the lower edge of the eyelids, affecting the shape of the eye.
- Computer keratotopography. The technique determines the curvature of the cornea and the degree of refraction of light rays. If the cause of astigmatism is pathologies of the cornea, the doctor determines in which area there are distortions of its tissues.
- Measuring corneal thickness. If it becomes excessively thin, the patient may be diagnosed with keratoconus.
Based on all the data received, the doctor makes a reliable diagnosis, determines the root cause of the disease, and only then begins treatment.
Tests at home
Before going to the doctor, parents can check for the presence or absence of astigmatism in their child using home tests. Some of these studies can be repeated by an ophthalmologist:
- Application of diagnostic tables. They can be downloaded from the Internet or printed on a printer.
- Snellen figure. In another way, this test is called radiant figure. It can be downloaded and printed on a printer. The child must carefully examine the image. The figure contains parallel lines that form a point in the center. If your child has astigmatism, these lines may become distorted. The center point may be off to the side or completely absent.
- Raubichek's arrow. The image shows a circle, inside of which there are two hyperbolas, whose shape resembles an arrow. If a child has astigmatism, the figure may be blurred in all elements except the apex of the arrow.
- Duochrome test. You will need a printed ophthalmology chart for this. Parents will also need glasses with red and green lenses. With astigmatism, the patient sees letters well in the red spectrum, but poorly in the green spectrum.
With the data obtained, parents can contact their doctor for treatment.
Possible consequences of the disease
Astigmatism that is not treated promptly can lead to lazy eye syndrome, or strabismus. In 20 cases out of 100, there will be a permanent deterioration in vision in one or both eyes, up to complete loss of vision.
Lazy eye is the loss of the brain's ability to combine visual input from the eyes to produce a clear picture. Most often, attempts to cover, squint one eye, noticeable headaches, dizziness, and nausea are added to the existing symptoms.
Treatment consists of two parts: stopping further processes of loss of vision clarity, restorative therapy.
Strabismus is not just a cosmetic defect. Behind it is the lack of three-dimensional vision, systemic deterioration of vision in both eyes, and almost always a sharp decrease in image quality in the squinting eye. Treatment includes different techniques, depending on the type of disease:
Treatment
Treatment for the patient’s condition depends on the type of astigmatism, the number of diopters for farsightedness, and the severity of clinical symptoms. Until the age of 4, you can only use glasses for vision correction. This method is suitable for mild to moderate grades. If the child has a high degree, it is necessary to use spherical and toric lenses for glasses.
Once the eyeballs are fully formed, surgical or laser treatment can begin.
Arcuate keratotomy
The doctor preliminarily measures the meridians, identifying the altered ones. On the opposite side of it, small arc-shaped incisions are made on the cornea. As a result of these actions, a protrusion and a change in the focal line are formed. The number and depth of the incisions made depends on the data obtained during the examination of the cornea.
Photorefractive keratectomy
An excimer laser is used to remove corneal tissue at the required depth. During therapy, surrounding tissues are not damaged. The technique is suitable for mild astigmatism.
Laser keratomileusis
A special microkeratome device is used. It is used to create a flap on the cornea. A bed is formed, which is processed with a laser. The extracted flap is placed on top. The procedure is suitable for children with mild to moderate astigmatism.
Implantation of an intraocular lens
The technique is suitable for children whose astigmatism develops due to the development of cataracts. The pathological formation is first removed and an intraocular lens is installed in its place. It expands in the capsular bag and is localized in the same place where the lens was. It is identical in function to it. The device is made of hypoallergenic material to which the immune system does not react.
We recommend reading: Toric intraocular lenses
Laser correction
Laser vision correction is carried out using an excimer laser. This device operates in the ultraviolet part of the spectrum. By evaporating small areas of the cornea, the laser allows you to change its profile, which can successfully combat myopia, farsightedness and astigmatism.
If the doctor removes sections of the cornea in the central zone, it becomes flatter, which corrects myopia. Laser work along the periphery increases the sphericity of the cornea. Thus, farsightedness is corrected. Removing sections of the cornea in different areas allows you to successfully combat astigmatism.
The operation of the laser is controlled by a computer using a special program, so the accuracy of ablation (evaporation) of the desired areas is very high.
Laser correction of astigmatism is not performed on persons under 18 years of age, pregnant women, and patients suffering from degenerative diseases or pathologies of the body's immune system.
Laser correction leads to improved vision, but like surgical intervention, it is permissible only after 18. Before this age, eye growth and development still occur. You can wear glasses from an age when a child can consciously wear them and not play with them.
So it will be impossible for a 2-year-old child to put on glasses, and after much effort the parents will have to abandon this idea.
Prevention
Congenital astigmatism cannot be prevented. But you can eliminate the possibility of its development using the following methods:
- classes for the child only in a well-lit room;
- when standing or sitting, the child should keep his back straight, his head should look only forward, but not down;
- proper nutrition with the intake of all useful substances into the body; if this is not enough, it is necessary to use multivitamin preparations;
- timely visit to the ophthalmologist with all diagnostic tests for timely detection of the disease.
If a child has a congenital form of astigmatism, or it appeared in early childhood, the pathology can gradually worsen the quality of vision. Therefore, it is recommended to undergo an annual examination by an ophthalmologist and use the prescribed treatment.